![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
37 Cards in this Set
- Front
- Back
|
Diuretics - classification in order of site of action
|
COLT Pee (in their sequential site of action). PCT: Carbonic anhydrase inhibitors, Loop of Henle: Osmotic diuretics, Ascending loop of Henle: Loop diuretics, DCT: thiazides, CT: potassium-sparing diuretics
|
|
|
Osmotic diuretics - members
|
GUM: Glycerol, Urea, Mannitol
|
|
|
Classification of antihypertensive drugs
a. Diuretics (3) b. Drugs that interfere with the renin-angiotensin system (3) c. Drugs that decrease peripheral vascular resistance or cardiac output (2 groups with subgroups) |
a.
1. Thiazides 2. Loop diuretics 3. Potassium-sparing diuretics b. 1. ACE inhibitors 2. ATII receptor antagonists 3. Aldosterone antagonists c. 1. Direct vasodilators: Ca-channel blockers, nitrates 2. Sympathetic nervous system depressants: alpha- and beta-blockers, clonidine (Stringer) |
|
|
Thiazide diuretics
a. Members (5) b. Mechanism, where c. Potassium wasting or sparing? d. Drugs of choice for? |
a.
1. Chlorothiazide 2. Hydrochlorothiazide 3. Chlorthalidone 4. Metolazone 5. Indapamide b. Inhibit NaCl reabsorption in the TAL and early distal tubule c. Potassium wasting d. Treatment of primary hypertension (Stringer) |
|
|
ACE inhibitors
a. Members (5) b. Most important use (2) c. Side effects (6) |
a. (-prils)
1. Captopril 2. Enalapril 3. Benazepril 4. Fosinopril 5. Lisinopril b. 1. Hypertension (Especially useful in hypertension secondary to increased renin levels) (Used in diabetics since it don't influence the glucose levels.) 2. Heart failure c. 1. Headache 2. Dizziness 3. Confusion 4. Abdominal pain 5. Renal failure 6. Impotence 7. Dry cough (associated with bradykinin, ACE presumably inhibit this substance as well) (Stringer) |
|
|
ATII receptor antagonists
a. Members (3) b. Difference from ACE inhibitors |
a. (-Sartans)
1. Candesartan 2. Eprosartan 3. Losartan b. Don't produce cough, which is mediated by ACE (Stringer) |
|
|
Selective aldosterone receptor antagonist - members (2)
|
1. Eplerenone
2. Spironolactone (Stringer) |
|
|
Calcium channel blockers
a. Members (5) b. Effect |
a. (-dipine, -mil)
1. Diltiazem (Only exception to suffix rule) 2. Nifedipine 3. Verapamil 4. Amlodipine 5. Felodipine b. Decrease afterload. (Effect and side-effect are caused by vasodilation) (Stringer) |
|
|
Nitrates
a. Members (5 b. Effect c. What is the most commonly used antianginal agent, and the drug of choice for relieving acute coronary spasm? d. Which is an orally active nitrate that has the longest half-life? e. Which is used as continuous IV infusion to treat hypertensive emergencies? f. Side effects |
a.
1. Nitroglycerin 2. Amyl nitrite 3. Isosorbide dinitrate 4. Isosorbide mononitrate 5. Nitroprusside b. Vasodilate and reduce cardiac preload. (Work by conversion to nitric oxide -> cGMP -> smooth muscle relaxation) (Reduce afterload at higher concentrations) c. Nitroglycerin d. Isosorbide dinitrate e. Nitroprusside f. 1. Postural hypotension 2. Headache (Excessive cerebral vasodilation = headache) (Stringer) |
|
|
Other direct vasodilators (3)
|
1. Hydralazine
2. Minoxidil (1 and 2 directly relax arterioles by unclear mechanism, reflex tachycardia & increased renin) (Minoxidil cause unwanted hair growth, its marketed for topical treatment of baldness as Rogaine) 3. Fenoldopam (dilates renal and mesenteric vascular beds by acting as a selective DA1 receptor agonist) (Stringer) |
|
|
Beta-blockers used to treat hypertension
a. Beta-1 antagonists (5) b. Beta-1 antagonist with some sympathomimetic activity (2) c. Beta-1 and 2 antagonist (4) |
a.
1. Atenolol 2. Betaxolol 3. Carteolol 4. Metoprolol 5. Penbutolol b. Acebutolol, Esmolol c. 1. Propranolol 2. Nadolol 3. Timolol 4. Pindolol (some sympathomimetic activity as well) (Stringer) |
|
|
Centrally acting antihypertensive drugs (3)
|
1. Clonidine (alpha-2 adrenergic agonist)
2. Methyldopa (alpha-methyldopa) 3. Guanabenz (Side effects include drowsiness and dry mouth (anticholinergic)) (Stringer) |
|
|
Standard symptomatic treatment for congestive heart failure
|
1. Loop diuretic
2. Rapidly acting vasodilator or drug that increase contractility (Stringer) |
|
|
Why is nitroprusside used in acute heart failure?
|
It reduce both preload and afterload without affecting contractility.
(Stringer) |
|
|
Nesiritide - what? effect?
|
Recombinant form of human B-type natriuretic peptide.
Hormone naturally produced by the ventricle which produce natriuresis, diuresis, and vasodilation by increasing cGMP levels. (Stringer) |
|
|
Cardiac glycosides
a. Members b. Derived from c. Mechanism d. Therapeutic index e. Toxicity is more common in patients with? |
a. Digoxin, Digitoxin
b. The Digitalis purpurea plant (Foxglove plant) c. 1. Improve cardiac contractility by inhibiting Na-K-ATPase -> increased intracellular Na -> inhibit ion exchanger (3Na-Ca) which transport calcium out and Na in -> intracellular Ca 2. Increased intracellular calcium -> increased uptake of Ca into SER by SERCA -> more Ca can be released upon stimulation 3. Increase the sensitivity of the AV node to vagal stimulation -> slow ventricular rate in atrial flutter or fibrillaton d. 1.6-2.5 e. Hypokalemia (Digitalis competes with potassium for binding on the Na-K-ATPase) (Also hypercalcemia and hypomagnesemia. Hypercalcemia enhances digitalis-induced increases in intracellular calcium, which can lead to calcium overload and increased susceptibility to digitalis-induced arrhythmias. Hypomagnesemia also sensitizes the heart to digitalis-induced arrhythmias.) f. 1. Arrhythmias 2. Anorexia, nausea, diarrhea 3. Drowsiness and fatigue 4. Visual disturbances (Stringer) |
|
|
Inamrinone and Milrinone
a. What b. Used for c. Mechanism |
a. cAMP phosphodiesterase inhibitor in cardiac and vascular muscle.
b. Congestive heart failure c. Positive inotropic and vasodilatory effect. (Stringer) |
|
|
Draw the ventricular action potential and explain the phases.
|
Phase 0: Rapid depolarization
Opening of voltage-gated sodium channels (fast sodium channels) (Potassium channels simultaneously close) Phase 1: Partial repolarization Opening of a special type of transient K channel Phase 2 - Plateau phase Repolarization is delayed because of the simultaneous increase in slow inward conductance of Ca and the plateau phase is maintained. Phase 3 - Repolarization Increased potassium conductance and inactivation of Ca channels Phase 4 - resting potential (www.cvphysiology.com) |
|
|
Draw the ventricular action potential and explain the phases.
|
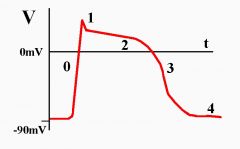
Phase 0: Rapid depolarization
Opening of voltage-gated sodium channels (fast sodium channels) (Potassium channels simultaneously close) Phase 1: Partial repolarization Opening of a special type of transient K channel Phase 2 - Plateau phase Repolarization is delayed because of the simultaneous increase in slow inward conductance of Ca and the plateau phase is maintained. Phase 3 - Repolarization Increased potassium conductance and inactivation of Ca channels Phase 4 - resting potential (www.cvphysiology.com) |
|
|
Class I antiarrhythmic drugs
a. Act on which phase of the cardiac action potential? b. General effect (2) c. IA: effect, members (3), use d. IB: effect, members (4), use e. IC: effect, members (4), use |
a. Phase 0 - rapid depolarization phase
b. Decrease the rate of rise of phase 0 of the action potential and suppress automoaticity of the Purkinje fibers and His bundle. c. IA: Slow the rate of rise of phase 0 and prolong the effective refractory period of the ventricle. 1. Procainamide 2. Quinidine (related to quinine and also have antimalarian actions) 3. Disopyramide Treatment of atrial and ventricular arrhythmias. d. IB Less of an effect on phase 0, but shorten the action potential duration and refractory period of the Purkinje fibers. 1. Lidocaine (drug of choice) 2. Mexiletine 3. Phenytoin 4. Tocainide Against ventricular arrhythmias (VT, VF, ventricular ectopy) e. IC Greatest prolongation of the early depolarization phase and have less of an effect on the refractory period of the ventricle. 1. Encainide 2. Flecainide 3. Indecaininde 4. Propafenone Against ventricular arrhythmias (Flecaininde and propafenone are absorbed orally and are used for chronic suppression of ventricular arrhythmias.) (Refractory period - the period following effective stimulation, during which excitable tissue such as heart muscle and nerve fails to respond to a stimulus of threshold intensity) (Stringer) |
|
|
Class I antiarrhythmic drugs
a. Which agent has features of all three subclasses b. Mechanism |
a. Moricizine
b. It inhibits sodium influx through fast sodium channels in cardiac tissue in a use-dependent fashion (the more the channel is used, the more it is blocked) |
|
|
Class II antiarrhythmics
a. Synonym b. Mechanism (3) c. Particularly used against d. Which beta-blocker is most commonly used to treat patients with arrhythmias |
a. Beta-blockers.
b. The mechanism of action of these drugs, in terms of rhythm stabilization is unknown, but they cause 1. Cardiac membrane stabilization 2. Slowed conduction through AV and SA node 3. Increased refractory period c. Suppressing tachyarrhythmias that result from increased sympathetic activity. d. Propranolol. (Stringer) |
|
|
Class III antiarrhythmics
a. Synonym b. Effect c. Members (5) d. Very useful in treating .... e. Which agent is used to convert atrial fibrillation and maintain sinus rhythm after cardioversion |
a. Potassium channel blockers
b. Complex, but they all prolong the duration of the action potential without altering phase 0 depolarization or the resting membrane potential. c. 1. Bretylium 2. Amiodarone 3. Dofetilide 4. Ibutilide (Don't block potasium currents. It promotes influx of sodium through slow inward sodium channels -> prolongation of the action potential) 5. Sotalol d. Intractable ventricular arrhythmias (VT and VF) e. Dofetilide (Stringer) |
|
|
Class IV antiarrhythmics
a. Synonym b. Mechanism and effect c. Most effective against |
a. Calcium channel blockers
b. Block the slow inward calcium current during phases 0 and 2 of the cardiac cycle -> slow conduction and prolong the effective refractory period, especially in the AV node (May terminate reentrant arrhythmias that require the AV node for conduction) c. Atrial arrhythmias (Stringer) |
|
|
Other antiarrhythmic drugs
a. Adenosine - drug of choice for, mechanism b. Digoxin\Cardiac glycosides - effect, effective for |
a. Paroxysmal supraventricular tachycardia
It depress SA and AV node activity. (Effective because the most common form of paroxysmal supraventricular tachycardia involves a reentrant pathway, half-life of seconds) b. Slow conduction through the AV node and increase its refractory period -> control ventricular rate in atrial tachyarrrhythmia (AF, or atrial flutter) (Stringer) |
|
|
Antiarrhythmics - synonym for group and name of most common agent
a. Class IA b. Class IB c. Class IC d. Class I with functions associated with several subdivisions e. Class II f. Class III g. Class IV h. Other agents (2) |
a. Class IA - Procainamide (\Quinidine)
b. Class IB - Lidocaine c. Class IC - Encainide d. Class I mixed - Moricizine e. Class II\Beta-blockers - Propranolol f. Class III\Potassium channel blockers - Amiodarone (Bretylium) g. Class IV\Calcium channel blockers - Verapamil h. Adenosine, Cardiac glycosides (Stringer) |
|
|
Antiplatelet agents
|
1. NSAIDS, including aspirin
(Inhibit COX -> inhibit TXA2 formation in platelets) 2. Anagrelide 3. Clopidogrel 4. Dipyridamol 5. Ridogrel 6. Ticlopidine 7. IIB\IIIA receptor antagonists Abciximab, Eptifibatide, Tirofiban (Fibrinogen and vWF bind to this receptor on the platelet) (Stringer) |
|
|
Antiplatelet agents
a. Dipyridamole - mechanism b. Ticlodipine and Clopidogrel (plavix) - mechanism c. Abciximab, eptifibatide, and tirofiban - mechanism |
a. Dipyridamole
Phosphodiesterase inhibitor -> increase cAMP in platelets -> decrease platelet adhesion to damaged endothelium. (Also used as antianginal for its coronary vasodilator properties. Then in combination with aspirin or warfarin.) (Don't alter bleeding time) b. Ticlodipine and Clopidogrel (Plavix) Inhibit platelet aggregation by inactivating the platelet P2Y ADP receptor. (Prolong bleeding time) c. Abciximab, eptifibatide, and tirofiban Platelet glycoprotein IIb\IIIa receptor antagonists. Prevent vWF and fibrinogen (bridging platelets) from binding here and thus prevents platelet aggregation. (Abciximab is a monoclonal antibody, the other two are receptor antagonist (Stringer) |
|
|
Antiplatelet agents - mechanisms
a. Ridogrel b. Anagrelide |
a. Inhibit the arachidonic acid pathway at two sites.
I. Prostaglandin endoperoxide receptor antagonist (Protein complex, catalyze COX, and hydroperoxidase activity which use glutathione to convert PGG2 to PGH2) II. Inhibit TXA2 synthase b. I. Inhibit platelet aggregation II. Reduce platelet count (Probably by inhibiting megakaryocyte development in the late, postmitotic stage.) (Stringer) |
|
|
Anticoagulant drugs - classification
|
1. Heparin and LMWH
Heparin (-arins. Ardeparin, Dalteparin, Enoxaparin, Tinzaparin, Danaparoid) 2. Oral anticoagulants Warfarin Dicumarol 3. Thrombin inhibitors -irudins. I. Hirudin II. Desirudin III. Lepirudin IV. Argatroban 4. Others I. Fondaparinux II. Drotrecogin alfa (The indication is PREVENTION of thrombus. They can not dissolve an already formed venous or arterial thrombus.) (Stringer) |
|
|
Anticoagulant drugs - heparin and LMWH
a. Mechanism b. What are LMWH and what are their advantage c. What are the antagonist to heparin |
a.
1. Potentiate antithrombin III which inhibits thrombin (IIa) (Exist AD ATIII deficiency) 2. Also inactivate IXa-XIIIa b. Oligosaccharide extracts from heparin. larger anti-Xa to anti-IIa activity -> can be used at lower doses, greater bioavailability and half-life when giving subcutaneously. c. Protamine sufate (Used to treat heparin-induced hemorrhage. Basic proteins that have a high affinity for the negatively charged heparin.) (Stringer) |
|
|
Warfarin and dicumarol
a. Clinical applications b. How can an warfarin overdose be treated |
a. Warfarin is the oral anticoagulant of choice, used for long-term therapy.
b. By giving vitamin K, but this takes about 24 hours. (Takes time to make new coagulation factors.) (Exist many drug interactions for the oral anticoagulants.) (Stringer) |
|
|
Anticoagulants
a. Direct thrombin inhibitors - members b. Fondaparinux - mechanism c. Rotrecogin alfa - mechanism |
a. -Irudins
I. Hirudin II. Desirudin III. Lepirudin IV. Bivalirudin b. Fondaparinux Bind to antithrombin and cause it to inhibit Xa\Thrombinase. c. Drotecogin alfa Recombinant form of activated protein C which inhibit factor Va and VIIIa (Stringer) |
|
|
Thrombolytic drugs - organization and members
|
First generation
1. Streptokinase 2. Urokinase (Convert all plasminogen to plasmin throughout the plasma) Second-generation 1. tPA - tissue plasminogen activator -plases (recombinant forms of t-PA, different time of onset and duration) 2. Alteplase 3. Anistreplase 4. Lanoteplase 5. Reteplase 6. Tenecteplase (Second-generation selectively activate plasminogen that is bound to fibrin. And is not antigenic as opposed to the first generation since they are foreign proteins. The antigenicity of the first generation can cause an allergic-anaphylactic reaction.) (Fibrinolysis: plasminogen activators activate plasmin from plasminogen. Plasmin catalyze the degradation of fibrin.) (Stringer) |
|
|
Which agents are used to treat intermittent claudication, and what are their mechanism
|
Pentoxifylline and cilostazol.
Phosphodiesterase III inhibitors -> inhibit platelet aggregation and case vasodilation. (Stringer) |
|
|
Lipid-lowering drugs - organization and members
|
HMG-CoA reductase inhibitors - Statins
1. Simvastatin 2. Lovastatin 3. Atorvastatin 4. Fluvastatin Bile-acid binding resins 1. Cholestyramine 2. Colestipol (Anion exchange resins that bind negatively charged bile acids) Drugs increasing lipoprotein lipase activity - -fibrates 1. Bazafibrate 2. Clofibrate 3. Fenofibrate 4. gemfibrozil Others 1. Ezetimibe (inhibit cholesterol absorption) 2. Niacin (Stringer) |
|
|
Lipid-lowering drugs
a. Ezetimibe - mechanism b. Niacin - mechanism |
a. Ezetimibe
Inhibit the absorption of dietary and biliary cholesterol from the small intestine. (Don't affect the absorption of other drugs and fat-soluble vitamins like the bile-binding resins do.) b. Niacin Decreased TG synthesis -> decreased hepatic VLDL secretion -> decreased plasma TG and cholesterol levels (Stringer) |

