![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
240 Cards in this Set
- Front
- Back
|
1 diuretics (Thiazide)
Hydrochlorothiazide Chlorthalidone Metolazone (popular used with loop agents) |
MOA: Inhibition of the Na/Cl transporter in the distal convoluted tubule
Effects: Modest increase in NaCl excretion some K wasting hypokalemic metabolic alkalosis decreased urine Ca Clinical App: Hypertension, mild heart failure, nephrolithiasis, nephrogenic diabetes insipidus Pharm/Kin/Tox: Oral duration 8–12 h Toxicity: Hypokalemic metabolic alkalosis, hyperuricemia, hyperglycemia, hyponatremia |
|
|
2 vasodilators:
Isosorbide |
MOA: Relax vascular smooth muscle
Venous>arterial>cardiac Venodilator reduces preload Reduces wall tension Reduces O2 demand Nitroglycerin – short acting (duration 20-30 minutes), multiple formulations, low bioavailability of oral preparations, usually sublingual tablets Isosorbide dinitrate – longer acting, oral preparation Isosorbide mononitrate- better bioavailability. Adverse Effects Too much vasodilation – orthostatic hypotension; headache; reflex tachycardia and increase in contractility Tolerance – continuous use not effective Can occur with in 24-48 hours. Use 12 H/day Drug interactions – sildenafil, etc. |
|
|
3 vasodilators:
minoxidil |
>orally active vasodilator. opens K+ channels in smooth muscle membranes by minoxidil sulfate
>Dilates arterioles but not veins >Minoxidil should replace hydralazine when maximal doses of the latter are not effective Effects: reflex sympathetic stimulation and Na+ and fluid retention. Must be used in combination with a beta blocker & loop diuretic. Tachycardia, palpitations, angina, and edema occur when doses of B blockers and diuretics are inadequate. HA, sweating, and hypertrichosis |
|
|
4 vasodilators:
hydralazine |
MOA: Dilates arterioles but not veins; >Combination of hydralazine with nitrates is effective in HF, and should be considered in patients with both HTN and HF, especially in A-A patients.
>Absorp: well absorbed and rapidly metabolized by the liver during the first pass, so that bioavailability is low (avg 25%) >Adverse Effects: headache, nausea, anorexia, palpitations, sweating, and flushing. |
|
|
5 alpha blockers:
Doxazosin |
Indication: used primarily in men with concurrent HTN and BPH
MOA: antihypertensive effects by selectively blocking 1 receptors in arterioles and venules .>Alpha blockers reduce arterial pressure by dilating both resistance and capacitance vessels. Toxicity: reported toxicities of the a 1 blockers are relatively infrequent and mild. dizziness, palpitations, headache, and lassitude |
|
|
6 diuretics (Loop diuretics)
Furosemide Torsemide |
MOA: Inhibition of the Na/K/2Cl transporter in the ascending limb of Henle's loop
Effects: Marked increase in NaCl excretion, some K wasting, hypokalemic metabolic alkalosis, increased urine Ca and Mg Clinical App: Pulmonary edema, peripheral edema, hypertension, acute hypercalcemia or hyperkalemia, acute renal failure, anion overdose Pharm/Tox/Intrx: Oral and parenteral preparations duration of action 2–4 h Toxicitiy: Ototoxicity, hypovolemia, K wasting, hyperuricemia, hypomagnesem |
|
|
diuretics (Potassium Sparing)
Spironolactone Epelrenone (selective aldosterone blocker) |
MOA: Pharmacologic antagonist of aldosterone weak antagonism of androgen receptors
Effects: Reduces Na retention and K wasting in kidney poorly understood antagonism of aldosterone in heart and vessels Clinical App: Aldosteronism from any cause hypokalemia due to other diuretics postmyocardial infarction Tox/Pharm/Intrx: Slow onset and offset of effect duration 24–48 h Toxicity: Hyperkalemia, gynecomastia (spironolactone, not eplerenone) additive interaction with other K-retaining drugs |
|
|
Centrally acting alpha agonists:
Clonidine Methyldopa Guanfacine |
MOA: reduce sympathetic outflow from vasomotor centers in the brain stem but allow these centers to retain or even increase their sensitivity to baroreceptor control
(decreasd sympathetic outflow to heart, kidneys, peripheral vascularture by stimulating alpha adrenergic receptors) |
|
|
Clonidine
|
Effect: reduction of cardiac output due to decreased heart rate and relaxation of capacitance vessels, with a reduction in peripheral vascular resistance reduces blood pressure (in the supine position)
AE: bradycardia, drowsiness, HA, CNS depression, xerostomia, constpation, weakness,transdermal rxns Misc: abrupt d/c may cause rebound HTN, fewer with TD patch |
|
|
Methyldopa
|
Clinical: (HTN in pregnancy)
Effect: reducing peripheral vascular resistance, with a variable reduction in heart rate and cardiac output. (supine) AEs: edema,dry mouth, drowsiness, mental depression, incr LFTs CIs: active hepatic dz, current MAOI use Misc: tx in pregnancy. DO NOT stop abruptly. |
|
|
Guanfacine
|
Guanabenz and guanfacine are centrally active antihypertensive drugs that share the central a-adrenoceptor-stimulating effects of clonidine. They do not appear to offer any advantages over clonidine and are rarely used.
AEs: somnolence, dizziness, HA, fatigue, constip, N&V, wt gain Metab: CYP3A4 |
|
|
Other antiarryhthmic agents:
Digoxin |
MOA: Na+,K+ ATPase inhibition results in reduced Ca2+ expulsion and increased Ca2+ stored in sarcoplasmic reticulum
Effect: Increases cardiac contractility cardiac parasympathomimetic effect (slowed sinus heart rate, slowed atrioventricular conduction) Clinical: Chronic symptomatic heart failure rapid ventricular rate in atrial fibrillation Pharm: Oral, parenteral duration 36–40 h Toxicity: Nausea, vomiting, diarrhea cardiac arrhythmias |
|
|
Ca2+ Channel Blockers
Non-dihydropyridine: verapamil, diltiazem |
Mechanisms – block voltage-gated calcium channels in vascular smooth muscle; decreases calcium entry; modest slowing of calcium channel reactivation in the heart
Pharmacological Effect – arterial vasodilation (less potent than nifedipine); decrease in BP; cardiac actions block reflex sympathetic activation of heart; modest decrease in HR with diltiazem Adverse Effects – excessive vasodilation (hypotension, etc.); bradycardia, transient asystole in patients with A-V conduction problems Therapeutic Uses – hypertension (a mainstay); angina; tachycardias |
|
|
Ca2+ Channel Blockers
Dihydropyridines: **amlodipine,** |
Mechanism – blocks voltage-gated calcium channels in vascular smooth muscle; decreases calcium entry
Pharmacological Effect – arterial vasodilation; decrease in BP; mild reflex sympathetic activation Therapeutic Uses – hypertension (a mainstay); angina Adverse Effects – excessive vasodilation (hypotension, etc.); edema, constipation |
|
|
asthma: incidence
|
-5% of US population
-2 million ER visits -500,000 hospitalizations -5000 deaths annually 50% of kids will outgrow sx |
|
|
asthma:
actue attack |
-caused by trigger/allergen
-characterized by: --bronchospasm --air trapping --mucus plugging |
|
|
asthma:
chronic pathophysiology |
-hyper responsive airways
-airway obstruction (in peripheral airspaces, air trapping leading to hypoxia) -airway remodeling (from persistent inflammation, hyperplasia of smooth muscle tissue) |
|
|
classification of asthma:
mild intermittant |
-pt is doing fine, not much limitation, might need inhaler for sports or something
Day Sx: <2 x per week night sx: <2x per month FEV1: > or = 80% |
|
|
classification of asthma:
mild persistent |
-some sx during daily activities
day sx: >2x/week night sx: >3-4/month FEV1: >/= 80% |
|
|
classification of asthma:
moderate persistent |
sx: every day
night sx: >5x/month FEV1: >60-<80% |
|
|
classification of asthma:
severe persistent |
continual symptoms
night symptoms are frequent FEV1: </= 60% |
|
|
Steps 1-6 for med treatment of asthma
|
Step 1: SABA (first line!!)
Step 2: Inhaled corticosteroid (best) or---LTRA,cromolyn, nedcromyl, theophyline Step 3: Low dose ICS+SABA --or-- medium dose ICS (alternatives: low dose ICS + either LTRA, theophyline or zileuton) Step 4: med dose ICS +SABA Alt- med dose ICS + either LTRA, theophylline, zileutron Step 5: hi-dose ICS + LABA *and* omalizumab (pts who have allergies) Step 6: hi-dose ICS + LABA + oral corticosteroid AND - omalizumab (allergies) Step 4: |
|
|
sympathomimetics: (bronchodilators)
Alpha-Adrenergic Stimulation |
-vascoconstriction
-nasal decongestion -pressor effects |
|
|
sympathomimetics:
(bronchodilators) B1-adrenergic stimulation |
-increases myocardial contractility and conduction
|
|
|
sympathomimetics:
(bronchodilators) B2 adrenergic stimulation |
-bronchial dilation
-vasodilation -enhanced mucociliary clearance -INHIBITION of cholinergic neurotransmission |
|
|
mechanism of action for bronchodilators (sympathomimetics)
|
1-stimulate beta receptors which then activate adenyl cyclase (AC)
2- increases the intracellular production of cAMP 3- bronchodilation, decreased inflammatory cell mediator release and increased mucociliary clearance ensues |
|
|
indications for:
Short Acting Beta Agonists Albuterol Levoalbuterol (Xoponex) |
-the FIRST LINE of tx for asthma
-tx for acute exacerbations -"rescue therapy" -prophylaxis for exercise induced asthma -duration: 3 hours Side Effects: (2ndary to beta1 action on heart) -common: palpitations, HTN, HA, tachycardia, paroxysmal bronchoconstriction -usually transient, pt edu! |
|
|
indications for Long Acting Beta 2 Agonists:
Salmeterol (serevent) |
Indications: MAINTENANCE TX in moderate to severe persistent
-incr with nocturnal sx -COPD w/ asthma component -->should NOT be used as only tx... NOT FOR RESCUE Side Effects: (2ndary to beta1 action on heart) -common: palpitations, HTN, HA, tachycardia, paroxysmal bronchoconstriction -usually transient, pt edu! |
|
|
monitoring for long/short acting beta agonists:
|
they can cause:
-hypokalemia: pts on diuretics take heed -blood pressure incr in pts taking MAOIs & TCAs -contraindication: hx of allergy to med |
|
|
sympathomimetic:
Epinephrine -basics & --indications |
-is naturally occuring catecholamine
-MAO: acts on alpha & beta receptors-->quick bronchodilation, incr gas exchange (1 min) -Route: IV-rapid onset, short duration, can repeat in 3-4 hours -Low doses: beta receptor action most potent High-doses: results in alpha rxn Indication: reserved for ACUTE asthma attack unrelieved with anything else & anaphylaxis |
|
|
sympathomimetic:
Epinephrine side effects, contraindications |
Side effects: similar to other sympathomimetics
-cerebral hemorrhage(a-1), cardiac arrhythmias/V-fib (b1), pulmonary edema, worsening cardiac sx in hypothyroid & cocaine use >>NO contraindications!! |
|
|
corticosteroids:
Fluticasone (Flovent) Prednisone MOA: |
-bind to glucocorticoid receptors,
-inhibit transcription to decrease release of inflammatory products -induces transcription of anti-inflammatory products -over long period: reduces airway hyperactivity |
|
|
corticosteroids:
Indications: Fluticasone (Flovent) Prednisone |
Long term control:
-FIRST LINE tx for persistent asthma (inhaled) -Systemic: acute exacerbation & severe persistent -IV - acute severe exacerbation (status asthmaticus) unable to take oral med during this |
|
|
corticosteroids:
Fluticasone (Flovent) Prednisone --Adverse Reactions |
>10% : insomnia, nervousness, increased appetite, indigestion
--1-10%: hyperglycemia, hirsutism, claucoma, epistaxis --<1%: edema, HTN, vertigo, Cushings, HPA (hypothalamic pituitary axis suppression), muscle wasting, osteoporosis, hypokalemia, |
|
|
corticosteroids:
Fluticasone (Flovent) Prednisone --Contraindications/monitoring |
Contraindications: hypersensitivity
-disseminated fungal infection Monitoring: blood pressure if taking with MAOIs/TCAs -systemic infections |
|
|
mast cell stabilizer:
Cromolyn MOA |
MOA: stabilize mast cells
-inhibit mast cell degeneration -decrease initiation of asthmatic response & inflammatory mediators |
|
|
mast cell stabilizer:
Cromolyn indications & Adverse Effects |
Indications: -alt tx to steroids
-safe, can be often use in children -exercise induced asthma, take 1 hour prior -allergic rhinitis component Adverse Effects: minimal: -dry throat/mouth, bad taste -well tolerated, no drug interactions |
|
|
Theophylline
MOA: |
MOA: induced phosphodiesterase inhibition
-results in INCR cAMP (to lesser extent than B-agonists) -non-bronchiodilator effects: --reduce mucus secretion, incr mucociliary transport, diaphragm contractility (NOT 1st line) |
|
|
Theophylline
Indications/Route: |
-3rd line in acute exacerbations to SABA and ICAs
-alt to LABA in persistent asthma -most beneficial as addition to ICS in pts with nocturnal sx ROUTE: oral: once daily IV: uncommon, only in hospital (infusion w/ loading dose) |
|
|
Theophylline
Side effects/ Contraindications/ Monitoring |
SE: n/v, diarrhea, anorexia, palpitations, incr GERD sx, reduced LES tone
Contraindications: -hypersensitivity to xanthine prod -caution in seziure/peptic ulcer dz Monitoring: REQUIRES TX DRUG MONITORING -concentration goal 5-15 ug/mL -caution with liver dz, HTN, CHF, EtOH, trough monitoring |
|
|
Theophylline
Interactions Stuff that Decreases it |
-age (1-9 yrs)
-fever, food, -high protein diet -smoking Drugs: carbamazepine, phenobarbital, phenytoin, rifampin |
|
|
Theophylline
Interactions Stuff that Increases it |
-age (elderly)
-cor pulmonale -CHF decompensated -fever -fatty foods, cirrhosis Drugs: allopurinol, BB, CCB, cimetidine, Cipro, flu vaccine, macrolides, oral contraceptives, zafirlukast |
|
|
what are the 2 kinds of leukotriene modifiers and what are they preventing from happen?
|
>5-lipoxygenase inhibitors &
>leukotriene receptor agonists --leukotrienes are the result of 5-lipoxygenase on arachadonic acid --synthesized by cells assoc w/ incr inflammation: eosin,baso,neutro & monocytes --results in: constriction of smooth muscle, promotes mucus secretion |
|
|
Leukotriene Inhibitors:
Monteleukast (Singulair) MOA |
MOA: bind to cysteinyl leukotriene receptors to inhibit actions of LTD4
-those receptors are found in: airway smooth muscles cells & macrophages -pro inflammatory cells (incl eosinophils) --anti-inflammatory, bronchodilator effects |
|
|
Leukotriene Inhibitors:
Monteleukast (Singulair) Indications |
-2nd LINE TX TO ICS
--important for MAINTENANCE tx --use for: chronic tx of asthma >12mo --seasonal allergic rhinitis >2 yrs --perennial allergic rhinitis >6mo --prevention of EIasthma >15 yrs --Give 2 hours BEFORE exercise (not w/in 24 hrs of previous dose) |
|
|
Leukotriene Inhibitors:
Monteleukast (Singulair) Adverse Effects & Monitoring |
AdvrseEvnts: uncommon
--HA, dyspepsia,dizziness -Churg-Strauss Syndrome (eosinophilic vasculitis, rare, usually occurs in pts w/ decr or taper of chronic steroids, monitor for vasculitis/rash, pulmonary/cardiac neuropathic sx -Monitor: pts taking hepatic enzyme inducers (rifampin, seizure drug) FDA2009: monitor for mood change |
|
|
Anti-cholinergics:
Mechanism of Action |
-block Ach from binding to post-ganglionic muscarinic receptors in airway
--result = bronchodilation --reduces intrinsic vagal tone in airways --reduces mucus gland secretion |
|
|
Anti-Cholinergics:
Ipatropium (Atrovent) Indications: |
--recommended for use in combination with beta agonists for acute exacerbation
--DO NOT use alone in exacerbation -->FIRST LINE IN COPD -alternative use: when pt presents with bronchospasm caused by BBlocker |
|
|
Anti-Cholinergics:
Ipatropium (Atrovent) Adverse Effects |
-URI, bronchitis, sinusitis, chest pain, palpiations, headache, dizziness, dyspepsia, nausea, dry mouth, UTI, back pain, flu like syndrome
--all rare things |
|
|
COPD:
Definition & Classification |
--abnormal tests of expiratory flow that do not change over periods of several months
--not fully reversible Classified: 2 things: --Emphysema -abnormal dilation of terminal air spaces, w/out evidence of interstitial lung dz --Chronic Bronchitis- chronic cough & sputum production |
|
|
COPD
Incidence |
-17 million Americans
-4th leading cause of death in US -leading cause of hospitalization in the elderly -most common in older men -women progress more rapidly |
|
|
COPD
Symptoms & Risk Factors: |
Sx:
-dyspnea on exertion, worsening -sputum production -chronic cough Risk Factors: -smoking -occupational -genetic |
|
|
COPD Staging:
|
(just like NYHA for CHF)
I-mild: chronic cough, sputum, asx FEV1 >80% II-moderate: DOE, cough, sputum, FEV1 >50% but <80% III-severe: SOB, fatigue, exacerbations, decr exercise FEV1 >30% but <50% IV-very severe: respiratory failure, decr quality of life FEV1 <30% or <50% w evidence of respiratory failure FOR ALL: FEV1/FVC <0.70 |
|
|
COPD treatment goals
|
-prevent progression
-relieve symptoms -minimize exercise intolerance -prevent exacerbations -treat exacerbations in timely manner -reduce hospitalization -reduce mortality |
|
|
COPD
Oxygen Therapy |
-indications: chronic hypoxemia
(Arterial O2 <55mmHg or Sat <88% -OR- -arterial O2 55-60mmHg or sat <89% with evidence of cor pulmonale, pumonary HTN, or polycythemia Administration: -Nasal canula -at least 18hrs q day for benefit -lowest dose necessary to keep sats at or above 90% |
|
|
medication therapy at each stage of COPD
|
>I-mild-add SAbronchodilator
active reduction of risk factors (flu vaccine) >II-moderate: both above and add regular tx with long acting bronchodilators, add rehab >III-severe: all of above add ICS if repeated exacerbations >IV-very severe: all of above + long term O2, consider surgery |
|
|
pulmonary hypertension:
definition |
pulmonary arterial pressure greater than 25 mm Hg
-diagnosed by right heart catheterization --overall poor prognosis |
|
|
pulmonary hypertension:
classification system by the WHO |
-Group 1: sporadic, hereditary, connective tissue disease, drug induced, portal HTn
-Group 2: left sided HF -Group 3: lung disease & hypoxemia (ex: COPD, interstitial lung dz) -Group 4: Chronic thromboembolic -Group 5: unclear cause |
|
|
Treatments for Pulmonary Hypertension (drugs)
|
-CCB
-Revatio (sildenifil) -Tracleer (bostenan) -flolan -iloprost |
|
|
Pulm HTN:
Sildenafil (Revatio) MOA |
-phosphodiesterase 5 inhibitor
-increases cGMP levels -allows vasodilation in smooth muscle, including pulmonary vessels -4 hour half life |
|
|
Pulm HTN:
Sildenafil (Revatio) Indication/ Dosage |
--pulmonary HTN, group 1 WHO
-Contraindications: -being on Nitrates already -hypersensitivity -use of protease inhibitors (HIV) Dosage: IV:bolus 10 mg TID oral: 20mg TID note: different dosing from viagra (dosed at 25,50, 100 mg) |
|
|
pulm HTN:
Sildenafil (revatio) Side effects: |
flushing
dizziness epistaxis more severe: hearing loss, priapism, MI |
|
|
pulm HTN:
Bosetan (Tracleer) MOA |
-dual endothelial receptor antagonist (endothelin 1 causes vasoconstriction/tissue remodeling/fibrosis)
--higher levels found in pts w/ pulmonary HTN --Medication: specific antagonist -vasodilation, incr CO, 5 hr half life |
|
|
pulm HTN:
Bosetan (Tracleer) Indications: |
-pulmonary HTN group 1
-increase exercise tolerance Contraindications: --use with glyburide/cyclosprine A PREGNANCY CATEGORY X (2 forms of birth control mandatory) |
|
|
pulm HTN:
Bosetan (Tracleer) Side Effects & Monitoring |
SE: hypotension, flushing, HA, Decr. Hgb, **Severe**: Liver failure, angioedema
Monitoring: pregnancy, monthly Liver enzymes, CBC 1st & 3rd mo, then q 3 mo. CHF monitoring |
|
|
pulm HTN:
Iloprost MOA: |
MOA: synthetic analog of prostacylcin PG2
-dilates systemic & pulmonary arterioles -**some action on platelet aggregation** -half life- 20-30 min -adm by inhalation 6-9 x q day (incr cAMP - relaxation) |
|
|
pulm HTN:
Iloprost Indications: |
pulmonary HTN
-contraindications: -none established currently -precaution in asthma/COPD (evidence of bronchospasm) |
|
|
pulm HTN:
Iloprost Side effects |
-flushing
-HA -cough -hypotension -severe: pulmonary edema |
|
|
Nicotine Replacement:
Nicotine: MOA |
-agonist to nicotinic receptors at autonomic ganglia, adrenal medulla, neuromuscular junctions & the brain
-release of pleasure neurotransmitters -routes: inhalation, systemic, nasal |
|
|
Nicotine replacement:
Nicorette Indication/adverse effects administration |
Indc: smoking cessation adjunct tx
-contraindicated: hypersensivty -Adverse Effcts: dermal reaction (if patch) -HTN, tachycardia -palpitations Instructions: bite down once, place gum at buccal mucosa, another bite & leave at buccal mucosa (NOT for chewing constantly) |
|
|
Verenicline (Chantix)
MOA |
-binds with hi affinity to alpha-4-beta nicotinic acetylcholine receptors in brain
-reduces craving -agonist at receptors inducing nicotinic effects -keep pt on for several months |
|
|
Verenicline (Chantix)
Indication/contraind, precautions/FDA |
-indicated: smoking cessation
-contra: hypersensitivity -warnings: mood disorders, CVD FDA: higher incidence of CV events Black Box: incr neuropsychotic events, suicide, psychosis, monitor behavioral change |
|
|
Verenicline (Chantix)
Adverse Effects |
-vivid dreams
-constipation -nausea -vomiting -HA |
|
|
hypertension:
Etiology |
Primary HTN: no identifiable cause no cure
Secondary: CKD, coarctation of aorta, Cushing's, drug induced, pheochromocytoma, primary aldosteronism, renovascular HTN, sleep apnea, thyroid/parathyroid disease, obstructive uropathy |
|
|
what are some drugs that elevate blood pressure?
|
prednisone
decongestants NSAIDS (illicit amphetamines of course) |
|
|
complications of HTN
(uncontrolled) |
-LV hypertrophy
-angina/MI -coronary revascularization -heart failure -peripheral artery disease -retinopathy -stroke/TIA -dementia |
|
|
blood pressure classifications by the JNC 7
|
normal - <120 / <80
preHTN - 120-139 / 80-89 Stage 1 HTN - 140-159 / 90-99 Stage 2 HTN - >=160/ >=100 |
|
|
Approach to treatment of HTN
|
1-start with lifestyle modifications
2- initial drug choices: with or without "compelling indications" WITHOUT: Stage 1: mono tx, thiazide diruetics Stage 2: 2 drugs - diuretic + ACEI, ARB, BB, CCB WITH: ACEI, ARB, BB, CCB treat indication |
|
|
ALLHAT trial: some conclusions from it?
|
>alpha blockers were stopped early due to higher CV events (NOT recommended for 1st line tx
>CCB v Diuretics: no difference in CHD/mortality/stroke but 38% higher risk from HF >ACEI v diuretics: no difference in CHD/ total moratlity. higher risk of stroke in AAs. 10% higher risk of combined CVD outcome DIURETIC TX is 1st LINE TX to nearly all HTN pts w/out comorbid conditions |
|
|
Diuretics:
MOA in General |
-inhibit reabsorption of sodium & water from renal tubules
-initial BP reduction results from decr blood volume/CO; incr PVR -after 6-8 wks CO returns to normal & PVR declines (they work better after you've been on them for 2 months) |
|
|
Types of Diuretics & Sites of Action:
Loop Thiazide K+ Sparing |
Loop: ascending loop of Henle
Thiazide: proximal distal tubule K+ Sparing: distal tubule |
|
|
Thiazide Diuretics:
>Hydrocholorothiazide >Metolazone >Chlorthalidone MOA Pharmacokinetics |
MOA: inhibit NaCl resorption by blocking Na+/Cl- transporter in distal collecting tubule
Pharmacokinetics: onset w/in 1-2 hours, metabolism: most agents not metabolised, primary renal excretion |
|
|
thiazide diuretics:
hydrochlorothiazide chlorothalidone metolazone SIDE EFFECTS |
>Electrolyte imbalances
--hypokalemia, hyponatremia, hyeruricemia, hypercalcemia, hypomagnesemia >increase in serum cholesterol!! >glucose intolerance >metabolic alkalosis |
|
|
thiazide diuretics:
hydrochlorothiazide chlorothalidone metolazone CLINICAL PEARLS |
-FIRST LINE for majority of pts with HTN
-better BP lowering effect than loop diuretics, but less effective diuretic effect -less effective when CrClrnce <30 mL/min (renal dysfunction) -response seen within 4-6 weeks |
|
|
Loop Diuretics:
(Furosemide, Torsemide) MOA |
> inhibts active Cl- transport in thick ascending limb of Loop of Henle
>MOST POTENT diuretic, but not most effective BP lowering agent |
|
|
Loop Diuretics:
(Furosemide, Torsemide) conversions between those 2 and buetanide |
Bumetanide 1 mg =
Furosemide 40 mg = torsemide 10 mg |
|
|
Loop Diuretics:
(Furosemide, Torsemide) Side effects |
>Fluid & electrolyte loss (decr in K+, Na+, Mg+, Ca+)
>Hyperglycemia >nephropathy >hyperuricemia >photosensitivity |
|
|
Loop Diuretics:
(Furosemide, Torsemide) Side Effects |
>Digoxin (diuretic induced hypokalemia, incr digoxin toxicity)
>Lithium: (decr. lithium excretion, monitor serum levels) >Aminoglycosides (incr risk for ototoxicity & nephrotoxicity) |
|
|
Potassium Sparing Diuretics:
Spironolactone/Epelrenone MOA |
>are ALDOSTERONE receptor blockers: have weak diuretic effect, are often combined with other agents
>inhibit Na reabsorption in the distal tubule, cortical collecting tubule, and collecting duct ... subsequently reducing K+ and H+ secretion >incr Na+ loss, incr K+ retention, decr Ca+ excretion, decr Mg+ loss |
|
|
Potassium Sparing Diuretics:
Spironolactone/Epelrenone Pharmacokinetics/ metabolism/ elmination |
Pharm: absorption: food increases bioavailability of spironolactone
Metab: epelrenone: extensive hepatic metabolism by CYP3A4 Elimination: primary renal |
|
|
Potassium Sparing Diuretics:
Spironolactone/Epelrenone Side Effects/Contraindctns |
SE: HYPERkalemia.
-spironolactone: impotence, bitch tits, benign prostatic hyperplasia >relative contraindication: -renal insufficiency >USE CAUTIOUSLY in combination with ACEI & ARBs since it may incr risk for hyperkalemia |
|
|
Diuretics: Monitoring parameters
|
>BUN, Serum Cr,
>Electrolytes, Weight >signs of fluid retention >signs/symx of dehydration >hearing loss (loops) >uric acid (thiazides) |
|
|
ACE inhibitors:
(Lisinopril, Captopril, Ramipril) MOA |
MOA: >competitive inhibitor of angiotensin converting enzyme which prevents conversion of angiotensin I to angiotensin II (a potent vasoconstrictor)
>indirectly inhibits fluid volume increases by inhibiting angiotensin II stimulated release of aldosterone As a result: incr bradykinin/decr II --> vasodilation ->decr angiotensin II = decr sympathetic stimulation -->decr aldosterone secretion = incr Na+/water loss |
|
|
ACE inhibitors:
(Lisinopril, Captopril, Ramipril) Clinical Uses/ Contraindications |
-HTN
-CHF -Post MI -Renoprotection in DM Contraind: 2nd/3rd trimesters of pregnancy, angioedema w/ ACEI |
|
|
ACE inhibitors:
(Lisinopril, Captopril, Ramipril) Pharmacology |
-onset 1-2 hours
-Duration: typically 24 hrs, dose related for captopril -Absorption: food decr the absorption of captopril, ramipril -decr bioavailability of lisinopril in class II-IV HF -~25-75% absorption |
|
|
why are ACEI's given to diabetics?
|
-decreases efferent arteriolar resistance, increases renal blood flow
>> has renoprotective effects for this reason |
|
|
ACE inhibitors:
(Lisinopril, Captopril, Ramipril) Metabolism/Elimination |
metab: activated by hydrolysis in liver (except captopril/lisinopril)
elimination: primarly renal, -reduce dose for pts with renal insuff |
|
|
ACE inhibitors:
(Lisinopril, Captopril, Ramipril) Adverse Effects |
-cough*
-rash* -hyperkalemia -hypotension -angioedema* (more in AAs) -taste disturbances -neutropenia/agranulocytosis -acute renal failure *>result of buildup of bradykinin |
|
|
ACE inhibitors:
(Lisinopril, Captopril, Ramipril) Drug Interactions/ Monitoring parameters |
>NSAIDS/ASA (reduce efficacy of ACEI)
>K+sparing diuretics/K+supplements, trimethorphin (high dose) --> may exacerbate elevated K+ >Lithium - rise in Li+ levels Monitor: BUN, SCr, WBC, K+ |
|
|
ACE inhibitors:
(Lisinopril, Captopril, Ramipril) Clinical Pearls |
>no one ACEI is better than the other
>base selection on cost & dosing frequency >lower response rates for monotx in those w/ low renin & salt sensitive (AA, DM, elderly) >full effect after several weeks >dose not ensure complete blockage of ATII, gets produced by other pathways |
|
|
Diuretics: Monitoring parameters
|
>BUN, Serum Cr,
>Electrolytes, Weight >signs of fluid retention >signs/symx of dehydration >hearing loss (loops) >uric acid (thiazides) |
|
|
ACE inhibitors:
(Lisinopril, Captopril, Ramipril) MOA |
MOA: >competitive inhibitor of angiotensin converting enzyme which prevents conversion of angiotensin I to angiotensin II (a potent vasoconstrictor)
>indirectly inhibits fluid volume increases by inhibiting angiotensin II stimulated release of aldosterone As a result: incr bradykinin/decr II --> vasodilation ->decr angiotensin II = decr sympathetic stimulation -->decr aldosterone secretion = incr Na+/water loss |
|
|
ACE inhibitors:
(Lisinopril, Captopril, Ramipril) Clinical Uses/ Contraindications |
-HTN
-CHF -Post MI -Renoprotection in DM Contraind: 2nd/3rd trimesters of pregnancy, angioedema w/ ACEI |
|
|
ACE inhibitors:
(Lisinopril, Captopril, Ramipril) Pharmacology |
-onset 1-2 hours
-Duration: typically 24 hrs, dose related for captopril -Absorption: food decr the absorption of captopril, ramipril -decr bioavailability of lisinopril in class II-IV HF -~25-75% absorption |
|
|
why are ACEI's given to diabetics?
|
-decreases efferent arteriolar resistance, increases renal blood flow
>> has renoprotective effects for this reason |
|
|
ACE inhibitors:
(Lisinopril, Captopril, Ramipril) Metabolism/Elimination |
metab: activated by hydrolysis in liver (except captopril/lisinopril)
elimination: primarly renal, -reduce dose for pts with renal insuff |
|
|
ACE inhibitors:
(Lisinopril, Captopril, Ramipril) Adverse Effects |
-cough*
-rash* -hyperkalemia -hypotension -angioedema* (more in AAs) -taste disturbances -neutropenia/agranulocytosis -acute renal failure *>result of buildup of bradykinin |
|
|
ACE inhibitors:
(Lisinopril, Captopril, Ramipril) Drug Interactions/ Monitoring parameters |
>NSAIDS/ASA (reduce efficacy of ACEI)
>K+sparing diuretics/K+supplements, trimethorphin (high dose) --> may exacerbate elevated K+ >Lithium - rise in Li+ levels Monitor: BUN, SCr, WBC, K+ |
|
|
ACE inhibitors:
(Lisinopril, Captopril, Ramipril) Clinical Pearls |
>no one ACEI is better than the other
>base selection on cost & dosing frequency >lower response rates for monotx in those w/ low renin & salt sensitive (AA, DM, elderly) >full effect after several weeks >dose not ensure complete blockage of ATII, gets produced by other pathways |
|
|
ARBs (angiotensin II receptor blockers)
Losartan MOA |
->selectively binds to the AT1 receptor to block the actions of angiotensin II (ie: vasoconstriction & aldosterone secretion)
>(stimulation of A2 receptor to mediate vasodilation/activates NO2) >increases excretion of: -Cl+, Mg+, Ca+, PO4-, uric acid |
|
|
ARBs (angiotensin II receptor blockers)
Losartan Indications |
>ALL ARBs: HTN
-Losartan: HTN w/ LVH & DM nephropathy |
|
|
ARBs (angiotensin II receptor blockers)
Losartan Bioavailability, onset, metab |
-~15-33%, food decreases bioavail of losaratan
-onset 1-2 hours regularly; losartan 6 hours Metab: losartan extensive first pass metabolism, others via GI & gut |
|
|
ARBs (angiotensin II receptor blockers)
Losartan Side Effects |
-hypotension
-worsening of renal failure -hyperkalemia -angioedema (rare, also if they had it with ACEI they'll have it with ARBs too) -cough (less common than with ACEI) -Category X!!! -avoid use pts w/ bilateral renal artery stenosis |
|
|
ARBs (angiotensin II receptor blockers)
Losartan Monitoring |
-BUN, SCr, electrolytes, K+, CBC, HR, Hypotension
|
|
|
ARBs (angiotensin II receptor blockers)
Losartan Clinical Pearls |
Population response:
-similar efficacy regardless of age/sex -AA are less responsive to ARBs -use lower initial doses in pts with depletion of intravascular volume (elderly, @ risk for dehydration) |
|
|
Beta Blockers: MOA
|
-suppress the influence of sympathetic stimulations on heart, blood vessels, and other structures
|
|
|
Beta Blockers:
Labetelol, Carvedilol, Metoprolol -actions of non-selective (labetolol & carvedilol) and selective beta blockers (metoprolol) |
Carvedilol - alpha-blocking activity
Labetalol - ISA (intrinsic sympathomimetic activity), long acting, also used for glaucoma Metoprolol - MSA (membrane stabilizing activity |
|
|
Beta Blockers:
Labetelol, Carvedilol, Metoprolol Adverse Effects |
-Cardiovascular: -bradycardia, reduced exercise capacity, HF, hypotension, AV node conduction block (with underlying cardiac dz)
Other: -bronchoconstriction, hypoglycemia NOTE: be cautious about starting in pts with stage 3/4 HF/decompensated HF |
|
|
Beta Blockers:
that reduce M&M in pts w/ CHF |
-carvedilol
-bispropolol -metoprolol |
|
|
Calcium Channel Blockers:
DHP: Amlodipine NDHP: Verapamil, Diltiazem MOA: |
L-type Ca+ channel blockade decr transmembrane Ca+ current resulting in smooth muscle relaxation, decreased contractility, myocardial O2 demand, PVR & HR
NOTE: not good monotx; usually added to another drug, but are good hypertensive agents |
|
|
Calcium Channel Blockers:
DHP: Amlodipine vs. NDHP: Verapamil, Diltiazem |
DHP: have greater ratio of vascular smooth muscle effects (vasodilating) to cardiac effects
NDHP: affect atrioventricular nodal conduction to greater extent |
|
|
Calcium Channel Blockers:
DHP: Amlodipine NDHP: Verapamil, Diltiazem Adverse Effects |
Edema
flushing, headache constipation (verapamil) AV block, bradycardia, palpitations dizziness |
|
|
Calcium Channel Blockers:
DHP: Amlodipine NDHP: Verapamil, Diltiazem Drug Interactions |
-beta-blockers (slght incr adv efcts)
-statins -azoles (incr effects of) -phenytoin (incr conc of) -carbamazepine -cardiac glycosides (incr efct of) -amiodarone (incr efct of) |
|
|
Calcium Channel Blockers:
DHP: Amlodipine NDHP: Verapamil, Diltiazem CLINICAL PEARLS |
->Short acting dihydropyridines not recommended for HTN tx
->avoid non-dihydropyridines in left ventricular dysfunction or pulmonary congestion (HF) ->recent FDA medwatch conc: concurrent use of Simvastatin and CCBs -->do not exceed 10 mg simvastatin daily w/ verapamil/diltiazem -do not exceed 20 mg simvastatin daily with amlodipine |
|
|
Special Populations:
Elderly |
-HTN is in 3/4 of pts >80 y/o
-treat to recommended BP -caution: hypotension w/ rapid BP lowering -avoid centrally acting agents & alpha blockers -monitor for constipation w/ CCB |
|
|
Special Populations:
African Americans |
-disproportionately affected with HTN
-thiazides are first line tx -combination tx frequently required -higher incidence of angioedema with ACEIs |
|
|
What is Resistant HTN?
|
-failure to achieve goal BP in adherent pts on max doses of appropriate 3 drug regimen
-prevalance - 9-30% of treated -2ndary factors more likely to be present in pts with RHTN |
|
|
Potential causes of resistent HTN?
|
-volume overload: -excessive Na+ intake, inadequate diuretic tx
-exogenous substances: - steroids, NSAIDs, antidepressants, estrogens, cyclosporine, erythropoeitin, pseudoepedrine, street drugs, caffeine, alcohol -obesity -2ndary causes: - OSA, thyroid dysfx, CKD, renal artery stenosis, pheochromocytoma, primary aldosteronism |
|
|
Treatment for Resistent HTN
|
-exclude pseudo-resistance
(inaccurate BP, inappropriate drugs, nonadherence, white coat) -ID & reverse contributing lifestyle factors -d/c, dcr exogenous substances -screen & tx 2ndary causes -intensify diuretic regimen OR target SNS |
|
|
Resistant HTN:
-option 1: strengthen diuretic regimen |
-controlls ~1/2 cases of resistant HTN
-consider if: high Na+ intake, +edema, absence of incr BUN/Cr, uric acid levels & CRD -possible considerations: --chlorthalidone + K+sparing -HCTX + K sparing -replace TZD diuretic w/ Loop -loop + TZD or metolazone |
|
|
Resistant HTN:
Option 2: Target the SNS (sympathetic nervous system) |
-sympathoplegics decr sympathetic discharge/its effects
-pharmacologic targets (centrally acting agents, ganglion blockers, postganglionic sympathetic neuron blocker, adrenoreceptor blockers) |
|
|
Adrenoreceptor Blockers: Alpha 1 Receptor Antagonists:
Doxazosin |
MOA: competetively inhibits a-1 receptors -->vasodilation of arterioles & veins, decr PVR/BP as result
AEs: dizziness,HA, orthostatic hypotension*(dose related), fatigue, nausea Metab: hepatic (3A4/2C19/2D6) Pearls: shown to be more effective in combo than as monotx; do not abruptly stop medication; often used when pts also have BPH. |
|
|
Direct Vasodilators:
Hydralazine, Minoxidil Isosorbide-Dinitrate (venodilator) MOA: |
-direct relaxation of vascular smooth muscle in the resistance vessels -->result decr PVR
-reflex activation of the autonomic reflexes --> incr HR & CO -stimulates RAAS -->aldosterone release Na retention, plasma volume expansion -NOT given as monotx! |
|
|
Direct Vasodilators:
Hydralazine, Minoxidil Isosorbide-Dinitrate (venodilator) Side Effects/Monitoring |
-flushing, HA
palpitations, significant fluid retention -ECG changes, hypertrichosis -transient BUN/Scr increase Monitoring: BUN, SCr, Lytes, Fluid balance/weight |
|
|
Direct Vasodilators:
Hydralazine (Apresoline) |
-metab: hepatic acetylation, extensive first pass
Decreased M&M in HF pts when combined with **Isosorbide Dinitrate** BiDil - combo agent of both |
|
|
Direct Vasodilators:
Minoxdil (loniten) |
metabolism: glucuronidation
|
|
|
Direct Vasodilators:
Isosorbide |
MOA: Releases nitric oxide (NO) activates guanylyl cyclase
effect->Venodilation reduces preload and ventricular stretch Use for HF & angina -additive w/ other vasodilators: SE: postural hypotension, HA, tachycardia |
|
|
Renin Inhibitors:
Aliskiren |
MOA:Inhibits enzyme activity of renin
Effects: Reduces angiotensin I and II and aldosterone Indications: Hypertension Pharm: Oral Toxicity: Hyperkalemia, renal impairment potential teratogen |
|
|
Cardiac Glycoside:
Digoxin |
MOA: Na+/K+ATP-ase inhibitor
-result: decr Ca+ expulsion, incr Ca+ retention in SR Effect: incr cardiac contractility, decr sinus HR, decr AV conductn For: symptomatic HF, rapid V-rate in A-fib. Tox: N&V, diarrhea, arrythmias |
|
|
Lipid Meds:
the Statins! Atorvastatin (Lipitor) Rosuvastatin (Crestor) MOA: |
-reduce hepatic cholesterol synthesis, lower intracellular chol--> stimulates upreg of LDL receptor & incr uptake of non-HDL particles from the systemic circulation
-->BLOCKS HMG-COA REDUCTASE (decreases chol synth, upregs LDL receptors) |
|
|
Lipid Meds:
the Statins! Atorvastatin (Lipitor) Rosuvastatin (Crestor) Metabolism: |
Atorvastatin: 3A4, no renal adjustment,yes myopathy/LFT abn
Rosuvastatin: minimal 2C9, renal adjustment**, yes myopathy/LFT abn **renal if GFR <30 |
|
|
Lipid Meds:
the Statins! Atorvastatin (Lipitor) Rosuvastatin (Crestor) EFFECTS ON LIPIDS |
-reduces: LDL-C by 20-60%
-TG's by 7-30% Raises HDL by 5-15% |
|
|
Lipid Meds:
the Statins! Atorvastatin (Lipitor) Rosuvastatin (Crestor) SIDE EFFECTS/CONTRAIND |
major (rare):
-myopathy (rhabdomyalisis) -incr liver enzymes Contraindications: -absolute: liver disease -relative: use w/ certain drugs (fibrates, niacin) |
|
|
Lipid Meds:
the Statins! Atorvastatin (Lipitor) Rosuvastatin (Crestor) DRUG INTRXNS |
-CYP 3A4 (HAART, amiodarone, macrolides, antifungals, cyclosporine)
-fibrates (gemfibrozil) |
|
|
Cholesterol Absorption Inhibitor:
Ezetimibe (Zetia) MOA: |
MOA: cholesterol absorption inhibitor, decreases it at brush border of SI (NPC1L1 recptor)
-decr delivery of intestinal chol to the liver -upregulation of LDL receptors |
|
|
Cholesterol Absorption Inhibitor:
Ezetimibe (Zetia) tx/lipid effects |
-monotx: low SE but also not potent. -see modest decr in LDL
-doesn't do much for HDL -best suited for person who cannot tolerate statin --Lipid Effects: reduces LDL 15-20% |
|
|
Cholesterol Absorption Inhibitor:
Ezetimibe (Zetia) side effects, drug interactions |
SE: absorbed & metabolised to active drug
-SE are RARE: incr liver enzymes (with statin at same time) -myopathy? Drug Interactions: no major ones |
|
|
Bile Acid Binding Resins:
Cholestyramine (Questran) MOA: |
-binds bile acids
-reduces enterohepatic recirculation of cholesterol -reduces intracellular cholesterol -upregulation of LDL receptors |
|
|
Bile Acid Binding Resins:
Cholestyramine (Questran) Lipid effects: |
-reduces LDL 15-30%
-raise HDL by 3-5% -may increase TG -Welchol -reduce HgA1c tiny bit |
|
|
Bile Acid Binding Resins:
Cholestyramine (Questran) Contraindications/SE |
Contraindications: raised TG (esp >400 mg/dL)
SE: GI distress/constipation -decreased absorption of other drugs ex: digoxin, thyroxin, warfarin (take 1 hour after or 4 hours before other meds) -Not absorbed, not metabolised |
|
|
the Fibrates:
Fenofibrate (Tricor) MOA: |
-PPAR-alpha agonists (transcription factor)
-increase HDL -decr TG and VLDL (incr their metabolism) |
|
|
the Fibrates:
Fenofibrate (Tricor) pharmacology & take home point |
-decrease dose in renal impairment, if severe decrease dose of all kinds of fibrates
-metab: hepatic: glucouronidation clearance: urine 60%, poo 25% |
|
|
the Fibrates:
Fenofibrate (Tricor) lipid effects, |
-lower TG 20-50%
-raise HDL 10-20% -lower LDL 5-20% (may raise LDL with high TG) |
|
|
the Fibrates:
Fenofibrate (Tricor) SE/Contraindications |
SE: dyspepsia, gallstones, myopathy, hepatitis
Contraind: -severe renal/hepatic dz -strong caution w/ statins!! -->myopathy (gemfibrozil) |
|
|
Niacin:
Niaspan MOA: |
-decreased FFA to liver, & TG production
-->decreased VLDL -decreased HDL catabolism (of Apo A1 protein) -->increased HDL levels |
|
|
Niacin:
Niaspan Side effects/drug forms |
-forms: immediate release, extended release, sustained relase.
SE: flushing, INCR glucose & uric acid!!! -GI distress -hepatotoxicity |
|
|
Niacin:
Niaspan Contraindications/ Lipid effects: |
-contraind: liver dz, severe gout, peptic ulcer, incr LFT abnormalities/myopathy w/ statins
Lipid effects: lowers TG 20-50%, raises HDL 15-35%, lowers LDL 5-25% |
|
|
Niacin:
Niaspan Flushing Tips |
-take aspirin 30 min before
-take w/ food -take in evening -long acting preparations -slowly titrate -warn the patient! |
|
|
Fish Oil (omega 3 FA's)
Lovaza MOA: |
-decr fatty acid delivery to liver
-decr TG production (blocks enzymes that lead to TG synthesis, shunts FA's toward breakdown) |
|
|
Fish Oil (omega 3 FA's)
Lovaza Lipid Effects |
-lowers TG 30-40%
-minimal change in HDL -incr or decr LDL |
|
|
Fish Oil (omega 3 FA's)
Lovaza SE/Contraindications |
SE: fishy taste, belching, incr bleeding (not really)
No contraidications |
|
|
Receptors:
a1 a2 |
a1- vasculature, vasoconstriction (eye, GI/GU)
a2- presynaptic, vasoconstriction |
|
|
receptors:
B1 B2 V1 DA |
B1- cardiac - incr HR & contractilty
B2-vasculature - vasodilation V1- vasculature, vasoconstriction DA (dopamine) vasculature (renal/mesenteric), vasodilation |
|
|
Shock Syndromes:
Hypovolemic |
PCWP:-> decr
CO: decr SVR: incr x 3 (ex: dehydration, trauma, anemia) |
|
|
Shock Syndromes:
Cardiogenic |
PCWP: incr
CO: decr x 2 SVR: incr x 3 ex: s/p cardiac arrest, PE's, pump failure |
|
|
Shock Syndromes:
Distributive |
PCWP: decr or no change
CO: incr x2 SVR: decr x 3 ex: sepsis, 3rd spacing, leaky capillaries |
|
|
Dopamine:
MOA: |
-release of norepinephrine from sympathetic nerves
-direct stimulation of B1, a1, DA receptors -selectively increases renal/splanchnic flow |
|
|
Dopamine:
Dose-dependent affects |
-low dose: DA receptors
-medium dose: beta recptors -high dose: alpha receptors |
|
|
Dopamine:
Indications & Adverse Effects: |
-indication: improve blood pressure & CO in setting of shock
-Adverse effects: -tachycardia -arrhythmias (use in distributive/hypovolemic shock) |
|
|
DoBUTAmine:
|
-inotropic agent:
-MOA: stimulates B2 receptors of heart, some B2 effects/vasodilatn -Indication: inotropic support, short term mgmt of CHF when incr CO needed -Adverse effects: incr HR, V-tach, hypotension (hi doses) --only for cardiogenic shock |
|
|
Epinephrine:
|
MOA: directly stimlates B1,B2, a1
Indications: V-fib, pulseless v-tach, pulseless electrical activity, asystole, sx bradycardia, severe hypotension, anaphylaxis AE: tachycardia, arrhythmias, incr myocardial O2 demand -->hypovolemic, distrib, not cardiogenic. last line for septic shock |
|
|
Norepinephrine:
|
-MOA: stimulates B1 and a1 adrenergic receptors (a >B)
Indication: hypotension refractory to fluids -causes LEAST amt of tachycardia -close 2nd to dopamine. -septic shock |
|
|
Phenylephrine:
|
PURE a1 agonist --> peripheral vasoconstriction
-Indications: drug induced hypotension, head/spinal cord injury (head traumas, ODs) -for hypovolemic, distributive shock |
|
|
Vasopressin:
|
Indications: VF, pulseless VT, PEA, asystole, refractory hypotension, (sepsis/SIRS) diabetes insipidus
AE: hypertension, bradycardia, myocardial ischemia**, tissue necrosis. -->hypovolemic/distributive shock |
|
|
Milrinone:
|
-MOA: decr breakdown of cAMP phosphodiesterase activity, incr cAMP resulting in inotropic effects
Indications: CHF/ pulmonary HTN AE: V-arrhythmias, supraventricular arrhythmias, hypotension, angina, chest pain, HA. a LAST LINE TX. |
|
|
NItroglycerine:
|
MOA: incr coronary blood flow by dilating coronary arteries/imprv collateral flow
lo-dose: produces venodilation, decr LV end-diastolic pressur/vol Hi-dose:produces arterial vasodilation, decr afterload Indications: chest pain, acute MI, acute pulmonary edema --Not Effective when used alone as systemic antihypertensive -pts can develop tolerance |
|
|
Sodium Nitroprusside:
|
-MOA: peripheral vasodilaion via direct relaxation of venous/arterial smooth muscle, results in preload/afterload reduction (also stimulates cGMP)
-Indications: hypertensive emergency, acute decomp HF -AE; hypotension, rebound hypertension, cyanide toxicity -use in pts with renal failure |
|
|
Nesiritide:
|
-recombinant human atrial naturetic peptide
-MOA: incr cGMP causing smooth muscle cell relaxation, natriuresis, diuresis -indicated for acute decomp HF -may cause hypotension (long half life) |
|
|
Beta Blockers Review:
|
-MOA: antagonize B1 (heart) and B-adrenergic receptors
-B2-bronchial & vascular smooth muscle Class II antiarrhythmic agents |
|
|
Esmolol:
|
-ultra short acting, selective B1 blocker, at hi doses will inhibit B1/B2
-Indication: supraventricular tachycardias & BP control -AE: hypotension/bradycardia |
|
|
Labetalol:
|
MOA: non-selective beta blocker and a1 adrenergic blocker resulting in peripheral vasodilation
Indication: *hypertensive emergency* -for recent cocaine use, test in urine -AE: hypotension, bradycardia |
|
|
Nicardipine:
a dihydropyridine |
DHP-CCB: more selective for smooth muscle
MOA: inhibits txport of Ca+ into myocardial & vascular smooth muscle-->causes dilation of main coronary/systemic arteries Indication: hypertensive emergency (s/s end organ fail) -AE: hypotension,flushing, syncope, palpitations, tachycardia |
|
|
Analgesics/Sedatives:
general indications |
indications: mechanical ventillation, procedural sedation, moderate (conscious) sedation
-agents do not always have combined effects |
|
|
Analgesics/Sedatives:
Continuous Infusion pros/cons |
Pros: consistent level of sedation
-possible decr risk of adverse events Cons: adjust to pt needs, can be difficult, difficult to assess neuro function, need for loading doses, potential for drug accumulation/over-sedation |
|
|
Analgesics/Sedatives:
Bolus/Continuous Infusion Steady-State |
-the 'true' effect of a drug @ steady state
-Steady state = amount of drug going into body = amount of drug going out of body. (5 half lives) |
|
|
Fentanyl:
|
MOA: highly lipophilic agent, binds to opiate receptors in CNS
Additive effect when used w/ benzos/propafol -Indications: analgesia, additive sedation -AE: hypotension, bradycardia, respiratory depression, constipation |
|
|
Morphine:
|
MOA: binds opiate receptors in CNS
-Indication: pain control, palliative care -Active metabolite, renally eliminated Histamine release, long duration of action. -onset: 8 min antidote: narcam |
|
|
Propafol
|
MOA: not fully understood, thought of as an anaesthetic
Indication: sedation, general anaesthesia -highly lipophilic -short duration of action, ideal for frequent neuro checks -no analgesic effects! -->AE: itching, hypotension, bradycardia, propofol infusion syndrome (metabolic acidosis when on it for a long time) --hyperTG-emia |
|
|
Benzodiazepines
in general |
MOA: potentiates GABA
Effect: sedative, amnestic, anxiolytic, anticonvulsant AE: hypotension, respiratory depression Antidote: flumazenil (may precip seizures) ALWAYS bolus first, start lo, go slow. |
|
|
Midazolam:
|
-highly lipophilic
-short acting benzodiazepine -active metabolite (alpha hydroxymidazolam) that is renally eliminated Pharm Pearl: --accumulates p 24 hrs of continuous infusion -incr duration of action -Indications: conscious sedation, agitation, anxiolysis |
|
|
neuromuscular blocking agents:
in general non-depolarizing/depolarizing |
-NON: acts as antagonist by competing with Ach for nicotinic cholinergic receptors of motor end plate
DEPOLAR: acts as AGonist at the nicotinic cholinergic receptors on the motor endplate, produces fasciculations |
|
|
Indications for NMBA (neuromuscular blocking agents)
in the ICU |
-manage mechanical vent
-manage intracranial pressure -treat muscle spasms -decr O2 consumption -rapid sequence intubation (RSI) |
|
|
NMBA's:
Clinical Pearls |
-no sedative, amnestic or analgesic properties!!
-pts must receive sedation before admin of NMBA -pts receiving long-term paralysis should get: -DVT prophylaxis -corneal abrasion prevention -train of four monitorin (paralysis watch) -monitor for pressure ulcers Reversal agents: Physostigmine, neostigmine |
|
|
Succinylcholine
|
-depolarizing NMBA (only one)
-Indication: short-term paralysis, RSI -AE: K+ release, existing renal dysfunction, burns, crush injuries -can increase intracranial/intraocular pressures -fasciculations |
|
|
Atracurium:
|
-benzylisoquinolinium, non-depolarizing NMBA
-Indication: long-term paralysis -AE: histamine release, CNS exictation w/ hepatic failure, tachyphylaxis -Metab: hoffman elimination (laudanosine), ester hydrolysis, pH & temperature dependent |
|
|
physiology of clot formation:
|
-clots: composed of platelets & RBCs
-Hemostasis: body's natural mechanism by which bleeding is stopped to prevent blood loss (vascular spasm, platelet plug formation, generation of thrombin-->via clotting cascade) |
|
|
Platelet Plug formation:
|
-platelet activation (tissue injury-->collagen, vWF, TF)
-platelet adhesion (expose binding sites, TXA2 synthesis) -platelet aggregation |
|
|
Aspirin:
MOA |
-irreversible inhibition of cyclooxygenase (COX) -->COX1--> Thromboxane A2 (TXA2)
-it antagonizes the TA2 pathway which reduces platelet production |
|
|
Aspirin:
Clincial Indications/Pharmacokinetics |
CI: pain, fever, inflammation, RA, OA. Prophylaxis of: MI, stroke, TIA, CABG, PTCA (stenting)
-Pharmkinetics:-> only available PO. hepatic metabolism. renal excretion. 1-2 hours to peak, t1/2=15-20 min |
|
|
Aspirin:
Adverse Effects Drug Rxn Monitoring |
AE: bleeding, gastric/duoden ulcers
asthma exacerbation, Reye's, acid-base disturbances DrugRxn: with anticoagulatns/antiplatelets, ACEI, alcohol, steroids, NSAIDs, Phenytoin. Monitoring: signs of bleeding (hgb, hct, platelets) renal function (SCr, CrCL) resolution of pain, allergies. |
|
|
Aspirin:
Clinical Pearls |
-drug of choice for cardiac events
-pregnancy category C (first tri) & D in 3rd/4th?? -Reye's syndrome -do not use in renal dysfunction -available OTC abundantly -check for drug intrxns |
|
|
Aggrenox
(ASA + dipyradamole) MOA: Clinical Uses: |
-additive effects:
-->dipyridamole inhibits adenosine uptake in cells -->ASA- irreversible inhibition of COX-->COX1-->TXA2 Clinical: -decr risk of stroke in pts with transient ischemia of brain/complete ischemia due to thrombosis (3rd line) |
|
|
Aggrenox
(ASA + dipyradamole) Pharm |
ASA: only availble PO, hepatic metab, renal excretion. dose dependent.
Diyridamole: only available PO, hepatic metab. different half-life |
|
|
Aggrenox
(ASA + dipyradamole) AE & monitoring |
AE: bleeing, GI, HA (30% pts)
monitoring: SCr, (CrCL) Hgb, Hct, platelets S&S of bleeding or stroke |
|
|
Aggrenox
(ASA + dipyradamole) Clinical Pearls: |
-dipyridamole rarely used by itself
-NOT first line tx for stroke -ASA content is only 25 mg!!! -most likely reason for d/c is HA (up to 30%) -due to antiplatelet effects, use w/ caution in combination w/ other antiplatelets or anticoags |
|
|
ADP Inhibitors: thienopyridines
Ticlidopine (Ticlid) Clopidogrel (plavix) AE: Drug interaxns |
AE: bleeding, risk of gastritis, TTP, neutropenia (only with Ticlopidine)
Drug Interxns: concomitant antiplatelets/anticoagulants NSAIDs, CYP inhibitors/inducers (CYP2C19, 3A4, 2B6) |
|
|
ADP Inhibitors: thienopyridines
Ticlidopine (Ticlid) PK/PD |
-absorption 80-90%
-metab: liver -onset 6hrs -t1/2 -12-36 hrs, incr to 4-5 days with repeated use |
|
|
ADP Inhibitors: thienopyridines
Clopidogrel (Plavix) PK/PD |
-absorptin: well absrbd
-t1/2: 7-8 hours -peak- 1hr -metab: hepatic to active metabolite -inhibition of platelet aggregation: 2 hrs p 300 mg -CYP2C19 pharmacogenetics (means a genetic resistance to ASA/drugs like it) |
|
|
ADP Inhibitors: thienopyridines
Monitoring parameters |
-CBC, Hgb, Hct, platelets
-LFTs -CYP2C19 pharmacogenetic assays (only with clopidogrel) -if they stroke, indicative of genetic resistance |
|
|
ADP Inhibitors: thienopyridines
Clinical Pearls |
-Clopidogrel/prasuragrel require activation to active form
-review all pts for allergies/drug interactions -incr risk of GI bleeds -neutropenia risk with ticlopidine -in pts with PTCA/stent: -BMS=ASA + clopidogrel/parasurgel 4 weeks -DES= ASA + clopidogrel/prasugrel for at least 12 weks |
|
|
GPIIb/IIIa Inhibitors
Abciximab (Reopro) MOA: |
-non-competetive blocking of the platelet glycoprotein IIb/IIIa receptor complex (the final common pathyway --> inhibits platelet aggregation
|
|
|
GPIIb/IIIa Inhibitors
Abciximab (Reopro) Structure, antibodies other facts |
structure: antibody
antibodies?: yes binding: irreversible indication: PCI no renal dosing, <10 min to 80% inhibition. half life- 30 min to 15 days |
|
|
GPIIb/IIIa Inhibitors
Abciximab (Reopro) AE & Drug Intrxns |
AE: bleeding, thrombocytopenia
N&V, hypotension, bradycardia, HA, hypersensitivity Drug Intrxns: antiplatelets, anticoagulants, NSAIDs |
|
|
GPIIb/IIIa Inhibitors
Abciximab (Reopro) Monitoring/ Clinical Pearls |
Monitor: aPTT, ACT (activated clotting time)
CBC (bleeding), SCr,CrCL, hypersensitivity, thrombocytopenia Pearls; -abciximab can cause hypersensitivity rxns -have short half life compared to other anti-platelets -MUST monitor ACT to assess clinical efficacy -recommend for hi-risk pts -VERY costly |
|
|
Thrombolytics:
Alteplase (Activase, tPA) MOA/Indications |
MOA: helps plasminogen convert to plasmin -->degrades fibrin
Indications: STEMI, AIS, PE, line clots (tPA only) |
|
|
Thrombolytics:
Alteplase (Activase, tPA) Adverse Events: |
-hemorrhagic stroke
-cardiac rupture -bleeding -allergic reaction (mostly streptokinase) -fever -hypotension/LFT elevations |
|
|
Thrombolytics:
Alteplase (Activase, tPA) Drug interactions/monitoring |
-interactions: anticoagulants, antiplatelets, NSAIDs
Monitoring: -signs of bleeding, CBC, LFTs, aPTT & PT, (not routinely used for clincal efficacy) |
|
|
Thrombolytics:
Alteplase (Activase, tPA) Clinical Pearls |
-alteplase given w/in 3 hrs of sx onset for ischemic stroke
-thrombolytics for STEMI ONLY should be given in 12 hours -risk of local after clot lysis -incr risk of bleeding (since given with other antiplatelet/anticoagulants) Antidotes: amiocaproic acid, aprotinin (inhibit streptokinase activity) |
|
|
Cilostazol (Pletal)
|
Cilostazol is a newer phosphodiesterase inhibitor that promotes vasodilation and inhibition of platelet aggregation. Cilostazol is used primarily to treat intermittent claudication.
|
|
|
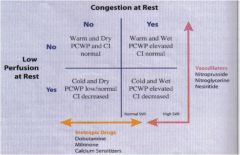
Classifying Severity of HF:
Forrester |
Warm & Dry (1)-PCWP/Cardiac index normal
|
|
|
forrester classification
|
|
|
subdural hematoma
|
accumulation of blood beneath the dura mater caused by relatively slow venous bleeding, owing to head trauma that is usually not severe enough to cause skull fracture
-bleeding occurs from small veins that bridge the subdural space from the superior saggital sinus to the brain surface & accumulates a mass that pushes the brain aside DIFFERS from epidural hematoma in that: in subdural bleeding is slow and venous. epidural is fast and arterial |
|
|
subarachnoid hemorrhage
|
->any bleeding into the subarachnoid space
-usually sudden & not assoc w/ trauma or precipitating cause -the most common cause is trauma. |
|
|
2 main causes of sponatneous non-traumatic subarachnoid hemorraghe
|
-saccular (berry) aneurysms (after birth development) MOST COMMON CAUSE of spontaneous rupture of a sub-A Hemorrhage
-vascular malformations (congenital) |
|
|
vascular malformations
|
-congenital malformations that can also cause spontaneous intracranial bleeding
-vascular malformations usually occur on the surface of the cerebral hemisphere & are formed by tangled masses of arteries/veins or mixture. they may also be a source of seizures |
|
|
medical history of people with white strokes
|
-DM, atherosclerosis, valvular heart disease, HTN,
especially coronary vascular disease |
|
|
transient ischemic attacks
|
-dizziness, syncope, focal weakness, or other neurologic symptoms
-25% of pts with TIAs will have a white stroke w/in 5 years |
|
|
laminar cortical necrosis
|
a superficial layer of dead neurons of the cerebral cortex
|
|
|
diffuse axonal injury
|
-occurs when sudden/severe twisting motion of the head
can stretch brain nerve tracts to the point of injury -gross abnormalities may be minimal but severe deficits can occur |
|
|
meningitis
|
-inflammation of the meninges
-almost always from infection by viruses or pyogenic bacteria: acute prurulent: (aerobic bact: E coli, Haeomphilus influenzae, S. pneumoniae, N menigitidis) -pus in the CSF & over surface of brain -viral is much less threatening -chronic can be from tubercle bacilli, syphillis, fungi |
|
|
brain abscess
|
-localized area of dead, liquefied tissue
-acute inflammatory cell exudate caused by bacterial infection -lungs are important in etiology: blood borne spread arises from lung abscess -viral are generalized infections: |
|
|
spongiform encephalitides
|
-group of universally fatal, very rare diseases : prions, mad cow
-most notable: Creutzfeldt Jakob disease |
|
|
degenerative brain diseases: common features;
|
-have no known cause, but some are inheritable
-occur in selected ares of gray matter while leaving others unaffected -abnormal protein deposits in affected tissue -are associated with dementia |
|
|
Huntington disease
|
-autosomal dominant genetic disease traced to a defect on chromosome 4
-most are inherited -white people. doesn't become symptomatic till 30-40 years old - |
|
|
leukodystrophies
|
-group of autosomal recessive genetic demyelinating diseases
-DNA coding defect for enzyme proteins important in the production & maintenance of healthy myelin -lesions found in white matter. -diseases of infancy/childhood -metachromic leukodystrophy |
|
|
Wernicke encephalopathy
|
-cerebellar atrophy, ataxia, tremors, confusion
-paralysis of extraocular muscles -untreated can turn into Korsakoff psychosis: permanent defect in long & short term memory |
|
|
other genetic/metabolic conditions of the brain:
|
-cretinism: infantile hypothyroidism
-PKU - -wilson disease -neuronal storage diseases (Gaucher) |
|
|
brain tumors : basics
|
-half originate in the cranium & include:
--tumors of brain cells (glia, neurons, related embryonic cells) --tumors of cranial nerves & meninges -all others (20%) |
|
|
gliomas
astrocytoma, oligodendroma ependymoma |
-astrocytomas: most common
-mostly in adult, classified by microscopic grade: --low grade: early in life, leas aggressive --intermediate grade: uncommon, 3 year survival --high grade: glioblastoma multiforme, older adults, fatal |
|
|
oligodendromas
|
-tumors of cells that form myelin
- |

