![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
32 Cards in this Set
- Front
- Back
|
Describe homeostasis & its importance in physiology.
|
Homeostasis is the maintenance of the internal environment within narrow limits. It is controlled by feedback mechanisms which are affected by disease/dysfunction. Alteration of this control results in disease/dysfunction
|
|
|
What is the flow of fluids through a tube/vessel dependent on?
|
force (pressure difference), tube (diameter & length), fluid (viscosity & density), flow (laminar/turbulent)
|
|
|
What happens to arteries in atherosclerosis? Name some consequences of atheroma in different parts of the body.
|
They become narrowed - causing turbulent & noisy flow of blood.
Brain - stroke, Heart - heart attack, Kidneys - renal failure |
|
|
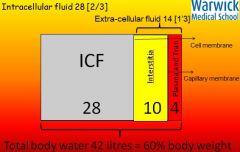
What is the total volume of body water? How is it distributed in the body?
|
|
|
|
What governs the movement of water between the passive capillary membranes between the blood & interstitial fluid?
|
Starling Forces:
- hydrostatic (vascular) pressures - oncotic pressures (form of osmotic pressure exerted by proteins in plasma) |
|
|
How is does membrane transport between interstitial & intracellular fluid differ to transfer between interstitial & blood plasma?
|
Transfer is across an active membrane - cell wall. Water & ions are transferred by active processes.
|
|
|
Explain how Starling forces govern equilibrium between plasma & interstitial fluid.
|
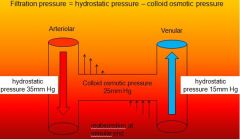
Loss of fluid from the plasma owing to hydrostatic pressure is opposed by reabsorption of fluid into plasma owing to oncotic pressure/colloid osmotic pressure. The impermeance of plasma proteins draws fluid back into capillaries.
|
|
|
What are the values of arteriolar vs venular hydrostatic pressures?
|
Arteriolar = 35mmHg
Venular = 15mmHg |
|
|
What is the movement of water influenced by in the body?
|
Hydrostatic pressure generated by gravity or the heart (or both),
Oncotic pressure, Type & integrity of membranes. |
|
|
What can go wrong that influences water movement & give examples of how this can occur?
|
Things that can go wrong:
- fall in plasma protein - starvation (low input), liver failure (not enough made) - defect in capillary membrane - increasing tissue oncotic pressure leads of oedema as in inflammation, anaphylaxis & sepsis - rise in venous pressure - heart (pump) failure, fluid overload |
|
|
What ion channels are important for nerve conduction? What causes these to open & close & what does this result in?
|
Sodium & potassium voltage-gated ion channels. A change in voltage causes them to open/close, resulting in a self-propagating wave of depolarisation
|
|
|
Describe the action potential.
|
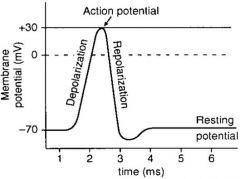
Depolarisation results in an AP (30mV), followed by repolarisation, a refractory period, then back to the resting potential (-70mV)
|
|
|
Briefly describe the myelin sheath & function.
|
Myelin is produced by oligodendrocytes and insulates nerve cell axons. Nodes of Ranvier allow salutatory conduction down the axon.
|
|
|
What is an acid & a base?
|
An acid donates protons (H+ ions). A base accepts protons. Acids have pH values <7, bases have pH values >7.
|
|
|
What do strong acids usually do in solution?
|
Dissociate completely.
|
|
|
Why is maintaining pH important in physiology?
|
Changes in acidity profoundly affect proteins. Protein function relies on their shape, which changes with pH.
|
|
|
What are the normal pH limits in the body?
|
7.35 - 7.45
|
|
|
What disturbs the body's pH?
|
CO2 production (respiration - when glucose is metabolised via glycolysis) & metabolic acids (anaerobic metabolism produces lactic acid, & accumulates in shock). Protein breakdown produces acids.
|
|
|
How does the body prevent pH changes?
|
Buffers allow acid to be 'stored' temporarily. Bicarbonate/ CO2 is the most important. CO2 can be excreted by the lungs.
Proteins can reversibly accept H+ ions e.g. intracellular phosphate |
|
|
What is the reaction when excess acid (H+) is present that produces CO2?
|
H+ + HCO3- --> CO2 + H2O
|
|
|
What is the reaction for intracellular phosphate accepting H+ ions?
|
HPO4 ^2- + H+ --> H2PO4-
|
|
|
How is excess acid expelled from the body?
|
Respiratory acid (CO2) is excreted by the lungs - increase ventilation rate & depth. Metabolic acids are excreted by the kidneys.
|
|
|
What does excess acid or base in the body produce?
|
Respiratory or metabolic: acidosis or alkalosis.
|
|
|
What does an Arterial Blood Gas Analysis reveal & what does it include?
|
Oxygenation & acid/base status of the body.
pH paO2 paCO2 BE (Base Excess) |
|
|
What do positive/negative values of Base Excess (BE) tell you?
|
Positive = acidosis
Negative = alkalosis |
|
|
What are normal Arterial Blood Gas Analysis values?
|
paO2: 10-13 kPa
pH: 7.35-7.45 paCO2: 4-4.5 kPa BE: -2-2 mmol/l |
|
|
How would you interpret Arterial Blood Gas Analysis values?
|
First look at pH (low = acid, high = base). Next look at paCO2 (high = respiratory acidosis). Then BE (-ve = metabolic acidosis). To interpret paO2 you need to know what [O2] the patient is breathing.
|
|
|
Can the body overcompensate for disturbances to acid/base?
|
The body NEVER OVERCOMPENSATES for disturbances.
The lungs can compensate QUICKLY. The kidneys can compensate for metabolic disturbances SLOWLY. But when things go wrong, a metabolic acidosis can build up FAST. |
|
|
At which angle (straight or right angle) does the knee jerk reflex give a better twitch & why?
|
Right angle because there must be tension in the muscle/tendon for demonstration of the reflex. The muscle is already contracted when leg is straight.
|
|
|
Why does teeth clenching improve the knee-jerk reflex?
|
Descending inhibition of spinal inhibitory pathways.
|
|
|
Name one cause of alkalosis.
|
Hyperventilation - either tidal volume or respiratory rate (or both) too high
|
|
|
Name one cause of acidosis.
|
Poor perfusion.
|

