![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
92 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Cross-tolerance
|
There is a decrease in response to one drug due to exposure to another drug. It is observed in treatment with antivirals, antibiotics, analgesics and many other medications.
|
|
|
|
Cross tolerance and opioid
|
exists among the opioid agonists (eg, oxycodone, methadone, fentanyl, codeine, heroin). Accordingly, individuals tolerant to one of these agents will be tolerant to the others. No cross-tolerance exists between opioids and general CNS depressants (eg, barbiturates, ethanol, benzodiazepines, general anesthetics).
|
|
|
|
Major established risk factors for Alzheimer’s disease
|
b. Advancing age
c. Family history |
|
|
|
Possible risk factors for Alzheimer's Disease
|
e. Female
f. Head injury g. Low educational level h. Production of apoE4 i. High levels of homocysteine j. Nicotine in cigarette smoke |
|
|
|
Drugs for mild to moderate Alzheimer's Disease
|
Cholinesterase inhibitors
(donepezil, galantamine, rivastigmine, and tacrine) Prevent breakdown of ACh Help to slow progression of disease |
|
|
|
Drug for severe Alzheimer's Disease
|
Memantine
a. First drug in a new class, the NMDA receptor antagonists b. Indicated for moderate to severe AD c. Better tolerated than cholinesterase inhibitors e. blocks neuronal receptors for NMDA (N-methyl-D-aspartate) |
|
|
|
Adverse effects of Cholinesterase Inhibitors
|
b. GI Gastrointestinal effects—nausea, vomiting, dyspepsia, diarrhea—occur often.
a. Dizziness b. Headache c. Bronchoconstriction d. Liver injury (tacrine) |
|
|
|
Addiction
|
a behavior pattern characterized by continued use of a psychoactive substance despite physical, psychologic, or social harm.
|
|
|
|
Physical dependence
|
a state in which abrupt discontinuation of drug use will precipitate a withdrawal syndrome.
|
|
|
|
minimum effective concentration (MEC)
|
the plasma drug level below which therapeutic effects will not occur.
|
|
|
|
toxic concentration
|
The plasma level at which toxic effects begin
|
|
|
|
Lithium levels
|
must be kept below 1.5 mEq/L; levels greater than this can produce significant toxicity.
|
|
|
|
For initial therapy of a manic episode
|
lithium levels should range from 0.8 to 1.4 mEq/L.
|
|
|
|
maintenance lithium levels
|
0.4 to 1.0 mEq/L
|
|
|
|
lithium determinations should be drawn
|
in the morning, 12 hours after the evening dose
|
|
|
|
benzodiazepines for muscle spasms
|
diazepam, clorazepate
|
|
|
|
benzodiazepines for Alcohol Withdraw
|
Chlordiazepoxide [Librium], diazepam, lorazepam, Oxazepam
|
|
|
|
benzodiazepines for Panic Disorder
|
Alprazolam [Xanax, Niravam], clonazepam [Klonopin], and lorazepam [Ativan]
|
|
|
|
benzodiazepines for Perioperative Applications
|
diazepam [Valium], lorazepam [Ativan], and midazolam [Versed]—are given IV for induction of anesthesia.
|
|
|
|
benzodiazepines for Insomnia
|
Estazolam, Flurazepam, Oxazepam, Temazepam, Triazolam
|
|
|
|
benzodiazepines for seizures
|
diazepam, clonazepam, lorazepam, and clorazepate
|
|
|
|
Adverse reactions of Benzodiazepines
|
CNS Depression
Anterograde Amnesia Sleep Driving and Other Complex Sleep-Related Behaviors Paradoxical Effects Respiratory Depression (weak depression) Abuse severe allergic reactions including angioedema and anaphylaxis. |
|
|
|
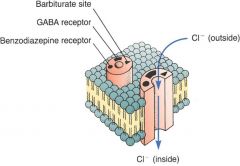
Benzodiazepines Molecular mechanism of action
|
– Potentiate the actions GABA
– Are much safer than Barbituates Benzodiazepine-Like Drugs |
|
|
|
Zolpidem [Ambien]
|
– Sedative-hypnotic
– Short-term management of insomnia Benzodiazepine-Like Drugs |
|
|
|
Zaleplon [Sonata]
|
– New class of hypnotics, pyrazolopyrimidines
– Short-term management of insomnia – Prolonged use does not appear to cause tolerance Benzodiazepine-Like Drugs |
|
|
|
Eszopiclone [Lunesta]
|
– Is the S-isomer of zopiclone
– For treating insomnia – No limitation on how long it can be used Benzodiazepine-Like Drugs |
|
|
|
Antidepressant classifications
|
Tricyclic antidepressants
Selective serotonin reuptake inhibitors (SSRIs) Serotonin/norepinephrine reuptake inhibitors (S/NRIs) Monoamine oxidase inhibitors (MAOIs) Atypical antidepressants Electroconvulsive therapy Vagus nerve stimulation |
|
|
|
TRICYCLIC ANTIDEPRESSANTS (TCAs) - Pharmacokinetics
|
Long and variable half-lives
– Usually single daily dose – Requires individualization of dosage |
|
|
|
TRICYCLIC ANTIDEPRESSANTS (TCAs) - Therapeutic uses
|
• Depression
• Bipolar disorder • Neuropathic pain |
|
|
|
TRICYCLIC ANTIDEPRESSANTS (TCAs) - Adverse Effects
|
• Orthostatic Hypotension
• Sedation • Anticholinergic Effects (Think Atropine) – Block muscarinic receptors – Dry mouth – Blurred vision – Urinary Retention – Constipation – Tachycardia – Asthma |
|
|
|
Neurotransmission without TCA
|

|
|
|
|
TRICYCLIC ANTIDEPRESSANTS (TCAs) - Drug Interactions
|
• Monoamine oxidase inhibitors
• Direct-acting sympathomimetic drugs • Indirect-acting sympathomimetic drugs • Anticholinergic agents • CNS depressants |
|
|
|
TRICYCLIC ANTIDEPRESSANTS (TCAs) - Preparations and Drug Selection
|
• Nine equally effective tricyclic antidepressants (TCAs)
• Selection based on side effects For the exam remember: Initial response is 1-3 weeks Maximal response 1-2 months |
|
|
|
SELECTIVE SEROTONIN REUPTAKE INHIBITORS (SSRIs) - Mechanism of Action
|
• Produces selective inhibition of serotonin reuptake
• Produces CNS excitation |
|
|
|
SELECTIVE SEROTONIN REUPTAKE INHIBITORS (SSRIs) - Therapeutic Uses
|
• Primarily to treat major depression
• Obsessive-compulsive disorder • Bulimia nervosa • Premenstrual dysphoric disorder |
|
|
|
SELECTIVE SEROTONIN REUPTAKE INHIBITORS (SSRIs) - Pharmacokinetics
|
• Half-life of 2 days
• Widely distributed and highly bound to plasma proteins. • Overall better tolerated than TCA |
|
|
|
SELECTIVE SEROTONIN REUPTAKE INHIBITORS (SSRIs) - Adverse Effects
|
Most common are:
• Sexual Dysfunction • Weight Gain • Serotonin syndrome • Withdrawal syndrome • Neonatal withdrawal syndrome Less common are: • Extrapyramidal side effects • Bruxism: Grindin of teeth • Bleeding disorders |
|
|
|
SELECTIVE SEROTONIN REUPTAKE INHIBITORS (SSRIs) - Drug Interactions
|
• Monoamine oxidase inhibitors
• Warfarin • Tricyclic antidepressants and lithium |
|
|
|
SELECTIVE SEROTONIN REUPTAKE INHIBITORS (SSRIs) - Preparations, Dosage, and Administration
|
• Several oral formulations
• Sold under three trade names – Prozac – Prozac Weekly – Sarafem • Daily, weekly, and withdrawal dosing |
(Prozac)
|
|
|
Serotonin/Norepinephrine Reuptake inhibitors (S/NRIs)
|
• Venlafaxine
• Duloxetine |
|
|
|
Venlafaxine [Effexor]
|
• Major depression
• Generalized anxiety disorder (GAD) • Social anxiety disorder (social phobia) • Blocks NE and serotonin uptake • Does not block cholinergic, histaminergic or alpha1-adrenergic receptors. • Serious reactions if combined with MAOIs |
|
|
|
Venlafaxine [Effexor] - side effects
|
• Nausea
• Headache • Anorexia • Nervousness • Sweating • Somnolence • Insomnia • Weight loss/anorexia • Diastolic hypertension • Sexual dysfunction • Hyponatremia (in elderly) • Neonatal withdrawal syndrome |
|
|
|
Duloxetine [Cymbalta] - Mechanism of action and therapeutic use
|
– Inhibits serotonin and NE reuptake
– Weakly inhibits dopamine reuptake – Does not inhibit monoamine oxidase (MAO) – Relieves depression – Relieves pain of diabetic peripheral neuropathy |
|
|
|
Duloxetine [Cymbalta] - Pharmacokinetics
|
– Well absorbed following oral administration
– Food reduces rate of absorption – Highly bound to albumin in the blood – Half-life is 12 hours |
|
|
|
Duloxetine [Cymbalta] - Adverse effects
|
– Nausea
– Somnolence – Dry mouth – Sweating – Insomnia – Blurred vision • Effects in pregnancy and lactation |
|
|
|
Duloxetine [Cymbalta] - Drug interactions
|
– Alcohol
– MAO inhibitor – Drugs that inhibit CYP1A2 or CYP2D6 |
|
|
|
MONOAMINE OXIDASE INHIBITORS (MAOIs) - Mechanism of action
|
– Converts monoamine neurotransmitters—NE, serotonin, and dopamine—into inactive products.
– Inactivates tyramine and other biogenic amines – Two forms of MAO in the body – MAO-A and MAO-B – Affected by antidepressants – Acts on MAO in two ways: reversible and irreversible • Irreversible, lasts about 2 weeks • Reversible, lasts 3 to 5 days – All of the MAOIs in current use cause irreversible inhibition. |
|
|
|
MONOAMINE OXIDASE INHIBITORS (MAOIs) - Therapeutic uses
|
– Depression
– Other uses • Bulimia nervosa • Obsessive-compulsive disorders • Panic attacks |
|
|
|
MONOAMINE OXIDASE INHIBITORS (MAOIs) - Adverse effects
|
– CNS stimulation
– Orthostatic hypotension – Hypertensive crisis from dietary tyramine |
|
|
|
MONOAMINE OXIDASE INHIBITORS (MAOIs) - Drug interactions
|
– Indirect-acting sympathomimetic agents
– Interactions secondary to inhibition of hepatic MAO – Antidepressants: TCAs and SSRIs – Antihypertensive drugs – Meperidine |
|
|
|
MONOAMINE OXIDASE INHIBITORS (MAOIs) - Preparations, dosage, and administration
|
– All MAOIs are administered orally
|
|
|
|
ATYPICAL ANTIDEPRESSANTS - Bupropion [Wellbutrin]
• Actions and Uses |
– Acts as stimulant and suppresses appetite
– Antidepressant effects begins in 1 to 3 weeks – Does not affect serotonergic, cholinergic, or histaminergic transmission – Does not cause weight gain – Increases sexual desire and pleasure |
|
|
|
ATYPICAL ANTIDEPRESSANTS - Bupropion [Wellbutrin]
• Adverse Effects |
– Can cause seizures
– Agitation – Tremor – Tachycardia – Blurred vision – Dizziness – Headache – Insomnia – Dry mouth – GI upset – Constipation – Weight loss |
|
|
|
ATYPICAL ANTIDEPRESSANTS - Bupropion [Wellbutrin]
• Drug Interactions |
– MAOIs can increase the risk of bupropion toxicity
|
|
|
|
ATYPICAL ANTIDEPRESSANTS - Bupropion [Wellbutrin]
• Preparations, dosage, and administration |
– Immediate-release, sustained-release, or extended-release tablets
|
|
|
|
Other Atypical Antidepressants
|
• Nefazodone
• Mirtazapine [Remeron] • Amoxapine [Asendin] • Reboxetine [Vestra] • Trazodone [Desyrel |
not on study guide
|
|
|
Electroconvulsive Therapy
|
• Outside the realm of pharmacology
• Valuable treatment for depression • Two desirable characteristics – Effectiveness – Rapid onset (relative to antidepressant drugs) • Two primary types of patients – Those who have failed to respond to drugs – Severely depressed, suicidal patients • Can terminate depression episode • Adverse effect – Some loss of memory for events immediately surrounding treatment |
not on study guide
|
|
|
Vagus Nerve Stimulation
|
• For long-term therapy of treatment-resistant depression (TRD)
• Where at least four antidepressant drugs have failed • Mechanism of action – An implanted device – Delivers electrical pulses to the vagus nerve • Side effects – Hoarseness – Voice alteration – Cough – Dyspnea |
not on study guide
|
|
|
Parkinson’s disease (PD) is
|
a neurodegenerative disorder of the extrapyramidal system associated with disruption of neurotransmission within the striatum.
c. Proper function of the striatum requires a balance between the neurotransmitters dopamine and acetylcholine (ACh). d. Imbalance between dopamine and ACh results from degeneration of the neurons that supply dopamine to the striatum. |
|
|
|
Parkinson’s disease is characterized by
|
dyskinesias and akinesia.
|
dyskinesias:
1. A defect in the ability to perform voluntary movement. 2. Any disorder characterized by uncontrolled or involuntary movements. akinesia: Complete or partial loss of muscle movement; also spelled acinesia. |
|
|
Therapeutic goals of PD Drugs
|
o Improve patient’s ability to carry out activities of daily life
o Drug selection and dosages are determined by extent to which PD interferes with work, dressing, eating, bathing, etc. |
|
|
|
Normal
|

|
|
|
|
PD
|

|
|
|
|
Two major categories of PD drugs
|
o Dopaminergic agents
o Anticholinergic agents |
|
|
|
o Dopaminergic agents
|
By far the most commonly used for PD
Promote activation of dopamine receptors Levodopa [Dopar] |
|
|
|
o Anticholinergic agents
|
Prevent activation of cholinergic receptors
Benztropine [Cogentin] |
|
|
|
Dopamine agonists
|
o Pramipexole [Mirapex]
o Entacapone [Comtan] o Amantadine [Symmetrel] o Selegiline [Eldepryl, Carbex] |
|
|
|
Blood Brain Barrier
|
Nerve cells called astrocytes
Encircle the capillary walls of the brain Small molecules get through as well as lipid soluble drugs, glucose and gases. Permeation can occur with large doses of drugs that don’t usually cross or with meningeal irritation. Envision this as a large cap of astrocytes like a netting of protection. Alcohol can cross and it acts fast, Oxygen of course and glucose. Lipid soluble drugs Drugs that are protein bound or highly ionized can not cross Which protein are medications most likely to bind to once they are in the blood vessels? It isn't fully developed at birth, therefore newborn infants are much more sensitive to CNS drugs than are older children and adults |
|
|
|
Anticholinergic Effects
|
Salivary glands—decreased secretion
Sweat glands—decreased secretion Bronchial glands—decreased secretion Heart—increased rate Eye—mydriasis, blurred vision Urinary tract—interference with voiding Intestine—decreased tone and motility Lung—dilation of bronchi Stomach—decreased acid secretion Inform patients about possible anticholinergic reactions (dry mouth, blurred vision, photophobia, urinary hesitancy, constipation, tachycardia, suppression of sweating), and teach them how to minimize discomfort. Instruct patients to avoid all drugs with anticholinergic properties, including the antihistamines and certain over-the-counter sleep aids. |
|
|
|
Haloperidol Action
|
Alters the effects of dopamine in the CNS.
Also has anticholinergic and alpha-adrenergic blocking activity. |
|
|
|
Haloperidol Indication
|
Principal indications are schizophrenia and acute psychosis. In addition, haloperidol is a preferred agent for Tourette's syndrome. The drug is also effective in refractory migraine, although it is not approved for this use.
|
|
|
|
Haloperidol administration
|
PO or IM. Oral bioavailability is about 60%. Hepatic metabolism is extensive. Parent drug and metabolites are excreted in the urine.
|
|
|
|
Haloperidol [Haldol]
|
a member of the butyrophenone family, is the prototype of the highpotency FGAs.
|
|
|
|
Signs and Symptoms of Depression
|
• Depressed mood
• Loss of pleasure or interest • Insomnia (or sometimes hypersomnia) • Anorexia (or sometimes hyperphagia) • Mental slowing and loss of concentration • Feelings of guilt • Worthlessness • Helplessness • Thoughts of death and suicide • Overt suicidal behavior • Symptoms must be present most of the day, nearly every day, for a least 2 weeks |
|
|
|
What is pain?
|
Unpleasant sensory and emotional experience associated with actual or potential tissue damage
The most reliable method is to have the patient describe his or her experience |
|
|
|
Nociceptive pain
|
Results from injury to tissues
Two forms: somatic or visceral pain |
Not on study guide
|
|
|
Neuropathic pain
|
Results from injury to peripheral nerves
Responds poorly to opioids |
Not on study guide
|
|
|
Management Strategy (Pain)
|
ASK about pain regularly
Assess pain systematically BELIEVE the patient and family in their reports of pain and what relieves it CHOOSE pain control options appropriate for the patient, family, and setting DELIVER interventions in a timely, logical, coordinated fashion EMPOWER patients and their families Enable patients to control their treatment to the greatest extent possible |
A
B C D E |
|
|
Issues of Pain
|
Addiction or tolerance
Bias of health care professionals Fear of side effects of opioids Legal regulations Understanding of how pain control works Cultural differences around pain and treatment |
Not on study guide
|
|
|
Acute Pain
|
Sudden onset
Change in VS Anxiety & restlessness Descriptors: Sharp Body Language apparent Throbbing |
Not on study guide
|
|
|
Chronic Pain
|
Ongoing, lived with a long time.
Effect on ADL’s is usually the best indicator of degree of pain. May have very little body language. Descriptors: Constant companion Dull, deep |
Not on study guide
|
|
|
Pain Assessment
|
Use symptom descriptors: ache, burning, continuous etc
Locate the pain on the body Mark it in the chart on either a figure of the body or describe it in terms of anatomy. Evaluation is the Key It is necessary to evaluate the pain on 3 levels: Prior to medication or intervention During intervention After intervention |
|
|
|
Three classifications of Barbiturates
|
– Ultrashort acting (thiopental)
– Short to intermediate acting (secobarbital) – Long acting (phenobarbital) |
|
|
|
Barbiturates Mechanism of action
|
– Binds to the GABA receptor-chloride channel complex
– Action is limited only by the amount of barbiturate administered. |
|
|
|
Barbiturates Pharmacokinetics
|
– Lipid solubility has a significant impact
– Rapid onset and brief duration |
|
|
|
Barbiturates Therapeutic uses
|
– Seizure disorders
– Induction of anesthesia – Insomnia – Other uses |
|
|
|
Barbiturates Adverse effects
|
– Respiratory depression
– Suicide – Abuse – Use in pregnancy – Exacerbation of intermittent porphyria – Hangover – Paradoxical excitement – Hyperalgesia |
|
|
|
Barbiturates Acute Toxicity
|
– Symptoms
• Respiratory depression • Coma • Pinpoint pupils – Treatment • Removal of barbiturate from the body • Maintenance of an adequate oxygen supply to the brain |
|
|
|
Barbiturates Administration
|
– Oral
– Intravenous – Intramuscular |
|
|
|
MAOI diet (avoid)
|
Avoid foods that contain Tyramine:
Avocados, especially if overripe; fermented bean curd; fermented soybean; soybean paste Figs, especially if overripe; bananas, in large amounts Meats that are fermented, smoked, or otherwise aged; spoiled meats; liver, unless very fresh Fermented varieties: bologna, pepperoni, salami, others Dried or cured fish; fish that is fermented, smoked, or otherwise aged; spoiled fish Practically all cheeses Yeast extract (eg, Marmite, Bovril) Some imported beers, Chianti wine Protein dietary supplements; soups (may contain protein extract), shrimp paste; soy sauce Chocolate (large amounts) Fava beans Ginseng Caffeinated beverages (large amounts) |
|
|
|
Barbiturates and benzodiazepines
|
|
|
|
|
Barbiturates over time
|
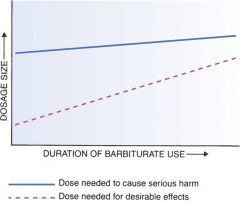
|
|

