![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
33 Cards in this Set
- Front
- Back
|
Functions of the blood: Transports: Protection: |
Oxygen, CO2, nutrients, waste,heat, and hormones maintenance of normal Ph, normal body fluidvolume, hemostasis, fight infection, and maintainhomeostasis |
|
|
Blood turns red when: and blue when: hemoglobin is: |
hemoglobin binds with O2, hemoglobin binds with CO2 a pigmented protein in erythrocytes |
|
|
Plasma: Buffy coat: hematocrit: a drop of blood outside the body separates into: |
55%, least dense, contains H2O, proteins, electrolytes, hormones, andnutrients less than 1%, contains leukocytes, platelets % RBC's, about 45%, most dense component serum (plasma - fibrinogen) and clot (hematocrit plus fibrinogen) (reddish dense mass of cells) |
|
|
formed elements of blood: The source of plasma water: The source of plasma protein: The source of blood cells: |
WBC, RBC, platelets ingested H2O liver bone marrow |
|
|
Source of RBC formation: Primary: Secondary: Tertiary: |
In adults, blood cells are formed by the red bonemarrow in the sternum, ribs,vertebrae, skull, and pelvis. Secondary: Blood cells can be formed by the marrow in thefemur & tibia (if necessary). Tertiary: In E.R. (excessive blood loss) blood cells can beformed in liver and spleen. |
|
|
Embryo primary RBC source: RBC's lack _____ and do not perform _________ |
liver and spleen nuclei, mitosis during their short lifetime (120 days) |
|
|
RBC increases: critical nutritional factors: Hormone that stimulates RBC formation: |
afterexercising, after a largemeal, when a person is athigh altitudes, or whenbody temperature rises. vitaminB-12, folic acid, and iron Erythropoietin from thekidney stimulate RBCproduction from the bonemarrow. |
|
|
Blood prevents blood loss by: Prevents infection by: |
Activating plasma proteins and platelets Initiating clot formation when a vessel is broken Synthesizing and utilizing antibodies, Activating complement proteins, Activating WBCs to defend the body against foreign invaders |
|
|
anemia: check notes - do I need to know each kind? |
a condition where the oxygen – carryingcapacity of blood is reduced due to RBC or hemoglobindeficiency, and result in lack of energy in the person |
|
|
leukocytes: 2 groups and their subcategories: phagocytes and their subcategories: |
less than .1% of blood, generally function in lymphatic system granulocytes (WBC that contain granules in theircytoplasm with their nuclei divide into lobes): Neutrophils, Eosinophils, Basophils agranulocytes (lack granules): lymphocytes, monocytes leukocytes that have the ability to engulf foreignsubstances for body defense purposes. These include the neutrophils, eosinophils, and monocytes |
|
|
Monocytes develop into ____, which: Netruophils phagocytize: Eosinophils: Basophils: |
macrophages, travel long distances to find foreign substances small particles in blood or connective tissue control inflammation and allergic reaction release anticoagulant (to prevent spontaneous blood clotting) and histamines to enhance inflammation |
|
|
monocytes lymphocytes: platelets = and are critical in forming: |
phagocytize larger cells in connective tissues attack foreign agents directly or indirectly by forming antibodies thrombocytes, platelet plugs in hemostasis and blood clots with fibrinogen |
|
|
Albumin: Globulin: Fibrinogen: |
Albumin is critical in maintaining osmotic pressure in bloodand body fluids. Globulin serves as protein transporters (e.g.for steroid hormones). Fibrinogen is converted into fibrins inthe formation of a blood clot. |
|
|
plasma lipids combine with globulins to form: VLDL: LDL: |
lipoproteins Very low density lipoproteins (VLDL) have a high amount oftriglyceride. It transports triglycerides synthesized in the liverfrom carbohydrates to adipose cells (bad cholesterol).
Low density lipoproteins (LDL) have a high amount ofcholesterol . Delivers cholesterol to various cells, includingliver cells (bad cholesterol). |
|
|
HDL |
High density lipoproteins (good cholesterol) Relatively high concentration ofprotein and low concentration of lipids. Function: Transports to the liver remnants ofchylomicrons that have given up their cholesterol. Note: A high ratio of HDL to LDL cholesterolappears to ward off plaque formation and heartdisease. |
|
|
Major events in red blood cell destruction |

1. Squeezing through the capillaries of active tissues damagesred blood cells. 2. Macrophages in the liver & spleen phagocytize damaged redblood cells. 3. Hemoglobin from the red blood cells is decomposed intoheme and globin. 4. Heme is decomposed into iron and biliverdin. 5. Iron is made available for reuse in the synthesis of new hemoglobin or is stored in the liver as ferritin. 6. Some biliverdin is converted into bilirubin. 7. Biliverdin and bilirubin are excreted in bile as bile pigments. |
|
|
Hormonal control of RBC steps: |
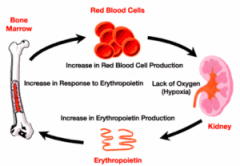
The kidney & liver tissue experience an O2deficiency. These tissues release the hormone erythropoietin. Erythropoietin travels to the red bone morrow and stimulates an increase in production of red cells. As increasing number of red blood cells arereleased into the circulation, the O2 – carryingcapacity of blood rises. The O2 concentration in the kidney and liver tissue increases, and the release of erythropoietin decreases. |
|
|
3 dietary factors affecting RBC production: |
vitamin B12, Iron, Folic acid |
|
|
B12 source and function: Iron source and function: Folic Acid source and function: |
source: Absorbed from small intestine. Function: DNA synthesis. Requires intrinsic factor for absorption. Absorbed from small intestine; conserved during red celldestruction and made available for reuse. Function: Hemoglobin synthesis. Req. Vit. C Absorbed from small intestine. function: DNA synthesis. |
|
|
hemostasis: |
the stoppage of bleeding Blood clotting involves a series of Rxs wherein each reactionstimulates the next Rx, which may be initiated by extrinsic orintrinsic mechanisms. Clot formation depends on the balance between clotting factors that promote clotting and those that inhibit clotting. |
|
|
extrinsic and intrinsic mechanisms: |
The extrinsic clotting mechanism is triggered when blood contacts damaged tissue. Damaged blood vessels in the injuredarea release "tissue thromboplastin ", which after a series ofchemical reaction, produces "prothrombin activator " The intrinsic clotting mechanism is triggered when blood contacts a foreign surface. blood being exposed to collagen fibersor other foreign substances after blood vessels are opened, willrelease the "Hageman factor", which will also produce the "pro-thrombin activator" |
|
|
Prothrombin activator |
"prothrombin activator " converts prothrombin (produced byliver) into thrombin, which in turn converts fibrinogen intofibrins. These steps require calcium and "clotting factors"(proteins that facilitate blood coagulation |
|
|
4 steps of blood clotting: |
1. Injury to wall of blood vessel 2. Vasoconstriction 3. Platelet Plug Formation 4. Clot formation |
|
|
Injury to wall of blood vessel: Vasoconstriction: |
Injury (cut) to a blood vessel is followed by a series of reactionsthat result in the formation of a blood clot, which seals theinjured opening and prevents the loss of blood. Adhesion of blood platelets to the exposed collagen fibers (inthe wall of the injured vessel) cause the release of serotoninfrom platelets, which induces strong vasoconstriction anddecrease blood flow. |
|
|
Platelet plug formation: |
contact of the platelets with collagen in the injuredwall releases thromboxane A2, which inducesaggregation of more platelets in the plug area andstimulates the formation of platelet pseudopods.These enable the platelet aggregates to bindtogether, forming a temporary plug to stop bloodloss (platelets adhere to rough surfaces and to eachother, forming a plug) |
|
|
clot formation: |
To strengthen the plug, Fibrinogen, a blood protein isconverted to fibrin; fibrin forms a net over the platelets. Red cells inthe center and exterior of the plug adhere to this net. The combinationof platelets and red cells entangled within a tight fibrin net forms ablood clot, a stronger and more permanent plug to stop blood loss |
|
|
see desktop for photo summary |
see other side |
|
|
To dissolve a clot: |
the enzyme plasmin lyses the fibrinnet; plasmin is formed from an inactive precursor, plasminogen |
|
|
4 clotting factors: CHECK that we only need to know 4 |
I . FibrinogenII. ProthrombinIII. Tissue ThromboplastinIV. Calcium |
|
|
6 factors that inhibit blood clot formation |
1. Smooth lining of blood vessel – prevents activation of intrinsicblood clotting mechanism. 2. Prostacyclin - inhibits adherence of platelets to blood vessel wall. 3. Fibrin threads - absorbs thrombin. 4. Antithrombin in plasma - interferes with the action of thrombin. 5. Heparin from mast cells and basophils - interferes with theformation of prothrombin activator. 6. Aspirin - inhibits prostaglandin production resulting in a defectiveplatelet release reaction. |
|
|
agglutination: blood group is based on: Order of popularity: |
clumping of erythrocytes when blood groups with different antigens and antibodies mix and bind antigen presence O, A, B, AB |
|
|
Antigens are synthesized during fetal development. About 2-8months after birth, the immune system will spontaneouslydevelop specialized proteins called antibodies to be"compatible" with these antigens |
see other side |
|
|
universal donor: universal recipient: |
O AB |

