![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
32 Cards in this Set
- Front
- Back
|
- What is Osteoarthritis (OA) also known as? - Is it a primary or secondary disease? (What is the difference between the two? - How many area affected? |
- degenerative joint disease - Can be both (Primary = no cause is known, secondary = a cause is known (ex: trauma, infection) - 27 million, most common rheumatic disease |
|
|
- What are common risk factors? (6) - What two groups are most at risk? - Does it typically affect individual joints, or groups of joints? - Is it inflammatory? |
- heredity, obesity, anatomic joint abnormality, injury, reduced muscle strength, work/leisure leading to overuse of joints - Those over the age of 65 and females - Individual joints, typically on dominant side (ex: you can have it in one knee and not the other) - OA itself is non-inflammatory, though inflammation caused by joint damage is common |
|
|
- What is the process leading to OA |
Two Steps: 1) Breakdown of articular cartilage in joints, causing softening and stiffening; then cartilage wears away causing bone on bone contact (painful, causes crepitus) 2) Reactive bone formation of osteophytes (bone spurs) where ligaments and capsule attach to bone (bone thickens); bone loses its normal shape; cysts form |
|
|
What are symptoms of Osteoarthritis
|
- Morning stiffness (less than 30 min) - Crepitus: audible/palpable crunching or popping in joint caused by irregular cartilage surfaces - Joint pain - Gelling: stiffness after periods of inactivity - Joint enlargement and/or deformity - Clinical symptoms: pain with barometric pressure changes, "i can tell it's going to rain today" |
|
|
- Osteoarthritis diagnosis (3 ways) - What criteria for diagnosis do some doctors adhere to? |
-1 Patients history is taken and physical exam is done by physician - 2 X-ray to confirm clinical diagnosis. Will show osteocyte formation at the joint margin, joint narrowing, subchondral bone sclerosis - 3 MRI can provide closer look at joint damage - Some doctors adhere to specific criteria for diagnosis, such as American college of Rheumatology Criteria |
|
|
How is osteoarthritis medically managed? (7)
|
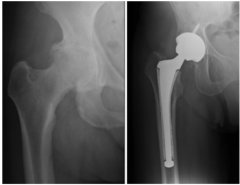
- Non-steroidal anti-inflammatory drugs (NSAIDs) - Analgesic agents - Corticosteroids - Disease-Modifying Antirheumatic Drugs - Biological Response Modifiers - Surgery, such as joint replacement, arthroscopic joint debridement, cartilage grafts, joint fusion - Ergonomic evaluation |
|
|
- Define systemic - Define auto-immune |
- Affects more than just one area (ex: joints, heart, eyes, etc. - Body attacks itself, destroys tissues |
|
|
-What is rheumatoid arthritis (high level)? - Who is at the highest risk (2) - About how many Americans are affected by it? |

- Chronic, systemic auto-immune inflammatory condition, where synovial tissue secretes matrix-degrading enzymes "pannus" into synovial fluids, which attacks the joint lining causing synovitis - People between 40-70 years old and females - 1.5 million americans per year |
|
|
- What are symptoms of Rheumatoid arthritis?
|
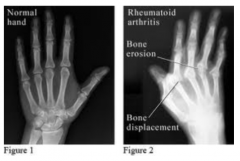
- MAIN: Joint swelling due to excess synovial fluid, enlargement of synovium and thickening of joint capsule. This weakens the joint capsule and stretches ligaments and tendons attached. - Secondary: Fatigue, Red/hot/swollen/stiff joints, symmetrical joint pain (pain in same joint on both sides), fever, anemia, weight loss, limited independence with ADL/IADL, depression, pulmonary hypertension, renal dysfunction, gastrointestinal bleeding, pericarditis, chest pain, SJOGREN's Syndrome, skin rashes |
|
|
- How is RA diagnosed
|
- Mostly by Rheumatoid Factor Antibody (70-90% of those with it have it) - High erythrocyte sedimentation rate (indicates presence of inflammatory process) X-ray: shows progressive joint destruction |
|
|
- What is the American College of Rheumatology Criteria for having RA
|
- Demonstrate 4 of the following: 1. Morning stiffness 2. Arthritis of three or more joint areas 3. Arthritis of hand joints (swelling) 4. Symmetrical arthritis 5. rheumatoid nodules 6. Serum rheumatoid factor 7. Radiographic changes |
|
-How does RA typically affect the joints? - Who is the best person to refer someone to who may have RA |
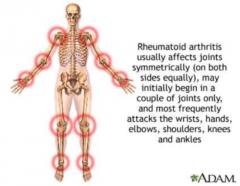
- Process IS symmetrical, however one side can be affected more than another - Joint deformities occur in about 33% of the people diagnosed w/ RA - Best person is Rheumatologist, not general practitioner |
|
|
- What is the process of RA
|
- Process varries - 20% have single episode than remission (monocyclic) - Most experience a series of flares than remission(Polycyclic) - Some experience unremitting increase in severity of symptoms (progressive) |
|
|
What are the two stages of disease process that the American College of Rheumatology Classifies RA
|
- Stage 1: Early: no destructive changes on x-ray but osteoporosis may be present - Stage 2: Moderate: x-ray shows osteoporosis and possibly subchondral bone and/or cartilage destruction; limited joint mobility, muscle atrophy, possible nodules and tenosynovitis - Stage 3: Severe: X-ray evidence of cartilage and bone destruction, soft tissue lesions plus stage 2 criteria - Stage 4: Terminal: Fibrosis or bony anklyosis plus Stage III criteria |
|
|
What are some common deformities with Rheumatoid Arthritis -late stage (3)
|
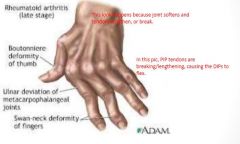
|
|

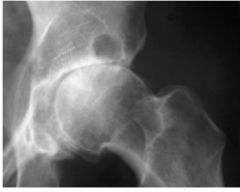
What sort of RA condition are we seeing here?
|
Wrist Subluxation (partial dislocation of the wrist)
|
|
|
- Is there a cure for RA? - What type of medical treatment is given for RA (10)? |
- No cure - Treatment 1.) Reduce pain, swelling, fatigue 2.) Improve joint function/minimize deformity (deformity is hard to correct once its happening) 3.) Prevent disability and morbidity (disease) 4.) Maintain physical, social and emotional function while minimizing long-term toxicity from medications 5.) Medication (managed by rheumatologist) 6.) NSAIDS (rarely used alone, reduce joint pain/swelling, don't alter disease progression) 7.) Corticosteroids - awesome, but bad side effects 8) DMARDS (disease-modifying anti-rheumatic drugs) - used early to alter disease course 9.) Biologic drugs - when DMARDS don't work 10.) Surgery |
|
|
- What is fibromyalgia - How many are affected/who is most common group affected/what is peak onset - What are common symptoms that occur together |
- Common musculoskeletal illness - 5 mill Americans/women/40-55 yrs old 1.) Decreased pain threshold or tender points 2.) incapacitating fatigue 3.) Widespread pain 4.) Anxiety depression |
|
|
What are other common symptoms of fibromyalgia
|
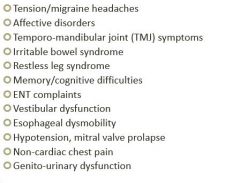
|
|
|
What are fibromyalgia points of pain?
|
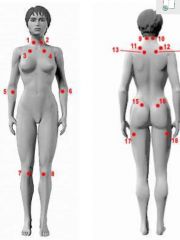
|
|
|
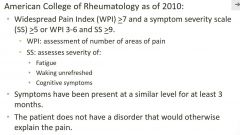
- What does the American College of Rheumatology define as the fibromyalgia diagnostic criteria? - How long may symptoms be present for? - What are some physical symptoms associated with fibromyalgia? This are what brings a patient to OT, they don't know they have FM/a |
- Trigger finger, tendonitis, joint sprains, nerve impingement, bone fractures
|
|
|
- What does the test for fibromyalgia (FM/a) look for? - What are common medications used for treating it? |
- White blood chemokine and cytokine patterns. People with FM/a have deregulated patterns of this. 1.) Lyrica - nerve pain 2.) Cymbalta and Savella (serotonin and norepinephrine reuptake inhibitors SNRIs 3.) Antidepressents |
|
|
- What theories exist about the etiology of FM/a
|
unknown- Cause is unknows, many theories exist - Hormonal or chemical imbalances/neuroendocrine abnormalities disrupt how the nerves signal pain - Traumatic event or chronic stress can increase susceptibility - Lack of sleep - Many call it a "somatization disorder" (mental, in the person's head) - Probably result of multiple causes |
|
|
- Might fibromyalgia present itself - Is there a cure? |
|
|
|
- What does an OT look for in their evaluation of someone with a Rheumatic disease?
|
- Client history with illness and medical mgmt - Occupational history, degree of debility w/ ADL and IADL - Activity diary - Cognitive, psychological and social status - Clinical status (ex: inflammation, ROM, strength, hand function, stiffness, pain, sensations, joint instability) |
|
|
OT Intervention: Rheumatic Disease - What can be done to relax muscle spasm resulting in joint dysfunction - Can joint mobilization be done? - Would someone with FM/A want to use a myofascial releases or trigger point release - Are modalities good for pain relief? What are some precautions? |
- Soft tissue mobilization and stretching - Minimal with OA and FM/a, but not with RA due to disease process - Myofasical due to hypersensitivity to touch - Yes, but heat shouldn't be used with significant inflammation, and cold shouldn't be used with RA |
|
|
- What therapeutic exercise is good for people with rheumatic disease? (what is best type)? - What is essential for success of therapeutic exercise? - What is a precaution? |
- strengthening and aerobic/AROM is best - with pain tolerance - Home exercise programs - Pain lasting 1-2 hours after exercise indicate need to decrease intensity of program |
|
|
- Is splinting good for people with rheumatic disease? What type? - What does splinting require? - What is the wearing schedule? |

- Yes, for inflammation and joint immobilization (static) - Doctors orders - Varies based on purpose and degree of inflammation |
|
|
- Why is education important for people with rheumatic disease?
|
- So they know disease progression, can adjust their life based on progression and to know the importance of doing OT
|
|
|
What are important precautions when dealing with rheumatic disease
|
- Respect pain, balance activity and rest, - Use larger, stronger, non-affected joints when possible - Avoid staying in one position for long - Use joints in good alignment - Maintain proper weight - Hands: avoid tight grasp, use both hands, avoid repetitive activities, avoid pressure to tip of thumb - Simplify daily activities - Do ergonomic analysis for home and work environment |
|
|
What works/doesn't work with people with - Fibromyalgia - Rheumatoid Arthritis - Osteoarthritis - What affects any therapy with these patients? |
- Stretching for reduce muscle spasms/manual therapy - cant tolerate - splinting-prevent deformity/manual therapy or cold packs due to nodules and joint destruction - strengthening - reduces pain/cold pacs - inflammation - can make therapy non productive |
|
|
What does evidence say about - Fibromyalgia - Osteoarthritis - RA |
- Aerobic exercise and patient education best - Increased physical activity and strengthening - Aerobic capacity - people with RA can increased aerobic capacity but not likely muscle strength |

