![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
53 Cards in this Set
- Front
- Back
|
Tidal volume (TV)
|
Is the volume inspired or expired with each normal breath 500 mL |
|
|
Inspiratory reserve volume (IRV) |
Is the volume that can be inspired over and above the tidal volume 3100 mL |
|
|
Expiratory reserve volume (ERV) |
Is the volume that can be expired after the expiration of a tidal volume 1200 mL |
|
|
Residual volume (RV) |
Is the volume that remains in the lungs after a maximal expiration Cannot be measured by spirometry 1200 mL |
|
|
Dead space |
150 mL |
|
|
Minute ventilation |
Minute ventilation=tidal volume x breaths/min |
|
|
Alveolar ventilation |
Alveolar ventilation= (tidal V-physiological dead space) x breaths/min |
|
|
Inspiratory capacity (IC) |
Is the sum of tidal volume and inspiratory reserve volume IC = TV + IRV |
|
|
Functional residual capacity (FRC) |
Is the sum of expiratory reserve volume and residual volume; 2400 mL FRC = ERV + RV Cannot be measured by spirometry |
|
|
Vital capacity (VC) |
Is the sum of tidal volume, inspiratory reserve volume and expiratory reserve volume; 4800 mL VC = TV + IRV + ERV Is the volume that can be forcibly expired after a maximal inspiration |
|
|
Total lung capacity (TLC) |
Is the sum of all four lung volumes and is the volume in the lunds after a maximal inspiration; 6000 mL TLC = TV + IRV + ERV + RV Cannot be measured by spirometry |
|
|
Forced expiratory volume (FEV1) |
Is the volume of air that can be expired in the first second of a forced maximal expiration FEV1 / FVC = 0.8 |
|
|
Obstructive lung diseases |
E.g. asthma and chronic obstructive pulmonary disease; expiration is impaired Both FEV1 and FVC are reduced, but FEV1 is reduced more than FVC; FEV1 / FVC is decreased |
|
|
Restrictive lund diseases |
E.g. fibrosis; inspiration is impaired Both FEV1 and FVC are reduced, but FEV1 is reduced less than FVC; FEV1 / FVC is increased |
|
|
Compliance |
Describes the distensibility of the lungs and chest wall and is inversely related to elastance and stiffness C = delta V / delta P |
|
|
Transmural pressure |
Transmural pressure = alveolar pressure - intraplural pressure |
|
|
Emphysema |
Increased; lung compliance Decreased; tendency of the lungs to collapse Result; higher FRC |
|
|
Fibrosis |
Increased; tendency of the lungs to collapse Decreased; lung compliance Result; lower FRC |
|
|
Surface tension of the alveoli |
Creates a collapsing pressure that is directly proportional to surface tension and inversely proportional to alveolar radius (Laplace's law) |
|
|
Surfactant |
- Reduce surface tension (increases compliance) - Present as early as gestational week 24 |
|
|
Airflow |
Is inversely proportional to airway resistance; thus, the higher the airway resistance, the lower the airflow |
|
|
Resistance of the airways |
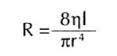
Is described by Poiseuille's law |
|
|
Which factors change airway resistance? |
- Contraction or relaxation of bronchial smooth muscle - Lung volume - Viscosity or density of inspired gas |
|
|
Describe the pressures and airflows at rest |
Alveolar pressure (=0) equals atmospheric pressure Intraplural pressure is negative Lung volume is the FRC |
|
|
Describe the pressures and airflows during inspiration |
Alveolar pressure (=negative) decreases to less than atmospheric pressure Intraplural pressure becomes more negative Lung volume increases; FRC + TV |
|
|
Describe the pressures and airflows during expiration |
Alveolar pressure (=positive) becomes greater than atmospheric pressure Intrapleural pressure returns to its resting value during a normal expiration Lung volume returns to FRC |
|
|
Perfusion-limited exchange |
E.g. N2O and O2 under normal conditions The gas equilibrates early along the length or the pulmonary capillary. The partial pressure of the gas in the arterial blood becomes equal to the partial pressure in alveolar air. Thus, the perfusion-limited process, diffusion of the gas can be increased only if blood flow increases. |
|
|
Diffusion-limited exchange |
E.g. Co and O2 during strenuous exercise The gas does not equilibrates by the time blood reaches the end of the pulmonary capillary. The partial pressure difference of the gas between alveolar air and pulmonary capillary blood is maintained. Diffusion continues as long as the partial pressure gradient is maintained. |
|
|
Methemoglobin |
- Iron is in the Fe3+ state - Does not bind O2 |
|
|
Hemoglobin S |
- Causes sickle cell disease - In the deoxygenated form, deoxyhemoglobin forms sickle-shaped rods that deform red blood cells (RBCs) |
|
|
Which factors affect the hemoglobin dissociation curve to shift to the right? |
Occur when the affinity of hemoglobin for O2 is decreased
- Increase in PCO2 - Decrease in pH - Increase in temperature - Increase in 2,3-DPG concentration |
|
|
Which factors affect the hemoglobin dissociation curve to shift to the left? |
Occur when the affinity of hemoglobin for O2 is increased - Decreased PCO2 - Increased pH - Decreased temperature - Decreased 2,3-DPG concentration - CO poisoning |
|
|
Causes of hypoxemia |
Hypoxemia is decreased arterial PO2 - High altitude - Hypoventilation - Diffusion defect - V/Q defect - Right-to-left shunt |
|
|
Causes of hypoxia |
Hypoxia is decreased oxygen delivery to the tissues - Decrease in cardiac output - Hypoxemia - Anemia - Carbon monoxide poisoning - Cyanide poisoning |
|
|
Erythropoietin (EPO)
|
A growth factor that is synthesized in the kidneys in response to hypoxia |
|
|
Regulation of pulmonary blood flow |
Hypoxic vasoconstriction (which is opposite than in other organs) |
|
|
Right-to-left shunts |
Rare Decrease in arterial PO2 because of the admixture of venous blood with arterial blood |
|
|
Left-to-right shunts |
More common Do not result in a decrease in arterial PO2 |
|
|
V/Q ratio |
Is the ratio of alveolar ventilation (V) to pulmonary blood flow (Q); 0.8 The V/Q ratio results in an arterial PO2 of 100 mmHg and an arterial PCO2 of 40 mmHg Perfusion is lowest at the apex and highest at the base because of gravitational effects on arterial pressure |
|
|
Control of breathing |
The output of the brain stem controls the respiratory muscles and the breathing cycle |
|
|
Central control of breathing |
Medullary respiration center 1) dorsal respiratory group 2) ventral respiratory group Apneustic center Pneumotaxic center Cerebral cortex |
|
|
Dorsal respiratory group |
Inspiration and the basic rhythm for breathing |
|
|
Ventral respiratory group |
Expiration and is not active during normal, quiet breathing Activated during exercise |
|
|
Apneustic center |
Lower pons Stimulates inspiration |
|
|
Pneumotaxic center |
Upper pons Inhibits inspiration |
|
|
Cerebral cortex |
Voluntary control; hyperventilation and hypoventilation |
|
|
Chemoreceptors |
CO2, H+ and O2 - Central chemoreceptors in the medulla - Peripheral chemoreceptors in the carotid and aortic bodies |
|
|
Central chemoreceptors in the medulla |
Sensitive to pH of the CSF; decreased pH of CSF produce hyperventilation Stimuli that increase breathing rate: - High; PCO2 - Low; pH |
|
|
Peripheral chemoreceptors in the carotid and aortic bodies |
Decreases in arterial PO2; hyperventilation Increases in arterial PCO2; hyperventilation Increases in arterial H+ |
|
|
Metabolic acidosis |
Hyperventilation because the arterial H+ concentration is increased and pH is decreased |
|
|
Other types of receptors for control of breathing |
- Lung stretch receptors (Hering-Breuer reflex) - Irritant receptors - Juxtacapillary receptors - Joint and muscle receptors |
|
|
Response to exercise |
Increased; O2 consumption, CO2 production, ventilation rate, venous PCO2, pulmonary blood flow Decreased; Arterial pH in strenuous exercise No change; Arterial PO2 and PCO2, arterial pH V/Q ration is more evenly distributed in lung (=decrease in physiological dead space) |
|
|
Response to high altitude |
Increased; Ventilation rate (hyperventilation), arterial pH (respiratory alkalosis), hemoglobin concentration (increased EPO), 2,3-DPG concentration, pulmonary vascular resistance (hypoxic vasoconstriction) Decreased; Alveolar PO2, Arterial PO2 (hypoxemia) Hemoglobin-O2 curve shifts to the right |

