![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
75 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
why mycobacterial infections are difficult to treat
|
- slow growing compared to other bacteria
- dormant and resistant to several drugs - lipid rich mycobacterial cell wall is impermeable to many agents - intracellular pathogens and are inaccessible to drugs (macrophages) |
|
|
|
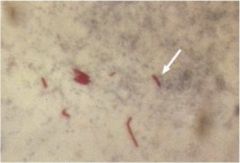
what bacteria is this?
|
|
Mycobacterium tuberculosis; acid-fast stain Ziehl-Neelsen stain
|
|
|
Describe gross morphology
|

|
TB cavity with caseous content. Cavity contains central core with many bacilli lined by caseous material containing fewer bacteria
|
|
|
Drugs used in TB first line
|
- isoniazid
- rifampin - pyrazinamide - ethambutol |
|
|
|
bactericidal first-line anti-tb drugs
|
- isoniazid
- rifampin - pyrazinamide |
|
|
|
first-line anti-tb drugs characteristics
|
- bactericidal (not ethambutol)
- relatively less toxic - effective in combination |
|
|
|
second-line anti-tb drugs
|
- cycloserine
- ethionadmide - kanamycin - capreomycin - para-amino salicylic acid - streptomycin |
|
|
|
second line anti-tb drugs characteristics
|
- more toxic
- less tolerated - reserved for txn of drug resistant tb |
|
|
|
Isoniazid (INH)
mode of action |
- bioactivated by katG (catalase)
- inhibits enzymes for mycolic acid synthesis - resistance associated with deletion in katG gene |
|
|
|
Isoniazid (INH)
pharmacokinetics |
- oral, absorbs well, distributes in all tissues, high intracellular concentrations
- metabolized mainly in liver and excreted in urine |
|
|
|
Izoniazid (INH)
adverse effects |
- hepatitis
- neuropathy - vitamin b6 deficiency |
|
|
|
Izoniazid (INH)
precautions |
- pyridoxine may be given to pts to prevent neuropathy
- inhibits metabolism of phenytoin (potentiates side effects (ataxia) of this drug |
|
|
|
Rifampin (RIF)
mode of action |
- blocks transcription
- inhibits bacterial DNA- dependent RNA polymerase by binding to beta subunit and inhibit RNA synthesis - bactericidal |
|
|
|
Rifampin (RIF)
pharmacology |
- orally well absorbed
- well distributed in tissues - metabolized in liver - excreted in feces and in urine (tears and urine rosy) |
|
|
|
Rifampin (RIF)
adverse effects |
- skin eruptions
- hepatitis - increases elimination of other drugs such as contraceptive steroids - urine has reddish color |
|
|
|
Rifampin (RIF)
precautions |
- watch for levels of other drugs
- HIV infected individuals should be given Rifabutin (does not increase metabolism of protease |
|
|
|
Rifampin induces:
|
:cytochrome P450
|
|
|
|
Drugs affected by Rifampin
|
- oral contraceptives
- protease inhibitors |
|
|
|
Pyrazinamide (PZA)
mode of action |
- converted to pyrazinoic acid (pncA)
- resistance may be due to mutations in pncA that impairs conversion of pyrazianamide to active form - active at pH of 5.5 affects mycobacteria residing in acidic envt of lysosomes - bactericidal |
|
|
|
Pyrazinamide (PZA)
pharmokinetics |
- absorbed orally
- well distributed in tissues - concentrates inside the cells - metabolized in liver - excreted in urine |
|
|
|
Pyrazinamide (PZA)
adverse effects |
- hepatitis
- hyperuricemia and gout - arthralgia, fever, rash |
|
|
|
Pyrazinamide (PZA)
precautions |
- monitor serum glutamic oxaloacetic transaminase (SGOT) and uric acid levels
|
|
|
|
Ethambutol
mode of action |
- inhibits arabinosyl transferase involved in bacterial cell wall synthesis
- bacteriostatic |
|
|
|
Ethambutol
pharmokinetics |
- well absorbed orally
- well distributed in most tissues - tuberculous meningitis txn - excreted mostly unchanged in urine |
|
|
|
txn for tuberculous meningitis
|
ethambutol
|
|
|
|
Ethambutol
adverse effects |
- OPTIC NEURITIS resulting in red-green blindness
- peripheral neuritis |
|
|
|
Ethambutol
precautions |
- monthly tests for visual acuity
|
|
|
|
second line therapy used in case of:
|
- resistance to first-line agents
- failure of clinical response to conventional therapy - seriously txn-limiting adverse drug rxns |
|
|
|
Streptomycin (SM)
mode of action |
- inhibits bacterial protein synthesis
- interferes w/ initiation complex of peptide formation - causes misreading of mRNA |
|
|
|
Streptomycin (SM)
pharmokinetics |
- given IV or IM
- distributed in most of the tissues - very low intracellular concentrations effective against extracellular bacilli - excreted unchanged |
|
|
|
Streptomycin (SM)
adverse effedcts |
- ototoxicity
- vestibulr dysfunction (pts fall in dark room), irreversible |
|
|
|
Streptomycin (SM)
precautions |
routine audiometry
|
|
|
|
Ethambutol
adverse effects |
optic neuritis with blurred vision, red-green color blindness
|
|
|
|
Ethambutol
watch for |
establish baseline visual acuity and color vision, test monthly
|
|
|
|
Isoniazid
adverse effects |
- hepatic enzyme elevation
- hepatitis - peripheral neuropathy |
|
|
|
Isoniazid
watch for |
take baseline hepatic enzyme measurements; significant interaction with phenytoin and antifungal agents
|
|
|
|
Pyrazinamide
adverse effects |
- hepatitis
- nausea - hyperuricemia - rash - joint ache - gout |
|
|
|
Pyrazinamide
watch for |
take baseline hepatic enzymes and uric acid measurement
|
|
|
|
Rifampin
adverse effects |
- hepatitis
- flu-like syndrome - significant interaction with several drugs |
|
|
|
Rifampin
watch for |
take baseline hepatic enzyme measurements and CBC count; warn pt urine and tears may turn red-orange in color
|
|
|
|
Streptomycin
adverse effects |
- ototoxicity
- nephrotoxicity |
|
|
|
Streptomycin
watch for |
baseline audiography and renal fxn tests
|
|
|
|
Paramino salicylic acid (PAS)
mode of action |
- competes with PABA for mycobacterial dihydropteroate synthetase
- bacteriostatic |
|
|
|
Paramino salicylic acid (PAS)
pharmokinetics |
- readily absorbed orally, give w/ food
- metabolized in liver - excreted in urine |
|
|
|
Paramino salicylic acid (PAS)
adverse effects |
- nausea
- ab pain - diarrhea - hypersensitivity - hepatitis |
|
|
|
Paramino salicylic acid (PAS)
precautions |
- GI symptoms common but give with food
|
|
|
|
Ethionamide
mode of action |
- related to INH
- blocks synthesis of mycolic acids |
|
|
|
Ethionamide
pharmokinetics |
- well absorbed orally
- widely distributed in body - metabolized in liver to ethionamide sulphoxide - excreted in urine |
|
|
|
Ethionamide
adverse effects |
- nausea
- diarrhea - gastic irritation - hepatotoxicity - neurological symptoms |
|
|
|
can lessen neurological side effects of ethionamide
|
Pyridoxine
|
|
|
|
Clofazimine
mode of action |
- inhibits bacterial DNA synthesis
|
|
|
|
Clofazimine
pharmacology |
- absorbed fairly by oral route
- distributed widely - concentrates in reticuloendothelial system and slowly released from deposits - metabolized into several inactive metabolites - excreted mainly in feces |
|
|
|
Clofazimine
adverse effects |
- GI disturbances
- Red-brown skin color - discoloration of skin, urine, and feces |
|
|
|
Cycloserine
acts by: |
- inhibiting cell wall synthesis
(rarely used - poor efficacy and adverse effects) |
|
|
|
Fluoroquinolones
act by: |
- inhibiting topoisomerase II
|
|
|
|
Fluoroquinolones
list |
- cirpofloxacin
- moxifloxacin - levofloxacin |
|
|
|
most active drug against M tuberculosis and is useful for drug resistant TB
|
moxifloxacin (a fluoroquinolones)
|
|
|
|
Standard txn regiments for pulmonary tuberculosis
|
- initial phase (2 mnths daily)
- INH, RIF, PZA or - INH, RIF, PZA, EMB - sterilizing phase (4 mnths daily or 3x/wk) - INH, RIF |
|
|
|
Preventive chemotherapy for tb
|
- individuals w/ + tuberculin test
- contacts of infectious cases of tb - INH monotherapy for 6 mnths |
|
|
|
Leprosy (hansen's disease) caused by:
|
Mycobacterium leprae (hansen's bacillus)
|
|
|
|
Mycobacterium leprae
characteristics |
- gram-positive
- rod shaped - surrounded by waxy coating - stains with carbol-fuchsin |
|
|
|
why M leprae will not grow in artificial culture conditions
|
it is an obligate intracellular parasite that lacks many necessary genes for independent survival
|
|
|
|
Tuberculoid (paucibacillary)
|
form of leprosy characterized by one or more hypopigmented skin macules and anaesthetic patches
|
|
|
|
Common features of tuberculoid leprosy
|
- skin sensations lost due to damaged peripheral nerves
- thickening of auricular nerve on neck of pts |
|
|
|
Lepromatous (multibacillary)
|
form of leprosy associated w/ symmetric skin lesions, nodules, plaques, thickened dermis, frequent involvement of nasal mucosa resulting in nasal congestion, gynaecomastia; detectable nerve damage is late
|
|
|
|
leonine faces
|
sign of lepromatous leprosy; loss of eyebrows and partial collapse of nose with heavy bacterial load
|
|
|
|
types of leprosy
|
- tuberculoid (paucibacilary)
- lepromatous (multibacillary) |
|
|
|
Treatment for leprosy
|
- Dapson (diamino diphenyl sulfone)
- recommended for MB: rifampin, clofazamine, dapsone - recommended for PB: rifampin, dapsone |
|
|
|
Type of therapy treatment for leprosy
|
multidrug therapy
(monotherapy is considered unethical) |
|
|
|
Dapson
mode of action |
- inhibits folate synthesis
|
|
|
|
Dapson
pharmacokinetics |
- oral well absorbed from gut
- excreted into bile - reabsorbed from intestine - excreted into urine |
|
|
|
Dapson
adverse side effects |
- well-tolerated
- fever - gastrointestinal intolerance - skin rash - exfoliative dermatitis |
|
|
|
Dapsone should not be given to:
|
:pts allergic to any of sulpha drugs
|
|
|
|
atypical mycobacteria seen in late stages of AIDS
|
Mycobacterium avium
(nontuberculous, noncommunicable) |
|
|
|
Mycobacterium avium
treatment |
- azithromycin
- ethambutol - rifabutin - moxifloxacin (a fluoroquinolones) |
|

