![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
107 Cards in this Set
- Front
- Back
|
Fire safety:
RACE |
R-rescue
A-alarm C-confine E-extinguish |
|
|
Fire Safety:
PASS |
P-pull pin
A-aim at base of fire S-squeeze handle S-sweep side to side |
|
|
Fire Safety:
Extinguisher Type A |
common materials such as paper, wood, or most combustibles
|
|
|
Fire Safety:
Extinguisher Type B |
Flammable liquids like gasoline, paint remover, or grease
|
|
|
Fire Safety:
Extinguisher Type C |
electrical
|
|
|
Fire Safety:
Extinguisher Type D |
combustible metals usually found in industry
|
|
|
Order of Opperations during assessment:
Regular |
inspection
palpation percussion auscultation |
|
|
Order of Operations during assessment:
abdominal |
inspection
auscultation percussion palpation |
|
|
Herberden Nodes are an indication of
|
osteoarthritis
|
|
|
Melena
|
blood in stool
|
|
|
Snellen chart test
|
Right eye
Left eye Together |
|
|
4 Phases of Disaster
|
mitigation
preparedness response recovery |
|
|
Mitigation
|
prevention/reduction
|
|
|
preparedness
|
form plans
|
|
|
response
|
action
|
|
|
recovery
|
return to normalcy
|
|
|
Biological Warfare
|
anthrax
botulism Hemm. fever Plague smallpox tularemia |
|
|
Chemical Warfare
|
ionizing radiation
mustard gas phosgene sarin |
|
|
Triage: Red
|
emergent care
-trauma, chest pain |
|
|
Triage: Yellow
|
urgent
-fractures, fever, abd. pain |
|
|
Triage: Green
|
nonurgent
-local injuries |
|
|
Triage: Black
|
death
|
|
|
Removing PPE
|
gloves
mask (lower, upper strings) gown eyeware/cap |
|
|
Hand washing: Drying
|
fingertips to forearm
|
|
|
Blood Typing: A
|
A & O
|
|
|
Blood Typing: B
|
B & O
|
|
|
Blood Typing: O
|
O
|
|
|
Blood Typing: AB
|
A, B, O
|
|
|
Universal RBC donor
|
O Neg
|
|
|
Universal RBC recipiant
|
AB Positive
|
|
|
Should not tranfuse blood longer than ________ hours
|
4
|
|
|
Blood should be started within _______ minutes from the bloodbank
|
30
|
|
|
What to assess before blood transfusion?
|
VS s/p first 15 minutes and q HR s/p transfusion
|
|
|
Platelets can be administered __________
|
15-30 mins
|
|
|
Prophylaxis for transfusion reaction
|
Oral Benedryl/Tylenol 30 mins before or IV immediately before
|
|
|
Isotonic solution
|
0.9% NS
|
|
|
Change an IV catheter every ________hours and a CVL every ________ hours.
|
72
24 |
|
|
Blood/rapid fluids gauge needle
|
14, 16, 18, 19
|
|
|
Lipids gauge needle
|
20, 21
|
|
|
Standard IV fluids/clear IV meds gauge needle
|
22, 24
|
|
|
Older client gauge needle
|
21 or <
|
|
|
Microdrip
|
60 gtts
slow rate <100 mL/hr medium titration |
|
|
Macrodrip
|
thick solution
10/15/20 gtt/mL |
|
|
Flow Rate Formula
|
total volume X drop factor
_______________________________=gtts/min time in minutes |
|
|
Infusion Time Formula
|
total volume
_______________= time mL/hr |
|
|
Air Embolism Actions
|
clamp tubing
L side Trendelenburg trap air in R atrium contact doctor |
|
|
Hypertonic Solution
|
5% Dextrose in 0.45% NS
|
|
|
Parenteral Nutriion
|
-glucose so insulin can be added
-Hep. added; change solution 12-24 hrs -change tubing every 24 hours -therapeutic response 1-3 lb gain |
|
|
When a patient is on lipids, they must be checked every
|
10 minutes
|
|
|
3 Ps of Hyperglycemia
|
polydipsia
polyuria polyphagia |
|
|
Hypoglycemia
|
shakiness/weak
diaphoresis anxiety |
|
|
Normal body pH
|
7.40
|
|
|
Avoid taking Vit B6 with
|
Levodopa
|
|
|
Mg sulfate antidote
|
Ca gluconate
|
|
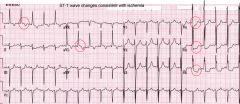
Ischemia on EKG
|
ST depression
|
|
|
L sided heart failure s/s
|
decrease UOP
dyspnea weight gain edema |
|
|
CVP pressure
|
7-12 cm H2O
|
|
|
If taking Epogen supplement with
|
Iron
Folic Acid |
|
|
If you have hypoparathyroidism supplement with
|
Vit D
Ca |
|
|
DKA blood glucose
|
>300
|
|
|
Gullian Barre
|
A disorder in which the body's immune system attacks part of the peripheral nervous system. The first symptoms of this disorder include weakness or tingling sensations in the legs spread to the arms and upper body. These symptoms can increase in intensity until the muscles cannot be used at all and the patient is almost totally paralyzed
|
|
|
Meniere's Disease
|
Meniere's disease is a disorder of the inner ear that causes spontaneous episodes of vertigo along with fluctuating hearing loss, ringing in the ear (tinnitus), and sometimes a feeling of fullness or pressure in your ear. In many cases, Meniere's disease affects only one ear
|
|
|
AIDS testing
|
2 positive ELISA
Western blot |
|
|
Atrial flutter
-sawtooth -atrial rate b/t 250-400 -absent T waves |
|
|
First signs of CRF
|
HTN
changes with urine |
|
|
Digoxin toxicity
|
Bradycardia
visual distrubances |
|

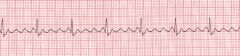
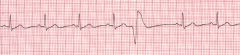
name this rhythm
|
normal sinus rhythm
-60-100 bpm |
|

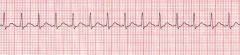
name this rhythm
|
sinus bradycardia
-<60 bpm |
|
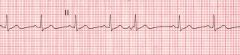
name this rhythm
|
sinus tachycardia
->100 bpm |
|
|
PR interval
|
0.12-0.20 seconds
|
|
|
QRS complex
|
0.12 seconds or less
|
|
Name this rhythm
|
Premature atrial contractions
-narrow QRS complexes -"skips a beat" |
|

Name this rhythm
|
Atrial fibrillation
-no P waves |
|
Name this rhythm
|
PVC
-no P wave -large T wave - T wave opposite of QRS complex |
|
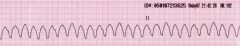
Name this rhythm
|
V Tach
|
|
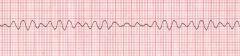
Name this rhythm
|
V Fib
|
|
|
QT interval
|
0.44 seconds or less
|
|
|
Square counting method for EKG
|
regular HR
-Count from first QRS complex to next QRS complex -300, 150, 100, 75, 60, 50 |
|
|
6 second method for EKG
|
irregular HR
-Count the number of QRS complexes that fit into 6 seconds -multiply by 10 |
|
|
If you have a prominent U wave suspect
|
hypokalemia
hypercalcemia hyperthyroidism |
|
|
Hyperkalemia EKG changes
|
prominent U wave
ST depression invertted T wave |
|
|
PR wave should be between 0.12-0.20, if not you have a
|
AV block
|
|
|
QRS should be less than 0.12 seconds, if not you have a
|
Bundle Branch block
|
|
|
MI is shown in an EKG as
|
ST segment elevation and not coming back to baseline (isoelectric)
|
|
|
Fahrenheit to Celsius
|
Degrees Fahrenheit – 32 × 5/9 = Degrees Celsius
|
|
|
Celsius to Fahrenheit
|
Degrees Celsius × 9/5 + 32 = Degrees Fahrenheit
|
|
|
Grading scale for pulses
|
• 4+ = strong and bounding
• 3+ = full pulse, increased • 2+ = normal, easily palpable • 1+ = weak, barely palpable • 0 = absent, not palpable |
|
|
HTN classifications
|
Prehypertension: a systolic BP of 120 to 139 mm Hg or a diastolic pressure of 80 to 89 mm Hg
Stage 1: a systolic BP between 140 and 159 mm Hg or a diastolic pressure of 90 to 99 mm Hg Stage 2: a systolic BP equal to or greater than 160 mm Hg or a diastolic pressure of 100 mm Hg or greater |
|
|
Radiography precautions
|
• Remove radiopaque objects such as jewelry.
• Ask the female client whether she is pregnant. • Inform the client that exposure to radiation is minimal and not dangerous. • Shield the client's abdomen and pelvic area. • Wears a lead apron if you stay in the room with the client. • After the radiograph, provide privacy for dressing or help the client dress as necessary |
|
|
Contrast dye precautions
|
• Determine whether the client is allergic to iodine, seafood, or radiopaque dye.
• Assess the client for any other allergies. • Inform the client of the possibility of throat irritation, flushing of the face, a sensation of warmth, or a salty taste during the test. • Encourage the consumption of fluids in the postprocedure period, unless this is contraindicated, and monitor urine output. • Assess the venipuncture site for bleeding. |
|
|
Thyroid scan precautions
|
• Before a thyroid scan, determine whether the client has received radiographic contrast agents within the past 3 months, which could invalidate scan results.
• Instruct the client to maintain nothing-by-mouth (NPO) status after midnight on the day of a thyroid scan. • No client preparation is necessary for needle aspiration of the thyroid |
|
|
Upper GI study precautions
|
• The client should not eat or drink after midnight before the day of the test.
• After the procedure, instruct the client to increase fluid intake to help pass the barium. • Monitor the stools for the passage of barium (evidenced by chalky whiteness), because barium can cause bowel obstruction. • A laxative may be prescribed if the client requires assistance in passing the barium |
|
|
Respiratory acidosis
|
In respiratory acidosis, potassium moves out of cells, producing hyperkalemia. Caused by any condition that obstructs the airway or depresses respiratory status
|
|
|
Respiratory alkalosis
|
In respiratory alkalosis, Hypokalemia, hypocalcemia, hyperreflexia, and seizures may develop. Any disease that increases metabolism
|
|
|
Metabolic acidosis
|
In metabolic acidosis, Kussmaul's respirations (deep and rapid) represent the body attempts to blow off the extra carbon dioxide and compensate for the acidosis
• Diabetes mellitus or diabetic ketoacidosis • Excessive ingestion of acetylsalicylic acid (aspirin) • High-fat diet • Insufficient metabolism of carbohydrates • Malnutrition • Renal insufficiency or failure • Severe diarrhea |
|
|
Metabolic alkalosis
|
• Diuretics
• Excessive vomiting or gastrointestinal suctioning • Hyperaldosteronism • Ingestion of excessive sodium bicarbonate • Massive transfusion of whole blood |
|
|
Respiratory Imbalance
|
• PCO2 is the respiratory function indicator.
• In a respiratory imbalance, you will note opposite responses of the pH and PCO2; in other words, the pH will be down with an increased PCO2 (acidosis) or the pH will be up with the PCO2 down (alkalosis). • Look at the pH and PCO2 to determine whether the condition is a respiratory problem. • In respiratory acidosis, pH is down and PCO2 up. • In respiratory alkalosis, pH is up and PCO2 down |
|
|
Metabolic Imbalance
|
• Bicarbonate (HCO3–) is the metabolic function indicator.
• In a metabolic imbalance, you will find a corresponding response between the pH and HCO3–; that is, the pH and HCO3– will both be down (acidosis) or the pH and HCO3– will both be up (alkalosis). • Look at pH and HCO3– to determine whether the condition is a metabolic problem. • In metabolic acidosis, pH is down and HCO3– down. • In metabolic alkalosis, pH is up and HCO3– up. |
|
|
Blood gas assessment
|
Step 1: Look at the pH. Is it up or down? If it is up, alkalosis may be present. A decreased pH reflects acidosis.
Step 2: Look at the PCO2. Is it up or down? If its response is opposite that of the pH, you know that the condition is a respiratory imbalance. If its response is not opposite that of the pH, move on to step 3. Step 3: Look at the bicarbonate (HCO3–). Does the change in HCO3– correspond with that of the pH? If it does, the condition is a metabolic imbalance. Step 4: Compensation has occurred if the pH is in the normal range of 7.35 to 7.45. If the pH is not within the normal range, look at the respiratory or metabolic function indicators to determine the degree of compensation. |
|
|
Warning Signs of CA
|
• Change in bowel and bladder habits
• A sore that does not heal • Unusual bleeding or discharge • Thickening or a lump in the breast or elsewhere • Indigestion or difficulty in swallowing • Obvious change in a wart or mole • Nagging cough or hoarseness |
|
|
A yearly mammogram is recommended starting at age _______ and continuing for as long as a woman remains in good health
|
40
|
|
|
Clinical breast examinations about every ____ years are recommended for women in their twenties and thirties; women over the age of 40 should have one each ____
|
3
year |
|
|
Perform breast self-exam ________ days after start of menstruation
|
7
|
|
|
Normal Breath Sounds
|
• Bronchovesicular: moderately pitched; heard over the major bronchi
• Vesicular: low-pitched rustling; heard over the peripheral lung fields • Bronchial (tracheal): high-pitched, with a harsh, hollow, tubular quality heard over the trachea and larynx |
|
|
Abnormal Breath Sounds
|
• Crackles
o Fine: discontinuous high-pitched crackling sounds heard during inspiration that do not clear with coughing o Coarse: loud, low-pitched bubbling and gurgling sounds heard on inspiration (may be present on expiration); may decrease with coughing or suctioning but reappear • Wheezes: high-pitched, continuous musical sounds heard during inspiration or expiration • Rhonchi: loud, low-pitched, coarse rumbling sounds heard during inspiration or expiration; may be cleared by coughing • Pleural friction rub: dry, grating quality sounds heard best during inspiration; does not clear with coughing |
|
|
Tensilon test: cholinergic crisis
|
overmedication with anticholinesterase drugs
-worsening of the s/s after test dose |
|
|
Tensilon test: myasthenic crisis
|
undermedication with cholinesterase inhibitors
-brief improvement in muscle strength |

