![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
88 Cards in this Set
- Front
- Back
|
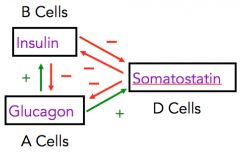
Which cells create insulin? Glucagon? |
Insulin = beta cells. Glucagon = alpha cells. |
|
|
What hormone is released by pancreatic delta cells? |
Somatostatin |
|
|
What type of hormones circulate without carrier proteins? Name six examples we've talked about? |
Peptide; insulin/glucagon, GH, Angiotensin II, ACTH, ADH |
|
|
When glucose goes up, what hormone is secreted? |
Insulin |
|
|
What are incretins? |
Digestive system-prod. hormones which trigger insulin release |
|
|
What's the normal fasting level for blood glucose? |
90-100mg/mL |
|
|
What type of receptors does insulin trigger? |
RTK's |
|
|
What does insulin do in muscle? |
Stimulates glucose uptake, anabolism (building) |
|
|
What's insulin's effect on protein metabolism and growth? |
Promotes protein synth and storage, inhibits degradation. |
|
|
What does insulin act synergistically with to promote protein synthesis and storage? |
Growth hormone |
|
|
What's the effect of insulin on the liver? |
Promotes glucose uptake, storage |
|
|
What's the effect of insulin on fat metabolism? |
Promotes fat building and storage. |
|
|
What's the effect of insulin on plasma levels of: glucose, free fatty acids, ketoacids, and amino acids? |
Decrease! Uptake by cells is promoted. |
|
|
What does beta adrenergic stimulation do in regards to insulin release? Alpha adrenergic stimulation? |
Beta adrenergic stim. promotes insulin release, whereas alpha inhibits |
|
|
What's the "hormone of starvation"? |
Glucagon (I always think– make glycogen gone). Glycogen being storage molecule for gluc. chain. |
|
|
Three factors stimulating glucagon release? |
Hypoglycemia (fasting), epinephrine, vagal stimulation (parasympathetic) |
|
|
Two factors inhibiting glucagon release? |
Hyperglycemia, somatostatin |
|
|
What effects on hormonal release does glucagon have? (2) |
Stimulates insulin and somatostatin release |
|
|
Four things which promote somatostatin release? |
Increased: amino acids, blood glucose, fatty acids, glucagon |
|
|
Three effects of somatostatin? |
Inhibit insulin and glucagon secretion, decrease motility of GI tract, decrease absorption, secretion of GI tract. |
|
Fill in blanks (in boxes) with either insulin, glucagon, somatostatin |
|
|
|
Diabetes mellitus stems from a problem related to this hormone, whereas insipidus is related to this hormone: |
Mellitus = insulin. Insipidus = ADH |
|
|
Type 1 diabetes arises from what pathology? Type 2? |
Type 1 is insulin deficiency, type 2 is insulin resistance. |
|
|
Hyperinsulemia would be a characteristic of this type of diabetes: |
Type 2 mellitus |
|
|
Name the three P's of diabetes mellitus: |
Polyuria (frequent urination), Polydypsia (frequent thirst), Polyphagia (frequent hunger) |
|
|
Weight loss even though you are eating more is indicative of this type of diabetes: |
Type 1 diabetes mellitus |
|
|
Tingling, pain, or numbness in the hands and feet is more indicative of this type of diabetes: |
Type 2 mellitus |
|
|
What metric is used to measure long-term blood glucose maintenance? What are "good numbers"? |
A1C- you want it to be less than 6.5% |
|
|
Autoimmune destruction of pancreatic beta cells will result in this type of diabetes: |
Type 1 mellitus |
|
|
How many pancreatic beta cells need to be destroyed before T1 DM happens? |
80-90% |
|
|
What is likely to be the condition of a patient's plasma K+ levels if they have type 1 DM? |
Hyperkalemic |
|
|
What causes diabetic ketoacidosis? What diabetics are most susceptible? |
Excessive metabolisis of fatty acids producing ketones; type 1 diabetics are most susceptible |
|
|
Fruity breath is an indicator of what pathology and is a result of excess production of this molecule: |
Diabetic ketoacidosis; acetone |
|
|
What's the most important risk factor for type 2 diabetes? |
Obesity |
|
|
Cushings syndrome or steroid use can bring about this type of diabetes |
Type 2 mellitus |
|
|
Five chronic complications of mellitus: |
Retinopathy, nephropathy, neuropathy, vascular disease, myopathies |
|
|
What band of muscle fiber does not shrink in size? |
The A band |
|
|
What line delineates a sarcomere? |
The Z line |
|
|
What band is made up of strictly thick filaments? What about thin filaments? |
A is strictly thick filaments, whereas I band is only thin |
|
|
What is the "H zone"? |
The region in-between thin filaments which shrinks during contraction as thick filaments with myosin heads pull thin filaments together |
|
|
What portion of the sarcomere links the central region of thick filaments? |
The M line |
|
|
What portion of the sarcomere anchors thin filaments? |
The Z line |
|
|
What filaments are present in the H zone? |
Only thick filaments |
|
|
What protein in the sarcomere functions like a spring? |
Titin |
|
|
What protein in the sarcomere is like a "ruler" for actin, dictating its length? |
Nebulin |
|
|
What's the function of alpha-actinin? |
Attaches thin filaments to the Z-disk |
|
|
What are the three main features of thin filaments? |
Actin, troponin, tropomyosin |
|
|
What protein blocks the binding site on actin? |
Tropomyosin |
|
|
Explain the function of troponin |
It binds calcium to push tropomyosin off the binding site of actin |
|
|
Which part of actin does myosin bind to? |
G-actin molecules |
|
|
What provides scaffolding for sarcomeres? |
The dystrophin-glycoprotein complex |
|
|
Duchenne and becker muscular dystrophies arise as a deficiency in what? |
Dystrophin necessary for connecting thin filaments to glycoproteins in sarcolemma |
|
|
What are the three phases of muscle twitch? |
Latent, contraction, relaxation |
|
|
How does botox work? |
Prevents the release of Ach at the NMJ |
|
|
What's the function of T-tubules? |
Allow Ca from the sarcoplasmic reticulum to properly perfuse the muscle. |
|
|
What's the portion of the sarcoplasmic reticulum that contacts the T-tubules? |
Terminal cisternae |
|
|
Three steps of an AP through muscle: |
Travels down sarcolemmal membrane, travels down T-tubules, activates DHP receptors. These open SR Ca channels |
|
|
Three points where ATP is essential for contraction |
A) Binds myosin to break cross-bridge connection to actin B) Hydrolyzed to release energy to cock myosin head in prep for power stroke C) Pi release from myosin head (Pi came from ATP hydrolysis) gives energy for power stroke, where myosin drags actin filament toward M-line |
|
|
Six theories behind why muscles fatigue? |
Change in Vm, depleted ACh, blockage of blood flow, NT in brain depletion, too much lactic acid byproduct, depleted glycogen |
|
|
What's happening in the "rigor state" of cross-bridge cycling? |
Myosin and actin are tightly bound |
|
|
What moves myosin and actin out of the rigor state? |
ATP binds myosin, decreases its affinity for actin |
|
|
What two physiologic actions must happen to stop muscle contraction? |
Alpha motor neuron must stop firing, cystolic (in cytosol) Ca must decrease. |
|
|
Type 1 muscle fibers: Size? Metabolic properties? Fatigue properties? |
Small; oxidative (red), fatigue slowly
|
|
|
Type IIA muscle fibers: Size? Metabolic properties? Fatigue properties? |
Medium-sized, Oxidative and glycolytic, resistant to fatigue |
|
|
Type IIB muscle fibers: Size? Metabolic properties? Fatigue properties? |
Large, glycolitic (white instead of red), fatigable |
|
|
Type 1 muscle fibers in the jaw are different elsewhere in the body in that: |
They are large, whereas normally they are the smallest fiber type. |
|
|
What's sarcopenia? |
Decrease in muscle diameter, common with age |
|
|
What size of muscle fibers are recruited first? |
The smallest |
|
|
Small motor units (x) are associated with which type of muscle fibers? |
Type 1 |
|
|
What motor units are recruited last? |
Type Z (IIB fibers) |
|
|
Define isometric contraction: |
Force produced is less than required to move load; no net mvmnt |
|
|
Define isotonic contraction: |
Force produced is great enough to move a load |
|
|
All muscle forces start out using this type of contraction: |
Isometric |
|
|
What are the two ways contractile force is increased? |
1) Increase motor unit recruitment/frequency of fiber activation (temporal) 2) Increase number of muscle fibers contracting (spatial summation) |
|
|
Speed of muscle contraction is a function of what? |
The load size contracting against. |
|
|
The greater the load, the slower/faster the speed of muscle contraction? |
Slower |
|
|
1A fibers go from where to where? 1B? |
1A) Muscle spindle to spinal cord. 1B) Golgi tendon organ to spinal cord. |
|
|
What's the function of gamma muscle fibers? |
They activate intrafusal muscle fibers |
|
|
Extrafusal muscle fibers are activated by what type of neurons? |
Alpha motor neurons |
|
|
Why must intrafusal muscle fibers contract with extrafusal? |
They must stay at the same amount of tension as extrafusal fibers to give constant feedback via 1A nerve fibers regarding the status of muscle contraction |
|
|
What's the main function of the golgi tendon organ? |
Protective, senses changes in force. |
|
|
1A fibers in muscle spindles sense ____ whereas 1B fibers in the golgi tendon organs sense ____ |
1A) length, 1B) force |
|
|
Isometric maximum contractions will send signals via this structure and this nerve in order to stop contraction: |
Golgi tendon organ; 1B |
|
|
What's the effect of the golgi tendon organ reflex? |
Decreased contraction |
|
|
Describe the function of the central pattern generator? |
It works from the brainstem, and generates cyclical coordinated activation and inactivation of jaw openers and closers |
|
|
Describe what causes the jaw opening reflex |
Pain inhibits the alpha motor neuron, resulting in an opening of the jaw |
|
|
Describe the jaw jerk reflex |
A strong tap to the chin stimulates jaw closing muscles, which close the jaw. |
|
|
What reflex would happen by pressing weakly on a tooth? |
The jaw would close (ie– to chew food). |

