![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
112 Cards in this Set
- Front
- Back
|
Where are bile salt reaborbed?
|
the terminal ileum
|
|
|
What is the #1 and #2 most common cause of physician visits?
|
1. respiratory
2. abdominal pain |
|
|
How long is the live GIT compared to one in a cadaver?
WHy? |
half as long due to tonic contraction
|
|
|
What makes up the biliary system?
|
gallbladder to produce and liver to store
|
|
|
3 reasons why it's important to keep GI contents in the tube?
|
ph=2
lots of enzymes that will digest us lots of microorganisms that will infect us |
|
|
Where is most of the fluid absorbed?
|
the SI
|
|
|
What is absorbed in the LI? Where does that go?
|
fluid, which goes to the kidney
|
|
|
WHat gets left in our poop?
|
small amount of undigested food, microorganisms, and sloughed off cells
|
|
|
What is the RMP of the intestines? What layer is this in?
What cells are responsible for this? What is their category? What ions come in an out to make this? |
oscillating slow wave potentials from muscular pacemaker cells in the muscular layer (that actually does the cntractions)
The interstitial cells of Cajal do this. They let some Ca2+ come in and then some K+ goes out. |
|
|
When do you get action potentials in the slow waves?
What determines the frequency of contraction? What is the frquency of contraction in the stomahc vs duodenum vs colon? |
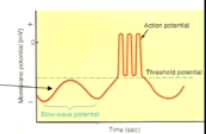
contraction everytime a peak goes over the threshold.
stomach- 3/min duodenum- 12/min colon- 8/min |
|
|
WHat happens to slow waves whe inhibitors chemicals are released?
Give an example of an inhibitory chemical. |
NO- waves are now below threshold and either freq is lower or the muscle is completelly relaxed
|
|
|
What are the layers of the GiT referred to as?
How do they change/stay the same throughout the GI? |
tunics
they are present throughout, but have specializations in each part of the tract |
|
|
What are the 4 layers of the GIT?
|
1. mucosa.
2. submucosa 3. muscularis externa 4. serosa |
|
|
Name the layers of the mucosa and the functions of each.
|
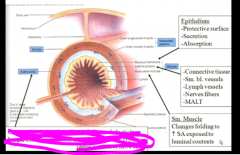
|
|
|
Give the fx of the submucosa
What is the plexus there called |
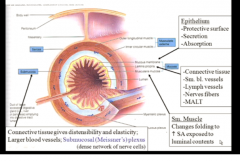
keeps the GI together- used to be used for sutures (cattle gut)
contains the submucosal plexus (meissner's) |
|
|
So what mediates changes in the folds vs peristalsis?
|
fold- muscularis mucosa
peristalsis- muscularis externis |
|
|
What are the two types of muscle in muscularis externia? Which one is more on the inside?
What is the exception to the two layer rule? |
longitudinal and circular, with circular more on the inisde
in stomach, there are 3 layers |
|
|
What plexus (give name and nickname) is in the muscular layer?
|
myenteric (muscle-gut)/ Auerbach's plexus
|
|
|
Why is the serosal layer called serosal?
What two fx does it serve. |
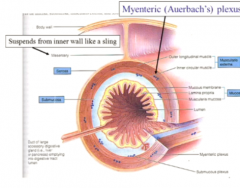
it secretes serious fluid so the intestines can glide up against one another.
also it hangs the gut like a sac. |
|
|
WHat are the 2 actions of the PS NS and 3 actions of the S NS on the GIT?
|
PS- activate secretion and motility
S- INctivate secretion and motility and constrict blood vessels |
|
|
Is the intrinsic or the extrinsic NS more important? WHy?
|
intrinsic
extrinsic (autonomic only modifies the intrinsic by telling it to be more excitatory or inhibitory) |
|
|
another name for the intrinsic GI NS?
What territory does it innervate? WHat territory does the vagus innervate? |
the enteric NS
it innervates from mid esophagus to the external anal sphincter vagus does mid esophagus to the transverse colon |
|
|
Can out Gi tract function without the autonomic?
WHat two structures make it up? |
yes! the myenteric and the submucosal.
|
|
|
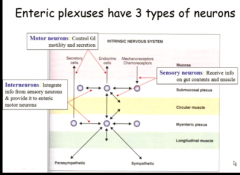
describe the 3 types of cells in the enteric NS (ENS)
|
|
|
|
What NT's do PS neurons give to the ENS?
|
ACh and substance P
|
|
|
What stimulus is taken up by sensory neurons?
WHat cell releases this? |
serotonin released by enteric chromaffin cells when they detect mechanical, chemical stimulation in the luman
|
|
|
What is one side effect of taking SSRI's then? Mechanism?
|
HYPER MOTILITY OF PERISTALSIS
too much stimulatory signals from the GI to proceed with food processing nausea, vomiting, and constipation |
|
|
What two muscular activities does the sensory neuron stimulate when it gets serotonin signals?
|
relaxation in front of the tube
contraction behind peristalsos! |
|
|
What are the inhibitory transmitters of the NS?
|
NE and vasoactive intestinal peptide (VIP)
|
|
|
now we talk about NT's and NM;s!
Name all the fx of ACh! What is it released by? |
1. relax sphincters and contract longitudinal
2. increase salivary, gastric, and pancreatic secretion |
|
|
All 2 fx of NE
What is it released by? |
1. relax longitudinal and constrict sphincter
2. decrease salivary secretions |
|
|
All fx of VIP. Summarize what it does.
WHat is it released by> |
it is a mixed bag
it relaxes SM, but increases all secretions after the esophagus (gastric, intestinal, and pancreatic) release by neurons of the mucosa and SM |
|
|
fx of substance P.
WHta is it released by? |
it is an adjuct to ACh and is always secreted in the same vesicle.
it aids with contraction of SM and increases salivary secretions |
|
|
What can you say about the more adjunct neurotransmitters/modulators in their control of muscle and secretion.
|
Both VIP and substance P will increase secretion, but in different places. SP handles the mouth.
they differ in their influence on contraction completely howeber. |
|
|
Now we talk about the hormones
What is a common fx of a hormone that is secreted in a specific area? What happens if there is too much or too little of it locally? |
they tend to maintain that area.
too little- atrophy too much- hyperplasia |
|

|

|
|
|
What is the aim of gastrin's motility fx?
|
to move food through form the stomach to the SI
and to let previous food sitting in the SI go to the colon |
|
|
WHat phenomenon does this explain?
|
why you need to poop shortly after you eat
|
|
|
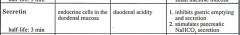
summarze the purpose of secretin
|
nature;s antacid- neutralizes stomach acid and tells stomach when too much is in the SI so it can stop passing it
|
|
|
|
|
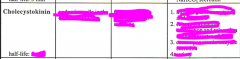
Dissect Chole-cysto-kinin
What should you automatically associate it with? |
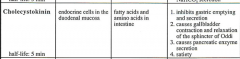
bile-bladder-contraction
think about fat when you think about CCK |
|
|
WHat is the sphinter of Oddi?
|
the final sphincter in the common bile duct to let all that bile in
|
|
|
sum up actions of CCK
|
it prevents too much food from coming into the SI (by delaying the stomach and telling us to stop eating) and also stimulates enzymes to digest protein and fat (especially fat)
|
|
What should you automatically associate this with?
|

glucose and insulin
|
|
|
When does GIP stimulate insulin release?
|
before the glucose even reaches the blood
|
|
|
What would happen to swallowing food if we had no bolus from saliva?
|
we would aspirate the tiny particles
|
|
|
What is the composition % of saliva?
|
99% serious with enzymes
1% mucous with mucin |
|
|
What are the enzymes in saliva? Are they important for digestion?
What is the composition of saliva secreted by each salivary gland? |
a-amylase and lipase- totally not important
they all secretes serous enzymes and mucin except for the parotid which only does serious with enzymes |
|
|
What pH is saliva? WHy is this good?
|
alkaline to protect against acidic erosion from sugar breakdown and gastric regurgitation
|
|
|
How does saliva serve an immune function?
|
it has antimicrobials in it.
|
|
|
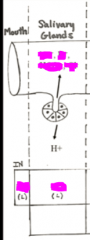
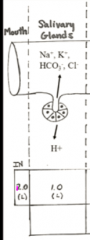
What is the 2 stage model of salivary secretion?
WHat cells are responsible for each stage? |
primary secretion of electrolytes- acinar cells
secondary secretion is modification of primary- duct cells |
|
|
Where do we borrow the primary secretion from? Were does it get put back?
Why may this be important in fluid balance pathology? |
the blood
if we vomit or have diarrhea, we don't have a chance to replace the electrolytes we borrowed |
|
|
imagine the channels necessary to create the priimary secretion?
How can you tell where the basolateral membrane is? What enzyme is in the acinar cell? |
the Na/K pumps are in the basolateral side
carbonic anhydrase is inside the cell to create the bicarb for alkalinity |
|
|
What other liquid does the primary secretion look like?
WHat is modified in secondary? |
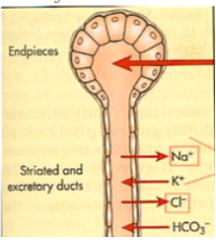
it looks like plasma.
Na and Cl are taken back from it |
|
|
What is the purpose of reabsorbing Na and Cl? What are we putting in at the same time?
How are we able to absorb more? |
to make a alkaline and hypotonic solution
hypotonic so that when salt does come in, we can taste it. we put in bicarb and K+ the slower saliva flows, the more hypotonic it becomes |
|
|
What hormone can act to modulate the salivary secretion here and accentuate the duct cell activity?
|
aldosterone! (it does the same thing in the renal tubules)
|
|
|
What is the major control of salivary secretion?
|
PS stimulation
|
|
|
describe the mechanism by which the PS NS does this
|

|
|
|
does aldosterone create more or less saliva?
|
neither, it only modifies the composition
|
|
|
What kind of disease is Cevimeline used for?
Who has this disease? |
schogren's disease for people who have autoimmunity against the tear and salivary ducts. they get xeropthalmia and xerostomia.
Venus Williams has this |
|
|
What are the two ways in which CEvimeline works?
what receptor does it act on? |
it increases the salivary secretion by the acinar and duct cells and dilates blood vessels so that it can pull more
|
|
|
What is the second messenger system by which the S NS affect salivary secretion?
What are the two effects it mediates? What is the overall effect? |
NE binds to B receptors --> increase cAMP via Gs --> increase enzyme exocytosis
overall this makes a more enzyme rich saliva also it costricts blood vessels to decrease saliva volume overall creases less, but ore enzyme rich saliva |
|
|
What would the saliva of a nervous vs very calm person be like?
|
nervous- S NS- it would be very low flow and thick
calm- PS NS- it would be flowing like a fountain |
|
|
Why would it be thick?
|
it would have a high mucous content
|
|
|
What is the effect of vomiting on the salivation rate?
smoking? sleep? fear? dehydration? fatigue? |
vomiting and smoking increases it to protect the mouth
sleep- circadian rhythm decreases it dehydration and fatigue- you don't have the fluid or energy to do it |
|
|
So why do I wake up with such a dry mouth every morning?
|
my circadian rhythm hormones will decrease my salivation
|
|
|
What are some diseases that can alter saliva production? procedures? Why?
|
sjodrens and cystic fibrosis can decrease it
radiation can destroy saliva glands |
|
|
how many exocrine glands does cystic fibrosis affect?
|
all of them!
|
|
|
What happens to saliva production as we age?
What augments this? |
it decreases because all processes decrease
medication side effects increase this effect |
|
|
give 2 examples of medications that would decrease saliva?
|
atropine/glycoprrole- anti cholinergic
isoroterenol- sympatpmimetic |
|
|
What happens to taste buds when we age?
what behaioral changes does this result in? |
we lose them so we tend to overuse salt and sugar as we age
|
|
say what ions and what volume of water comes in and out of the GIT here
|
|
|
|
What is the muscle composition of the different parts of the esophagus?
|

|
|
|
What kind of secretions does the esophgeal epithelium give?
|
mucus
|
|
|
What is the upper esophageal sphincter (UES) vs the LES controlled by?
|
UES- volunrary
LES- autonomic and enteric NS |
|
|
What is reponsible for tone of the GIT?
WHat is the purpose of tone? |
cross bridge actions of actin and myosin
it will keep pressure o contents and prevent over distension and outpouches |
|
|
What are the two types of disgestive motility superimposed on tone?
give an example of each. |
propulsion- sequential contraction- peristalsis
mixing- non sequential- segmentation |
|
|
What are the 3 phases of swallowing?
|
oral, pharyngeal, and esophageal
|
|
|
ORAL PHASE
describe the voluntary phase of the oral swallowing and then the reflexive part. |
voluntary- we chew food into a bolus and use our tongue to push it back
reflex- CN 9 detects the pressure in the back of the oropharynx and takes this to the swallowing center (nucleus ambiguus) to activate CN 9 and 10 to swallow |
|
|
PHARYNGEAL PHASE
how long does this phase last? describe the muscle activity in the pharyngeal phase. what are the three goals? |
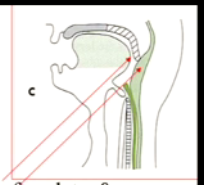
1 second
prevent food from going to the nose- your soft palate lowers peristalsis- there are superior constricters in your pharynx. These constrict to propel the bolus down let food into the esophagus- relax the UES to receive bolus |
|
|
besides swallowing, what other efferents are sent down by the swallowing center that is initiated by
|
vagal efferents to initiate the digestive process as a whole
|
|
|
What is the relaxation down stream called?
|
receptive relaxation to recerive the food
|
|
|
ESOPHAGEAL PHASE
how long does it last? describe when sphincters contracts and relaxes in this phase. |
5-10 seconds
UES is closed, but opens when the bolus is knocking, and closes right after it passes The swalloowing center tells the LES to relax (receptive relaxation) to anticipate the bolus and it closes right after it passes |
|
|
Describe primary and secondary peristalsis in the esophageal phase.
how strong is peristalsis? |
primary- to push bolus down
secondary- MAY happen after bolus passes to remove any remaining debris peristalsis is strong enough to happen upside down |
|
|
Give an example of when secondart peristalss would happen. WHat would the stimulus be?
|
when you have a pill stuck in your throat.
the distention triggers another wave of peristalsis from the swalllowing center |
|
|
what is the resting pressure of the UES and LES?
What is responsible for it? What mechanism causes them to relax? |
30 mmHg both because they are tonically contracted due to myogenic and neurologic factors
NO secreted by the vagus nerve |
|
|
What disease do we have when the LES isn't working right?
|
GERD
|
|
|
What are some mechansisms (not causes yet) that can cause GERD? (4)
|
1. chemical relaxation of the LES
2. increased pressure below the LES 3. failure to neutralize or remove acid in esophagus 4. Loss of reflex closure of the LES |
|
|
What did Dr. Podolin do to get her GERD?
|
became pregnant and played a lot of squatting racket ball
|
|
|
What are some chemicals that can relax the LES?
|
anything that is either sympathomimetic or anticholinergic
smoking, CCK (fat ingestion) |
|
|
What are some causes of increased pressure below the LES?
|
any kind of abdominal pressure
pregnancy, obesity, ascites, squatting, constrictive clothing |
|
|
Wha are some causes of loss of the normal LES closure reflex?
|
hiatal hernia, muscle atrophy, dennervation
|
|
|
What can be some causes of an inability to clear acid from the esophagus?
|
poor peristalsis
low saliva procuction (sjogren's syndrome) being supine for too long |
|
|
What is achalasia? nickname?
WHat is the mechanism? the cause? WHat NT;s are incolved? |
bird beak - food accumulates
the LES fails to relax because there is a loss of neurons that secrete NO and VIP (myenteric plexus is fibrosed) food gets stuck in the esophagus |
|
|
What happens to the esophagus as we age?
what are we more at risk for disease wise? |
more fibrosis, less muscle
it get stiffer, but with less muscle and peristalsis the LES relaxes more (less tonic activity) so we have a tendency toward GERD |
|
|
What is the main purpose of the stomach?
|
storage
|
|
|
|
|
|
What two parts of the stomach are histologically the same?
What distinguishese these regions from others? |
the fundus and the body
they both have very thin muscle, but a lot of thick mucosa folds called rugae |
|
|
mnemonic for the part of the stomach where food enters and where it exits.
|
cardia- closer to the heart
pyloric- literally means "gatekeeper" because it blockd back the majority of the food from the GI |
|
|
What is the wall of the pyloric antrum differet?
what happens in the pyloric sphincter? |
it becomes muscular and smooth for gatekeeping
in the sphincter, the circular muscle becomes especially thick |
|
|
|
|
|
Where do gastrin and secretin go after being secreted? Why?
|
into the blood because they are hormones
|
|

mnemonic for which cells go where
|

chief cells sit in the center of the pit because they rule the whole joint
parietal cells are their right hand man mucous neck cells make up the neck (as opposed to the head) epithelial cells are always on the surface |
|
|
What is a special fx of the mucous neck cells? do they secrete anything?
what is their nickname> |
they can migrate up and down the duct to become new cells, which is important for cell turnover.
no secretions aka parent cells becayse they give birth to new cells |
|
|
how often is the stomach lining turned over?
|
every 3 days
|
|
mnemonic for what secretes what
|
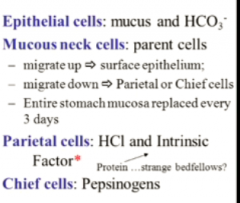
chief cells- important enzyme of the stomach
parietal cells- will always help with everything so HCL to activate pepsinogen and IF to help later absorb B12 epithrlial cells- always trying to protect our linings |
|
|
Why would the epithelial cells secrete bicarb if there is also so much acid being produced?
|
they secrete it underneath the mucus as a protective layer for the mucosa
|
|
|
What is the arrangement of mucous and bicarb here known as? Why?
|
the unstirred layer because they don't mix to prevent the acid from neutralizing the bicarb
|
|
|
What stimulates pepsinogen secretion?
is this necessary to digest protien? |
the cephalic and gastric phase from vagal- ACh stimulation
so just thinking about eating will stimulate it and the n the actual food will too it is totally not necessary for protein difestion |
|
|
What stimulates IF to be secreted?
How does it help the B12 absorption? |
B12 stimulates it
IF will cause B12 to dissocate from it's complex and bind with it. Together they can be absorbed |
|
|
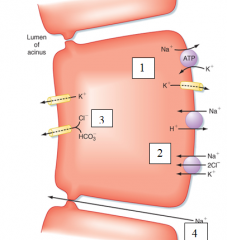
describe the ion channels in the parietal cell that allow it to secrete HCl
|

very ATP dependent K+/H pump
|
|
|
What happens to the pH of the blood leaving the stomach? Where is this cancelled out?
|
there is an alkaline tide, which is neutralized when the blood passes the pancreas
|

