![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
91 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What are the two geographical influences on parasitic infections?
|
Local ecology
Local socioeconomic conditions |
|
|
|
That are the types of alveolates?
|
Dinoflagellates
Apicomplexa Ciliates |
|
|
|
What are the properties of alveolates?
|
Submembrane
Cytoskeleton has a fixed shape |
|
|
|
What is the bug that causes an invasive intestinal protozoal infection?
|
Entamoeba hystolytica
|
|
|
|
What is the bug that causes amoebic dysentary?
|
Entamoeba histolytica
|
|
|
|
What disease does entamoeba histolytica cause?
|
Amoebic dysentary
|
|
|
|
What are the kinds of bugs that cause a non-invasive intestinal protozoal disease?
|
Giardia lamblia
Cryptosporidia Cyclospora microsporidia |
|
|
|
Giardia lamblia belongs to what class of parasite?
|
Diflagella
|
|
|
|
Cryptosporidia and cyclospora are members of what classes of parasites?
|
Apicomplexa
|
|
|
|
What are the characteristic symptoms of non-invasive intestinal protozoal infections?
|
Watery diarrhea
Weight loss |
|
|
|
What is the general life cycle of an intestinal protozoa?
|
1. Ingestion of a cyst
2. Cyst--gastric acid--> Trophozoite 3. Trophozoite forms inside the intestine 4. Near end of GI tract trophozoites-->cysts 5. Excretion in the feces |
|
|
|
What is the mechanism of division for trophozoites?
|
Binary fission
|
|
|
|
What are the two life forms of E. histolytica?
|
Trophozoite (1 nuclei)
Cyst (4 nuclei) |
|
|
|
What type of cell is commonly ingested by E. hystolytica? What form ingests the cells?
|
RBCs
Trophozoites |
|
|
|
What is the reservoir for E. histolytica?
|
Humans
|
|
|
|
What are the key virulence factors of E. histolytica?
|
Amebic lectin
Amoebapores Cystine protease |
|
|
|
What is the function of amebic lectin in this parasite?
|
E. hystolytica
Binds to galactose-containing sugars on host cells Adherence |
|
|
|
What is the function of amoebapores in this parasite?
|
E. histolytica
Performs cytolysis on adhered cells |
|
|
|
What is the function of the cystine protease in this paracite?
|
E. hystolytica
Cleavage of preIL-1B -->Il-!b Results in the mounting of a host inflammatory response |
|
|
|
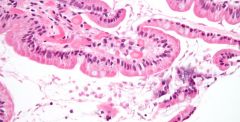
Histologically, what does mucosa infected by E. hystolytica resemble?
|
An iceberg: the area of damage under the surface is larger than the damage above
|
|
|
|
With E. hystolytica, what does the stool appear like
|
Low volume
Bloody |
|
|
|
What are the intestinal syndromes of an infection by E. hystolytica?
|
Anywhere inbetween:
Asymptomatic Chronic diarrhea Amebic dysentery (similar to shigella) |
|
|
|
What are the extraintestinal clinical syndromes of an infection by E. histolytica?
|

Amebic liver abscesses
Metastatic foci to the brain |
|
|
|
How does one diagnose an infection by E. histolytica?
|
Stool sample: ID of trophozoites/cysts
Stool antigen tests Serology |
|
|
|
What are the two types of Entomoeba?
|
histolytica: disease causing, invasive
dispar: non-pathogenic; shouldn't be treated |
|
|
|
What is the treatment for E. histolytica
|
Metronidazole
|
|
|
|
Where does the excystation of G. lamblia occur?
|
Upper small intestine
|
|
|
|
Histologically, what does G. lamblia cause? What is the overall effect of this change?
|
Killing off of the villi in the duodenum-->hypersensitivity
Malabsorption of fats |
|
|
|
What are the clinical features of giardia?
|
Chronid diarrhea
Malabsorption Steatorrhea Weight loss |
|
|
|
What is the most effective way to diagnose an infection with G. lamblia?
|
Antigen testing from stool.
|
|
|
|
What antibiotics are used to treat Giardia?
|
Metronidazole
Tinidazole |
|
|
|
How is Giardiasis prevented?
|
Filtering the water
Heading the water to 50C 2% iodine x 30 min |
|
|
|
What two protozoa stain with the acid fast stain?
|
Cryptosporidium
Cyclospora |
|
|
|
Where do cryptosporidium, cyclospora, and microsporidia grow?
|
Inside intestinal mucosal cells
|
|
|
|
What diseases is Cryptosporidium parvum associated with?
|
Travelers diarrhea
Chronic diarrhea in immunocompromised patients |
|
|
|
Where is a place that a person would normally acquire Cryptosporidium parvum? Why there?
|
Pools, drinking water
They're Cl resistant |
|
|
|
What is the treatment for cryptosporidosis?
|
Supportive!
No real treatment |
|
|
|
What is the difference between cyclospora and cryptosporidium?
|
Cyclospora is much smaller.
|
|
|
|
What is the treatment for cyclospora? Would the treatment change in an immunocompromised individual?
|
Bactram for 7 days.
Yes; you need to give them antivirals in order for treatment to be effective. |
|
|
|
What are some of the apicomplexa tht cause a systemic protozoal infection?
|
Plasmodium
Babesiosis Toxoplasmosis |
|
|
|
What are the dinoflagellates that cause a systemic protozoal infection?
|
Leishmania
Trypanosomes |
|
|
|
What is the disease that Plasmodium species cause?
|
Malaria
|
|
|
|
What disease is caused by T. gondii?
|
Toxoplasmosis
|
|
|
|
What symptoms are common to malaria and babesiosis?
|
RBC infection
Fever |
|
|
|
What is common about the method of infection by toxoplasmosis and leishmani?
|
The bugs are intracellular
|
|
|
|
How do bugs in the apicomplexa move?
|
LIKE A TANK!
|
|
|
|
How does apicomplexa enter the cell?
|
Through a little ring of its own making
|
|
|
|
What is unique about an apicomplexa/parasitophorous vacuole?
|
No host proteins
No acidification No endosomal/phagosomal fusion It's invisible |
|
|
|
What is typical animal associated with a toxoplasma infection?
|
Cats and kitty litter
|
|
|
|
What is a place that a toxoplasma infection will first localize too?
|
Intestinal cells --> mesenteric nodes
|
|
|
|
How long can a toxoplasmosis cyst persist?
|
Decades - they're periodically released.
|
|
|
|
What are some serious clinical syndromes associated with toxoplasmosis?
|
Acute acquired toxoplasmosis
Congenital toxoplasmosis: what does this appear like? Ocular toxoplasmosis Cerebral toxoplasmosis (in AIDS - the worst kind) |
Blueberry muffin lesions
|
|
|
What type of patient are we most concerned about for toxoplasmosis?
|
Pregnant women - the parasite can go into newborns.
|
|
|
|
What tests are useful for a diagnosis of toxoplasmosis?
|
Serology:
+IgG: prior infection Single high IgM/IgG: recent in fection PCR: useful only if + |
|
|
|
If a woman has toxoplasmosis earlier in pregnancy does the baby have a greater or lesser chance of infection? Is it more/less serious?
|
Lesser chance of infection
BUT Much more serious for the baby |
|
|
|
Where is the first place of localization for malaria?
|
Liver
|
|
|
|
What is the type of plasmodium that are injected into the blood by mosquitos?
|
Sporozoites
|
|
|
|
What kind of plasmodium are released from the liver to infect the blood?
|
Merozoites
|
|
|
|
What is the kind of plasmodium that is found within a RBC?
|
Trophozoites
This is what is picked up by the mosquitos |
|
|
|
What kinds of plasmodium are released by a lysis of RbCs
|
merozoites
|
|
|
|
Where does sexual reproduction of plasmodium take place?
|
Inside the gut of a mosquito.
|
|
|
|
How long after infection by plasmodium do symptoms start to show?
|
10 days - 1 month
|
|
|
|
What is a large aggregation of merozoites called? Where are thy found?
|

Schizont
Inside hepatocytes, RBCs |
|
|
|
What is the main RBC receptor for Plasmodium falciparum?
|
Glycophorin
|
|
|
|
What is the RBC receptor for Plasmodium vivax? What group does not have this on their RBCs?
|
Duffy blood group
People from Africa; resist malaria from thei bug |
|
|
|
What is the energy source for Plamodium? What problem does this cause for the organism?
|
Consumption of hemglobin within RBC's
Heme toxicity. It needs to export the heme, which is a process that is targeted by the cloroquinones. |
|
|
|
What toxic byproduct is put in these aggregates by plasmodium?
|
Heme
Hemozoin - brownish pigment deposits |
|
|
|
What histologic feature is diagnostic of a merozoite?
|
Ring form within RBC
|
|
|
|
What is the most serious kind of plasmodium? Why?
|
Falciparum.
Because it is able to attack all types of red cells, not just young/old like the others. |
|
|
|
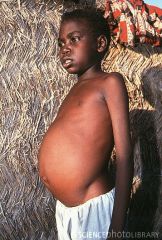
What is the difference between stable and unstable malaria?
|
Stable: endemic. Kids die of it; adults have immunity. Splenomegaly common.
Unstable: not endemic; all ages die. |
|
|
|
What are the clinical features of malaria?
|
Synchronous fevers caused by the RBC's releasing merozoites:
5 hrs.: fever, myalgia, headache, GI problems. 2 hrs: sweating, exhaustion |
|
|
|
What are the immunologically-mediated hematologic clinical changes in plasmodium?
|
Anemia
Thrombocytopenia Leukopenia |
|
|
|
What are secondary problems to infection by plasmodium falciparum?
|
Attachment of infected RBCs to venular endothelial cells via ICAM, etc. -->> reduced flow; hemorrhage
|
|
|
|
What genetic disease provides protection from malaria?
|
Sickle cell anemia
|
|
|
|
What tests are most effective in the diagnosis of malaria?
|
Microscopy
Rapid antigen detetion |
|
|
|
What histologic features are diagnostic of p. falciparum?
|
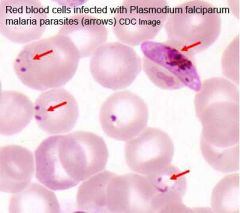
Ring forms
Multiple bugs/cell Banana shaped gametocytes |
|
|
|
What is the treatment for malaria?
|
Chloroquinones (blocks heme polymerization; falciparum is resistant)
Quinine + doxy Primaquine: vivax and ovale |
|
|
|
What is the mechanism of chloroquinone?
|
Changes the pH inside of the malrial vacule, preventing the polymerization of heme Toxicity.
|
|
|
|
What is the mechanism of resistance to chloroquinone by this bug?
|
P. falciparum
Efflux of chloroquinone by an amino acid transporter. |
|
|
|
What are the current malaria prevention strategies?
|
Mosquito control: insecticides, habitat removal
Mosquito protection: nets, screens Mass tx: get rid of carriers. |
|
|
|
What is the vector for babesois?
|
Ticks
|
|
|
|
What is the pathology of babeosis?
|
RBC lysis in asplenic/elderly
|
|
|
|
What is the geographic local of babeiosis?
|
Same as lyme disease - transmitted by ticks.
|
|
|
|
What is the vector for leishmaniasis?
|
Sand flies
|
|
|
|
What are the symptoms of infection by leishmania?
|

Skin ulcers - if bug grows at colder tempreatures
|
|
|
|
Where do leishmania live inside the body?
|
Phagolysosmes inside of macrophages
|
|
|
|
What kinds of leishmania grow inside the body?
|
L. donovani
L. infantum/chagasi |
|
|
|
What internal organs do the intracellular leishmania parasites target?
|
Think of the filtration of the body:
Liver Spllen Lymph nodes |
|
|
|
What are the symptoms of a systemic leichmania infection?
|
Fever
Malaise Weight loss Abdominal pain Pancytopenia, increased LFTs |
|
|
|
Why is an infection by P. falciprum more serious than the others?
|
Merozoites enter RBCs of any age
Parasitemias reach very high levels Infected RBCs (containing trophozoites and schizonts )stick to the sides of vascular endothelium, causing microinfarcts and hemorrhage |
|
|
|
What are the symptoms of acute toxoplasmosis?
|
Myalgia
Swollen Lymph noodes Symptoms may last for a long time - over a month. |
|

