![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
74 Cards in this Set
- Front
- Back
|
Puerperium
|
Puerperium: termination of pregnancy to a pre-pregnant state.
*Extends for 6 weeks after delivery. |
|
|
Uterus
Involution of the uterus Process #1 |
1.Autolysis of some of the protein cells of the uterine wall.
Uterine muscle proteins -> broken down into simple compounds ->absorbed -> eliminated in the urine. -size of the individual myometrial cells decrease. The increase in the total number of uterine cells from pregnancy is permanent. The increase in connective tissue and elastin in the myometrium, as well as the blood vessels is also permanent. |
|
|
Uterus
Involution of the uterus Process #2 (Regeneration of the endometrium) |
Regeneration of the endometrium
The endometrium is restored to its pre-pregnant state by the end of the 3rd week. A layer of granulation tissue is formed which divides the endometrium into two layers: - Superficial layer cast off as "Lochia". - Inner layer composed of connective tissue and uterine glands -> regenerates the endometrium. |
|
|
Uterus
Involution of the uterus Process #2 |
This granulation layer serves as a
protective barrier against infection. EXCEPTION: The placenta site takes 6 weeks to regenerate by a process known as Exfoliation. - An undermining of the placental site by the upward growth of endometrial tissue from the basal layer. - Unique healing process - Forms no scar - Enables the endometrium to resume its usual cyclic changes. - Permits implantation and placentation in future pregnancies. |
|
|
Uterus
Involution of the uterus Process #3 (Contractions of the uterus) |
myometrium remain contracted in the early postpartum period to minimize blood loss.
first hour postpartum ->postpartum hemorrhage is most likely to occur. The body produces systemic oxytocin which acts on the smooth muscles causing contractions. |
|
|
Uterus
Involution of the uterus Process #3 |
Uterus weighs:
-2 pounds after delivery -1 pound after one week -12 oz after the 2nd week -2 oz after 6 weeks |
|
|
Fundus - Top of the uterus
(location) |
After delivery of the placenta=the fundus is 2 cm below the umbilicus (U/2).
One hour after delivery = fundus rises to the level of the umbilicus (U/U) or 1 cm above the umbilicus (1/U). The fundus remains at this location for 12 hours, then it descends @ 1 - 2 cms every 24 hours. By the 9th day postpartum, the fundus no longer palpable. |
|
|
Fundus
(Risk factors of a hypotonic uterus?) |
Risk factors of a hypotonic uterus:
- Over-distended uterus - Rapid labor - Prolonged labor - Nulliparity - Prolonged general anesthesia - Pregnancy Induced Hypertension (PIH) |
|
|
Lochia
(defination?) |
Lochia - A vaginal discharge that persists throughout most of the postpartum period.
*Consists of blood from the uterine sinuses at the placental site and the necrotic superficial layer of the endometrium. |
|
|
Lochia
(three types?) |
Classified into three types:
1. Lochia Rubra 2. Lochia Serosa 3. Lochia Alba |
|
|
Postpartum: Menstruation
|
The menses returns within 6 - 8 weeks postpartum *if the mother does not breastfeed*,.
Breastfeeding mothers vary with the return of the menses. Nursing mother may not menstruate during the lactation period or the menses may occur the 2nd to 18 months after delivery. Ovulation is unpredictable! |
|
|
Postpartum:Perineum
|
Edematous after childbirth.
More pronounced within the first 24 hours after delivery. Episiotomy: incision of the perineum to enlarge the vaginal opening for baby delivery |
|
|
Postpartum:Perineum
(Perineal lacerations) |
Extent of the laceration is defined on the basis of depth.
1.Extends through the skin and structures superficial to the muscles. 2.Extends through the muscles of the perineal body. 3.Continues through the anal sphincter. 4.Involves the anterior rectal wall. Those at risk for lacerations are those whose tissue is less capable of distension. - Heredity is a factor. - Rapid delivery. |
|
|
Postpartum:Vagina
|
Recovers from distention and decreases in size, but never quite to the nullipara state.
Very smooth at first -> rugae reappear by the 4th week. Tone is regained by the 6 week. Local dryness and coital(sexual intercourse) discomfort may persist until ovulation and the menses resume. |
|
|
Postpartum:Mammary Glands
|
The breasts begin to secrete colostrum midway through pregnancy.
If no colostrum, doesn't mean client is incapable of milk production. The size of the breasts do not an indicator of its functional capacity. After delivery, no change is noted in the breasts for two days. -Colostrum continues to be secreted in small amounts until lactation begins. On the 3rd or 4th day, milk secretion begins. Breasts become larger, firmer, and more tender. -Veins more prominent. -Breasts feel heavier. -May have a burning or prickling sensation -> Secretion from the nipples changes from yellow to -bluish-white. |
|
|
Postpartum:Milk Production
|
-The hormone Prolactin stimulates milk production.
-Initially, high levels of prolactin are secreted after the delivery of the placenta. |
|
|
Postpartum:Milk Production
(SUCKING STIMULUS) |
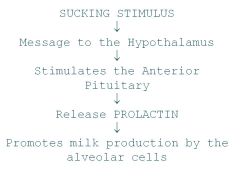
|
|
|
Milk Secretion
|
Frequent and complete emptying of the breasts is
necessary for milk secretion to continue. If the breasts are not emptied regularly -> Prolactin secretion is not stimulated -> milk production decreases and eventually ceases. Other factors that influence milk production: - Mother's diet - Fluid intake - Activity level/Rest -Milk production is inhibited by full breasts. -Milk production is dependent on the quantity of milk removal. -The more and more milk that is suckled -> Larger quantity is produced. |
|
|
Process of Let Down
|
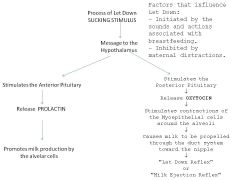
|
|
|
Postpartum:Vital Signs
|
Temperature
First 24 hours may be elevated to 100.4 Infection if: - Temperature > 100.4 - After the first 24 hours The third or fourth day temperature may be r/t ? Pulse -Bradycardia common the first 6-8 days postpartum -Pulse 50-70/minute considered normal. (Returns to normal within 3 months) -Tachycardia is r/t blood loss. Blood Pressure: Unchanged Hypotension indicates uterine bleeding. Orthostatic hypotension common first 48 hours. |
|
|
Postpartum:Circulatory system
|
Cardiac output continues to be elevated for up to 48 hours postpartum.
-Returns to the pre-pregnant level within 2-3 weeks The blood volume has returned to its pre-pregnant level within 4weeks after delivery. -The decrease in blood volume and decrease in fluid retention is r/t the decrease in progesterone and other placental hormones. Varicosities of the legs regress (abnormally or markedly swollen or dilated). |
|
|
Postpartum:Circulatory system
(Laboratory values) |
Leukocytosis(increase WBC) often occurs the first 10-12 days postpartum.(20,000 - 25,000 is considered normal).
Blood loss averages: Vaginal delivery: 200–500 mL C/Section: 700 – 1000 mL Hemoglobin and Hematocrit levels vary -First 72 hours after delivery there is a greater loss of plasma volume than blood cells -> increases in Hgb and HCT. -Low hemoglobin levels are r/t anemia. |
|
|
Renal System
|
Diuresis(increased excretion of urine) begins within 12 hours after delivery.
Ureters begin to shrink. Bladder fills quickly. Glucosuria is common. |
|
|
Renal System:
(Factors depressing urination) |
1.Trauma to the urethra and bladder as the infant passes
through the pelvis. 2.Edema of the urethra and urinary meatus. 3.Effects of anesthesia. 4.Pelvic soreness. 5.Vaginal lacerations /episiotomy. |
|
|
Gastrointestinal System
|
Digestive tract functions normally after a vaginal delivery.
May be a slight intestinal slow down from medications or hormones of pregnancy. |
|
|
Gastrointestinal System:(Bowel Function)
|
Spontaneous BM delayed for several days r/t:
- Decrease in muscle tone in the intestines. - Pre-labor diarrhea. - Lack of food/Dehydration. - Perineal tenderness. Stool softeners given to prevent constipation. Hemorrhoids that developed during pregnancy or during delivery regress. |
|
|
Integumentary System
|
-Pigmentary changes that developed during pregnancy either regress or disappear.
-Striae gravidarum become lighter in color. -Diaphoresis can occur during the first few days postpartum, esp. at night as the body rids itself of retained fluids from pregnancy. -Hair loss occurs. -Nails return to their pre-pregnant state. |
|
|
Abdominal wall
|
-Immediately after delivery, the abd is flat, soft, and flabby.
-When client stands upright, the abd muscles can not retain the abd contents -> Abd protrudes -> "still pregnant appearance". -Minimum of 6 weeks is needed for the abd wall to regain its muscle tone. |
|
|
Weight loss
|
At delivery @ 12 pounds.
During the first 2 weeks after delivery @ 9 pounds. Takes @ 6 weeks or more to return to their former wt. |
|
|
PSYCHOLOGICAL CHANGES
(Three Phases of Maternal Adjustment) |
1. Dependent phase "Taking In"
2.Dependent - Independent phase "Taking Hold" 3.Interdependent phase "Letting-Go" |
|
|
NURSING CARE OF THE POSTPARTUM CLIENT
(Delivery room) |
First two hours most critical.
- Initial readjustment to a non-pregnant state. - Body systems are stabilized Supine position for 1-2 hours, head elevated 45 . -No BRP r/t orthostatic hypotension. |
|
|
NURSING CARE OF THE POSTPARTUM CLIENT
(Delivery room) Assessment |
Monitor for hemorrhage q 15 minutes the first hour and q 30 minutes the second hour.
- Palpate fundus for firmness and location. - Note Lochia. - Assess vital signs. |
|
|
NURSING CARE OF THE POSTPARTUM CLIENT
(Delivery room) Interventions |
-Warm blankets for the intense chill-like tremors.
-Clear liquids in small amounts, drink slowly. Pain management: - Ice packs to perineum to decrease edema and numb area. - Analgesics |
|
|
NURSING CARE OF THE POSTPARTUM CLIENT
(Postpartum Unit) Assessment |
- Fundus
- Lochia - Vital signs - Voiding |
|
|
NURSING CARE OF THE POSTPARTUM CLIENT
(Postpartum Unit) |
Assist to BR the first time and STAY WITH CLIENT!)
(Have spirits of ammonia ready!) Instruct on peri care: - Peri bottle - Wipe (pat) front to back - Change pad every time Episiotomy care -Analgesics for pain Education - Cold packs for the first 12 hours. - After 12 hours -> Sitz baths. - Topicals: - Tucks pads - Anesthetic sprays-Dermoplast - Creams/Ointments - Kegel exercises |
|
|
NURSING CARE OF THE POSTPARTUM CLIENT
(Postpartum Unit) Hemorrhoidal care |
Hemorrhoidal care: Education
- Sitz baths - Topicals: - Tucks pads - Creams/Ointments |
|
|
NURSING CARE OF THE POSTPARTUM CLIENT
(Postpartum Unit) Breast care:Non-lactating |
Non-lactating
Educate client to: -Wash breasts daily with fresh wash cloth. - Wear a snug bra - Do not express milk from breasts. - Moderate amount of fluid intake. - If tender:Ice packs to breasts, Breast binder, and analgesics. - Avoid hot water on breasts. |
|
|
NURSING CARE OF THE POSTPARTUM CLIENT
(Postpartum Unit) Breast care:Breastfeeding |
Educate client to:
-Wash nipples daily with water - Leave colostrum on the nipple after feeding and let nipples air dry. - Wear a well fitted nursing bra, with broad shoulder straps. |
|
|
NURSING CARE OF THE POSTPARTUM CLIENT
Breastfeeding:sore nipples |
If client c/o sore nipples:
- Check position of infant's on areola. - Check the infant's sucking activity. - Check how the infant is removed from the breast. - Suggest client not use breasts as a pacifier. - Remind client to rotate positions from feeding to feeding. - Remind client to air dry nipples. - Can shorten the time infant is on each breast, and nurse more frequently. - Last resort: Creams (without alcohol). |
|
|
NURSING CARE OF THE POSTPARTUM CLIENT
Breastfeeding:foods to avoid |
Educate client on foods to avoid while nursing:
- Spicy foods - Gas-forming foods - Caffeine |
|
|
NURSING CARE OF THE POSTPARTUM CLIENT
Breastfeeding:engorged breasts |
Educate client on engorged breasts:
- Use warm compresses 15 - 20 minutes before breastfeeding - Warm shower. - Client may need to express some milk from the breasts to decrease the fullness to enable the baby to latch on to the breasts. - Prevention best. Inform clients to continue their prenatal vitamins for as long as they are breastfeeding. Monitor the medications client is taking. Refer to La Leche league. |
|
|
NURSING CARE OF THE POSTPARTUM CLIENT
Diet Medications |
Diet: Regular
Medications: - Stool softeners - Laxatives - Analgesics - RhoGam - given within 72 hours after delivery to prevent Rh Isoimmunization. - Rubella vaccine if non-immune. Encourage sibling visits Monitor parents/newborn interactions. |
|
|
NURSING CARE OF THE POSTPARTUM CLIENT
Discharge instructions |
Discharge instructions
- Rest as much as possible- Lochia will increase with activity. - Can resume intercourse when bleeding has stopped and episiotomy healed - Most MD's prefer clients to wait until 6 week check up. - Prenatal vitamins: --Breastfeeding - Continue while nursing. --Non-lactating - Finish prescription. - Elimination problems - Stool softeners if prescribed - Laxative MOM, or other MD preference. - Exercise - Roughage in diet - Adequate fluid intake |
|
|
Summary of postpartum nursing care
(10 B's) |
*Boggy Belly
*Bleeding *Bottom *Bladder *Bowels *Breasts *Bonding *Blood type *Blues *Birth Control |
|
|
Summary of postpartum nursing care
(BUBBLE-HE) |
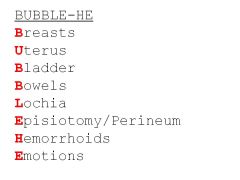
|
|
|
Infant Abduction
|
Common characteristics on an abductor:
- Female of childbearing age (12-50), often overweight. - Emotionally immature and compulsive. - Frequently has lost a baby or is incapable of having one. - Often married or cohabiting; companion's desire for a child may motivate the abduction. - Considers the baby her own once abduction occurs. - Usually lives in the community where the abduction occurs. - Often visits the nursery and asks detailed questions about hospital procedures and layout. - Usually plans abduction but does not necessarily target a particular infant. - Frequently impersonates a nurse or other hospital personnel. - Often acquainted with hospital personnel or the victim's |
|
|
Nurse's role in prevent abductions
|
- Know the characteristics on an infant abductor.
- Know who's on the unit. - Be alert for strange behavior. - Educate parents starting prenatally: -- Don't leave baby unattended. -- Ask identification of someone they don't know. |
|
|
Rh Isoimmunization
|
-A hemolytic disease arising from incompatibility of the Rh factors of maternal and fetal blood.
-RESULT OF AN ANTIGEN - ANTIBODY REACTION -Sensitization usually occurs when an Rh- women delivers an Rh+ baby -> Fetal erythrocytes enter maternal circulation -> Mother forms antibodies to the Rh+ complex of antigens. -With subsequent pregnancies of Rh+ fetuses -> Rh antibodies from sensitized woman's circulation crosses the placenta and enters fetal circulation -> causes hemolysis of the fetal RBCs-> Fetal anemia-> brain damage-> death. |
|
|
Rh Isoimmunization #2
|
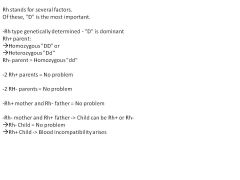
|
|
|
RhoGam: A immunoglobulin solution containing Rh (D) antibodies
|

|
|
|
Prenatal Blood work: Blood Type
|
Sensitization via Indirect Coombs test.
(Indirect Coombs test detects the presence of free circulating antibodies in serum: Anti RH antibodies). Prenatally at *28 weeks Rh- mothers given RhoGam* IM prophylactically. |
|
|
RhoGam given within 72 hours after delivery to RH- women who meets the following criteria:
|
|
|
|
POSTPARTUM HEMORRHAGE
(Late) |
•Most frequently caused by retained placental fragments.
•Develops a day or two after delivery. •Occasionally placental fragments are retained for a week or longer -> They become necrosed and fibrin may be deposited ->"Placental Polyp" fragment formed-> sloughing of the polyp-> sudden bleeding. oDx:- Boggy uterus - Large amount of vaginal bleeding - + HCG oManagement - Prevention best by careful examination of the placenta for any missing pieces. - D&C - Control bleeding with medications:(IV Oxytocin & Methergine) - Antibiotics. |
|
|
POSTPARTUM HEMORRHAGE
(Early)Cause |
Four causes:
- Uterine Atony. - Lacerations of the genital tract. - Retained placental fragments. - Blood coagulation problems. Management of uterine atony: Hemabate (Prostin 15M) given IM for postpartum hemorrhage not responding to conventional management. |
|
|
POSTPARTUM HEMORRHAGE
(Early)Retained Placenta |
Retained Placenta
•Hemorrhage occurs if the placenta is only partially separated r/t massage of the fundus prior to placenta separation. •Management: Manual removal of the placenta and uterine massage. Rarely Placenta Accreta is the cause of early postpartum hemorrhage. •Placenta Accreta is an abnormal adherence of the placenta to the uterine wall •Management: D&C or emergency hysterectomy. |
|
|
Nursing care for Postpartum Hemorrhage
Interventions |
Interventions:
•Massage fundus until firm •Increase the IV rate (with Pitocin) •Express clots •Monitor for signs of anemia •Encourage rest •Education is extremely important: oNormal postpartum course. oSigns of abnormal bleeding |
|
|
Nursing care for Postpartum Hemorrhage
Periodic assessments |
Periodic assessments:
- Fundal height and firmness - Bleeding - Pad counts / weighing pads |
|
|
Nursing care for Postpartum Hemorrhage
(Ways of prevention) |
Ways of prevention:
- Fundal massage - Assessing fundal height and consistency. - Inspecting of episiotomy and lacerations |
|
|
Nursing care for Postpartum Hemorrhage
(Call MD if) |
- Excessive or bright red bleeding(Saturation of > one pad/hour).
- A boggy fundus that does not respond to massage. - Abnormal clots - Temperature > 100.4 - Any unusual pelvic or rectal discomfort or backache. |
|
|
POSTPARTUM INFECTIONS
(Predisposing factors) |
- Prolonged rupture of the membranes.
- Retained placental fragments - Postpartum hemorrhage - Pre-existing anemia - Prolonged or difficult labor with use of instruments |
|
|
POSTPARTUM INFECTIONS
(Types of infections) |
1.Thrombophlebitis
2.Perineum 3.Endometritis 4.Mastitis 5.UTI's |
|
|
ENDOMETRITIS
|
After expulsion of the placenta -> the placenta site is an excellent medium for bacterial growth.
|
|
|
ENDOMETRITIS:
Early signs and symptoms |
Early signs and symptoms (On the third or fourth day postpartum).
- Temperature 100.4 or >. Occurs on two successive days,not counting the first 24 hours after delivery. - General malaise. - Anorexia. - Chills. |
|
|
ENDOMETRITIS:
Later signs and symptoms |
- Perineal discomfort.
- Lower abd distress. - N/V. -----------> - Foul or profuse lochia. - Tachycardia. - Pelvic pain and tenderness. |
|
|
ENDOMETRITIS:
Management |
Management
- Antibiotics. - IV fluids. - Analgesics. |
|
|
ENDOMETRITIS:Nursing care
(Interventions & Prevention) |
Nursing care
Assessment: q 8 hours or BID for signs and symptoms of infection. Interventions - Encourage po fluids. - Place in semi fowlers position. - Maintain peri care. Prevention Educate client on the importance of peri care: - Wiping front -> back. - Changing pads after each void. - Thorough hand washing. Diet high in protein and vitamin C. |
|
|
MASTITIS
|
An inflammation of the breast.
Incidence: 1% if delivered women. Usually unilateral. Develops after the flow of milk has been established. Organism usually Staph. Aureus. *Most common source is infant's nose and throat. |
|
|
MASTITIS:Pathophysiology
|
1
|
|
|
MASTITIS:
Clinical manifestations |
Clinical manifestations of Mastitis:
- Chills - Fever - Malaise - Local breast tenderness in upper outer quadrant - Axillary lymph nodes enlarge and are tender |
|
|
MASTITIS: Management
|
Management
- Intensive antibiotic therapy x 10 days - Breast support - Local heat - Analgesics - Lactation maintained via breast pump (milk discarded). - Encourage fluid intake - If abscess develops -> I&D |
|
|
MASTITIS
Nursing care: Prevention |
Nursing care: Prevention
-Teach proper breastfeeding techniques to prevent cracked nipples. -Avoid milk stasis. -Proper hand washing. -Avoid tight clothing. -Support for breasts (bra) at all times. -Teach daily breast assessment and signs and symptoms of mastitis to report to MD. - If client finds one are of her breast feels distended: - Rotate baby's position for nursing - Manually express remaining milk if infant not sucking well. - Massage caked area toward the nipple as baby nurses. |
|
|
Urinary Tract Infections
|
r/t difficulty voiding due to vulvar edema and loss of bladder tone from pressure of fetal head or increased residual volume.
|
|
|
Urinary Tract Infections:
Management |
Management
- Broad spectrum antibiotic x 10 days. - Analgesics for painful urination. |
|
|
Urinary Tract Infections:
Nursing Care Interventions |
- Encourage fluids 3000 mL to 4000 mL/ day
- Provide rest - Encourage peri care - If breastfeeding and Tetracycline or Sulfonamides prescribed -> Have client pump breasts and discard milk. |

