![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
80 Cards in this Set
- Front
- Back
|
True or False:
Action potential duration is much longer in heart than in cardiac muscle but the duration of contraction is comparable. |
True
p. 253 |
|
|
[ Cardiac / Skeletal ] SR has smaller volume and more mitochondria.
|
Cardiac
p. 254 |
|
|
Where are T-tubules located in cardiac muscle versus skeletal muscle?
|
cardiac: @ Z-line
skeletal: @ A-I bands note: T-tubules are sparse in atria and absent in PKJ fibers p. 254 |
|
|
Junction of SR and sarcolemma differs in heart and skeletal muscle. In heart, cisterna of SR forms [ diads / triads ] with limited SR-T tubule contact.
|
Diads
p. 254 |
|
|
Macroscopically, cardiac fibers are [ interwoven / parallel ] whereas skeletal fibers are [ interwoven / parallel ].
|
cardiac = interwoven
skeletal = parallel p. 254 |
|
|
Why does the heart's excitation-contraction coupling include a step of "Ca2+ - induced Ca2+ release" ? What does this mean?
|
Small amount of calcium from I Ca is the trigger for a large release of Ca2+ from SR. SR calcium release channel is the ryanodine receptor (RyR2).
p.254 |
|
|
Ca2+ - induced Ca 2+ release is graded by two factors. What are they?
|
- Size of trigger (amount of Ca2+ coming in from I Ca)
- amount of Ca2+ stored in SR p. 254 |
|
|
True or False:
The primary source of Ca2+ responsible for the increase of intracellular calcium concentration is the influx of Ca2+ from I Ca. |
FALSE. The primary source of increase is from Ca2+ release from SR!!
p. 254 |
|
|
When Ca2+ binds to troponin -C (TnC), tropomyosin shifts on the thin filament, unblocking myosin binding site and allowing weak binding of actin. That weak complex undergoes a cooperative conformational change, forming strong crossbridges that rapidly split ATP and generate force. These strong complexes [ decrease / increase ] the Ca2+ affinity of TnC.
|
strong A-M complexes INCREASE the affinity of Ca2+ for TnC.
p. 255 |
|
|
True or False:
Intracellular calcium concentration returns to near resting levels before relaxation begins; Ca2+ unbinding from TnC ends A-M ATPase activity and force production. |
True! It returns to near resting levels BEFORE relaxation begins.
p. 255 |
|
|
Regarding regulation of intracellular calcium concentration, what are the sarcolemmal processes for influx (1) and efflux (2) of Ca2+?
|
Influx: I Ca (L-type)
efflux: Na- Ca exchange IS THE PRIMARY MEANS OF EFFLUX)*** antiport: 3 Na+ IN , 1 Ca2+ OUT. Another way is the sarcolemmal Ca pump which directly extrudes calcium by splitting ATP. p. 255 |
|
|
Action potential duration can influence contractile force. Why/how?
|
APD is mainly dictated by the plateau created by I Ca. So decreasing APD means reduced I Ca --> smaller trigger for Ca2+ release from SR and also less amount of Ca2+ available to fill SR Ca2+ stores. p. 256
|
|
|
There is no recruitment regarding cardiac muscle contractile force. What does this mean/ indicate?
|
The heart is an electrical syncitium. Every fiber is activate. Each cell is electrically coupled with other cells thus every cell participates with each heartbeat. p. 257
|
|
|
In cardiac muscle, there is no tetanic contraction. This is because...
|
APD is slightly LONGER than the duration of contraction. Additionally, refractory period prevents stimulation at high enough rate.
p. 257 |
|
|
Which part of the autonomic nervous system has a
a) positive inotropic effect? b) negative inotropic effect? |
Inotropic effect refers to affecting the contractility (the intrinsic ability of the muscle to generate force independent of muscle length).
Positive = sympathetics (NE) Negative = parasympathetics (Ach) p. 258 |
|
|
[ Contractility / Contractile force ] is the intrinsic ability of the muscle to generate force independent of muscle length.
|
Contractility
p. 258 |
|
|
True or False:
Contractility is increased by elevating heart rate either by electrical stimulation or physiologically by sympathetic stimulation. |
True
p. 258 |
|
|
When HR is increased by NE, the [ duration / frequency ] of contraction decreases and rate of relaxation [ decreases / increases ], termed positive lusitropy.
|
when HR is increased by NE, DURATION or contraction decreases, rate of relaxation increases.
p. 258 |
|
|
The ascending staircase / positive staircase / Bowditch staircase / Treppe relates what relationship?
A. contractility : frequency B. force of contraction : frequency C. rest potentiation : HR |
B. force of contraction : frequency
p. 259 |
|
|
After a longer thannormal interval between beats, the first beat will exhibit greater than normal contractile force. What is this phenomenon called?
|
Rest potentiation.
This reflects the kinetics of SR Ca 2+ accumulation and Ca 2+ cycling in the SR. p. 259 |
|
|
Resting tension increases more rapidly with increasing muscle length in heart than in skeletal muscle. In other words,
A. a much greater preload is required to elongate cardiac muscle to max length than to elongate skeletal muscle B. cardiac muscle is stiffer than skeletal muscle |
B. cardiac muscle is stiffer than skeletal muscle . This is due to differences in the isoform of titin.
p. 261 |
|
|
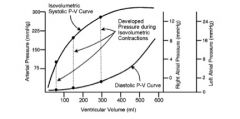
Why is cardiac muscle said to only operate on the ascending limb of Force-Tension curve?
|
Force produced by ventricular filling and atrial contraction is insufficient to stretch cardiac muscle beyond maximum length (and it is beyond maximum length that you'd get the descent). p. 261
|
|
|
What is the maximum sarcomere length for cardiac muscle?
A. 1.9 micrometers B. 2.0 micrometers C. 2.2 micrometers D. 2.5 micrometers |
C. 2.2 micrometers
is the max though working length (at end of diastole is 1.9 micrometers). p. 261 |
|
|
What are the four consequences of organs/ tissues being connected in parallel? (hint: think basic)
|
1. A given volume of blood ejected from the L ventricle passes thru only one organ before entering veins.
2. Aterial blood entering each organ has the same composition. 3. Blood pressure at the entrance to each organ is the same 4. Blood flow to each organ can be controlled independently (local regulation of flow). p. 266-7 |
|
|
Review of basics:
force/ area = _____ |
pressure
p.267 |
|
|
Review of basics:
volume / time = ____ |
flow (Q)
p. 268 |
|
|
Review of basics:
pressure difference / flow = ____ |
resistance
blood "resists" being moved becuase friction develops between the blood and the vessel wall, in addition to the friction that develops between adjacent imaginary layers (laminae) of blood. p. 268 |
|
|
Review of basics:
Give the equation for A) resistance in series B) resistance in parallel |
A) series: R1 + R2 = R eff
B) parallel: 1/(R1) + 1/(R2) = 1/(Reff) note, if the resistances are all equal in the parallel, you can also write it as R/N= R eff p. 269 |
|
|
Flow is proportional to radius (or diameter) to the ______ power.
A. 2nd B. 3rd C. 4th |
C. 4th power. Thus, small changes in vascular caliber can produce profond changes in blood flow thru a vascular segment. p. 272
|
|
|
Which vessels are colectively known as the "resistance vessels" in the vasculature?
|
Arterioles. This is where regulation of blood flow takes place. Note, capillary has the smallest radius of all blood vessels, so an individual capillary has the highest resistance to blood flow BUT the collective resistance to flow of all capillaries is less than the collective resistance to flow of all the arterioles. p. 272
|
|
|
Capillary has the smallest radius of all blood vessels, so an individual capillary has the highest resistance to blood flow. So why are arterioles the ones called "resistance vessels"?
|
The collective resistance to flow of all capillaries is less than the collective resistance to flow of all the arterioles. This is due to the sheer number of capillaries (much greater than arterioles). p. 272
|
|
|
What is the Law of Laplace and what does it describe?
|
Tension = (Transmural pressure * internal radius) / Wall Thickness
what determines the diamter of a blood vessel: take into accoun the distending force and compressing force for a thin walled object p. 273 |
|
|
True or False:
Both changes in blood pressure and changes in vascular smooth muscle contractile state can produce immediate changes in vessel diameter. |
TRUE. These are what determines the diamter of a blood vessel: take into accoun the distending force and compressing force. p. 274
|
|
|
True or False:
Whole blood (suspension of red cells in plasma and the viscosity of blood) depends on fluid velocity and thus is "non-Newtonian". |
True.
p. 275 |
|
|
What are the four major factors that determine the viscosity of blood?
|
1. Temperature ( Increase in temp = decrease in viscosity )
2. Hematocrit , the fractional volume of blood occupied by red cells. (Increase in Hct = Increase in viscosity) 3. Tube/vessel diameter ( below~300 micrometers, as diameter decreases, viscosity decreases) 4. Shear rate (relative velocity of one imaginary layer of fluid with respect to that of adjacent layers). As max shear rate increases, viscosity of blood decreases. p. 275-7 |
|
|
Acute, transient increases in shear rate lead to vasodilation due to shear-induced release of vasodilator _________ from the endothelium.
|
nitric oxide
remember, shear rate is the relative velocity of one imaginary layer of fluid with respect to that of adjacent layers p. 279 |
|
|
In low flow states (circulatory shock, for ex), [ high / low ] shear rates lead to [ decreased / increased ] viscosity that tend to reinforce the low flow creating a positive feedback that results in a vicious cycle.
|
in low flow states, LOW shear rates lead to INCREASED viscosity that tend to reinforce low flow!! p. 279
|
|
|
As the maximum shear rate increases, the viscosity of blood decreases. This is due to...
|
the breakup of aggregates of RBC (forms aggregates at low flows b/c they have a natural tendency to stick together). p. 278
|
|
|
True or False:
Reynold's number helps distinguish between laminar and turbulent flow. |
True. For values above 2,000 flow becomes turbulent. p. 280
|
|
|
Increase in shear rate [ decreases / increases ] viscosity. Why?
|
Increase in shear rate decreases viscosity. RBCs tend to stick together, thus increasing shear rate (relative velocity between RBCs) decreases aggregating tendencies and thus decreases viscosity. p. 279
|
|
|
S1 "lub" heart sound is due to [AV / semilunar ] valves snapping shut.
|
AV valves snapping shut
|
|
|
S2 "dub" heart sound is due to [AV / semilunar ] valves snapping shut.
|
semilunar valves snapping shut (note the aortic valve shuts slightly before the pulmonary valve).
|
|
|
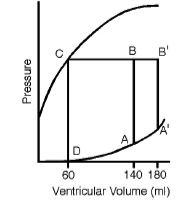
True or False:
Systole, active contraction of the heart, is about 1/3 of the cardiac cycle. |
True
p. 281 |
|
|
Stroke volume is...
|
amount of blood ejected during systole (ml/beat). calculated by:
Stroke Volume = End Systolic Volume - End Diastolic Volume p. 281 |
|
|
_________ is the volume of blood in the ventricle at completion of _______ as marked by closure of the aortic and pulmonic valves
|
ESV (end systolic volume) ; completion of systole p. 281
|
|
|
The ejection fraction for the normal heart is always greater than or equal to:
A. 0.45 B. 0.50 C. 0.55 D. 0.60 |
C. 0.55
p. 281 |
|
|
Cardiac output is typically ___ L / min. Can be calculated by the equation...
|
5 L/ min ; can be calculated by the equation CO = HR* SV
p. 281 |
|
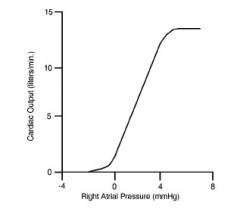
What is this?
|
Cardiac Function Curve!
Relates Right Atrial Pressure to CO. p. 282 |
|
|
True or False:
The Law of LaPlace relates tension and pressure relationship. |
True. For thin-walled sphere, P=(2HT)/r where H is wall thickness, T is tension, r is radius, P is pressure
p. 282 |
|
|
According to the Law of LaPlace, what is the relationship (proportional, inversely proportional) between
A. Tension and Pressure B. Tension and Radius C. Tension and Wall Thickness |
A. Tension is proportional to Pressure
B. Tension is proportional to Radius C. Tension is inversely proportional to Wall Thickness p. 282 |
|
|
Regarding EDV (end diastolic volume), ______ is "preload" and ______ is "afterload".
|
For EDV,
right atrial pressure = preload aortic pressure = afterload p. 283 |
|
|
|
|
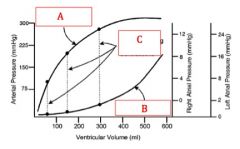
What does this relate?
A. Increased afterload B. Increased preload C. Increased contractility |
B. Increased preload
p. 284 |
|
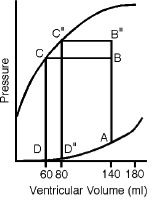
What does this relate?
A. Increased afterload B. Increased preload C. Increased contractility |
A. Increased afterload
p. 284 |
|
|
True or False:
Regarding Frank-Starling Compensation, the basis for compensation is a shift of blood volume between arterial and venous circulation, thereby altering preload and SV. |
True.
p. 285 |
|
|
True or False:
Regarding Frank-Starling Compensation, compensation operates over several beats and is NOT complete. |
True
p. 285 |
|
|
With cardiac function curves, which of the following is NOT held constant to isolate effects of right atrial pressure on cardiac output?
A. afterload B. contractility C. TPR D. HR |
A. afterload
Afterload (aortic pressure) is allowed to vary as a function of flow (CO). p. 286 |
|
|
The steepest part of the cardiac function curve is between RAP values of...
|
0 - 4 mmHg
(note: @ RAP greater than or equal to 7 mmHg, CO reaches a plateau) p. 287 |
|
|
What accounts for the plateau in the cardiac function curve?
|
1. increased afterload offsets increased preload.
2. Pericardium is rather inelastic and limits EDV. |
|
|
If a positive inotropic effect occurs, what happens to the cardiac function curve? Specifically, what happens to SV and CO, respectively?
|
+ inotropic effect means increase in contractility. That means increase in SV and increase in CO!
Cardiac function curve will shift to Left and become slightly steeper. p. 288 |
|
|
If a negative inotropic effect occurs, what happens to the cardiac function curve? Specifically, what happens to SV and CO, respectively?
|
- inotropic effect means decrease in contractility. That means decrease in SV and decrease in CO!
Cardiac function curve will shift to Right and become slightly less steep. p. 288 |
|
|
If TPR increases, what happens to the cardiac function curve? Specifically, what happens to SV and CO, respectively?
|
If TPR increases, aortic pressure (afterload) increases, SV decreases, and CO decreases. The cardiac function curve will shift slightly to the R and be slightly less steep. p. 288
|
|
|
If TPR decreases, what happens to the cardiac function curve? Specifically, what happens to SV and CO, respectively?
|
If TPR decreases, aortic pressure (afterload) decreases, SV increases, and CO increases. The cardiac function curve will shift slightly to the Left and be slightly steeper. p. 288
|
|
|
At a constant SV, an increase in HR must increase CO. At HR > _____ bpm, diastole is too brief for complete filling and EDV is reduced but it is not until ~ _____ bpm that CO peaks (under conditions used to obtain the cardiac function curve).
|
100bpm; 125 bpm
p.288 |
|
|
True or False:
At resting HR, atrial contraction has only a minor effect on EDV (5%). |
True.
p. 288 |
|
|
True or False:
The time for diastolic filling of ventricle is inversely proportional to HR. |
True. At HR less than or equal to 100 bpm, filling is complete. At HR > 100 bpm, filling is incomplete. At HR > 125, CO starts to fall.
p. 289 |
|
|
True or False:
When a normal heart is in circulation, it is primarily the properties of the vascular system which determine the cardiac output. In contrast, during heart failure, both the heart and vascular system determine cardiac output. |
True
p. 292 |
|
|
When a normal heart is in circulation, it is primarily the properties of the vascular system which determine the cardiac output. When would both the heart and vascular system determine cardiac output?
|
with heart failure
p.292 |
|
|
True or False:
The "knee" of the vascular function curve is a consequence of the negative pressures in the thoracic cavity. |
TRUE. p. 296
|
|
|
True or False:
The "knee" of the vascular function curve is a consequence of the negative pressures in the thoracic cavity. |
TRUE. p. 296
|
|
|
What would change the slope of the vascular function curves?
A. changes in contractility B. changes in HR C. changes in TPR |
C. changes in TPR!
remember the equation: Venous return = -[(Cv/Ca)+1] / TPR * (Pv-Pms) p. 295-6 |
|
|
What are two ways to increase stressed blood volume?
|
1) Increase in total blood volume (transfusion) --> increase in stressed blood volume --> increase Pms.
2) Increasing venoconstriction. The other way to change stressed volume is to change the amount of blood subjected to stress! This too leads to an increase in Pms. p.298 |
|
|
What would increase Pms (mean systems pressure)?
A. decrease in blood volume B. increase in blood volume C. venoconstriction D. venodilation |
B. increase in blood volume
C. venoconstriction p. 298 |
|
|
What would decrease Pms (mean systems pressure)? (2)
A. decrease in blood volume B. increase in blood volume C. venoconstriction D. venodilation |
A. decrease in blood volume
D. venodilation p. 298 |
|
|
True or False:
Positive changes in the cardiac function curve under resting circumstances produce little change but negative changes in the cardiac function curve create substantially profound effect of increased right atrial pressure. |
True.
p. 306-7 |
|
|
Positive changes in the cardiac function curve under resting circumstances produce [ little / substantial ] change and negative changes in the cardiac function curve create [little / substantial ] change of increased _______ .
|
+ CFC change --> little change in RAP
- CFC change --> SUBSTANTIAL change in RAP p. 307 |
|
|
True or False:
Elevated right atrial pressure are strong clinical indicators of heart failure. |
True. Because this means the heart is less able to transfer blood from the veins to the arteries and hence the higher right atrial pressure and lower vascular flow rate. p. 307
|
|
|
Inotropic changes shift the [ Cardiac Function Curve / Vascular Function Curve ] thus affecting the [ CO / RAP ] whereas changes in blood volume shift the [ Cardiac Function Curve / Vascular Function Curve ] thus affecting the [ CO / RAP ].
|
Inotropic changes --> change in CFC --> change in RAP.
Blood volume changes --> change in vascular function curve --> change in CO. p. 308 |
|
|
Quickly sitting/standing up and feeling faint due to gravity's force on venous return is a condition referred to as...
|
orthostatic hypotension
p. 310 |
|
|
Inspiration [ decreases / increases ] venous return to the right heart and [ decreases / increases ] right heart output.
|
both increase! why? During inspiration, the pressure within the thorax and around the heart decreases, thus increasing transmural pressure and thus flow of blood into ventricles. p. 311
|

