![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
47 Cards in this Set
- Front
- Back
|
What the Body does to a Drug |
Pharmacokinetics |
|
|
What a Drug does to the Body |
Pharmacodynamics |
|
|
Pharmacokinetics |
The study of Absorption,Distribution, Metabolism, and Excretion |
|
|
Bioavailability |
Fraction of unchanged drug that reaches the systemic circulation |
|
|
Disadvantages of Transdermal Medication Administration |
Must be lipid and Water soluble MW<1000 Dose<10mg per day pH 7-9 |
|
|
Factors affecting Absorbtion (Site) |
Blood Flow to the site pH of the tissue Surface area exposed to the Blood Flow |
|
|
Order of absorption for Local tissues I Think I Can Please Everyone But Susie and Sally |
IV Tracheal Intercostal Caudal Paracervical Epidural Brachial Plexus Sciatic/Subarachnoid Subcutaneous |
|
|
Factors Affecting Absorption (the Drug) |
Lipid or Water Soluble pKa Concentration Gradient of the Drug Protein Binding |
|
|
Distribution of Drugs |
The process of a drug permeating throughout the body's tissues after systemic absorption |
|
|
Total percent of body weight in water |
Men 60% Women and Elderly 50% Infants 70% |
|
|
Total % Body Weight in: Extracellular Fluid (ECF) Intracellular Fluid (ICF) |
ECF 20% (Plasma 5% + Intestitial Fluid 15%) ICF 40% |
|
|
Type of drugs that can be considered Single Compartment Theory |
Water Soluble drugs: administered IV nearly instantly evenly distributed throughout the body |
|
|
Two Compartment Model |
Central Compartment (Heart, Lungs, Liver, Brain, Kidneys which are Vessel Rich Organs)75% of CO Peripheral Compartment (Intestines, Bones, Skin which are less vessel rich Organs) 25% of CO |
|
|
Volume of Distribution |
Amount of Drug in the body related to the concentration of drug in the blood or Plasma Vd=Q(quantity of drug)/Cpt(Plasma Concentration at Time zero) |
|
|
Permeation |
the Movement of drug molecules within the body's environment |
|
|
Mechanisms of Permeation |
Aqueous Diffusion Lipid Diffusion Special Carriers (Active Transport/Facillitated Diffusion) Endocytosis (Phagocytosis (solids), Pinocytosis (liquids)) |
|
|
Factors Affecting Tissue Uptake |
Organ Perfusion Protein Binding Lipid Solubility |
|
|
Proteins Drugs Bind to |
Albumin (most Acidic Drugs) Alpha 1 Acidhlycoprotein (Basic Drugs) Lipoproteins |
|
|
What Protein to Most Local Anesthetics Bind to |
Alpha 1-Acid Glycoprotein |
|
|
How is Vd related to Protein Binding |
Inversely proportional as Protein Bound meds do not cross the cell membrane |
|
|
Is protein bound or unbound medication able to be metabolized and excreted through glomerular filtration |
Unbound medication |
|
|
Are lipid soluble medication polarized(ionized) or nonpolarized(nonionized) |
Nonpolarized |
|
|
What does the Dissasociation Constant pKa correspond to |
The pH at which 50% of the drug is ionized and 50% is non-ionized |
|
|
End products of Biotransformation (Metabolism) are: |
Inactive Water soluble to be excreted at the Kidneys |
|
|
Other sites of Biotransformation besides the Liver |
Plasma Lungs Kidneys GI Tract Placenta |
|
|
Two types of reactions in Biotransformation |
Phase I Reactions or Phase II Reactions |
|
|
Phase I Reactions (OIL RIG) |
Oxidation-Loss of an electron Reduction-Addition of electron catalyzed by cytochrome P-450 Hydrolysis-Breaking into 2 parts (doesn't always happen in the liver) |
|
|
Phase II Reactions (How does it work) |
Conjugation-couples a drug or Phase I metabolyte with an endogenous substrate (carbohydrate, amino acid) to form a highly polar/ionized or water soluble end product |
|
|
Types of Phase II Reactions |
Glucuronidation-Midazolam, Propofol, Morphine Glutathione Conjugation Sulfation Acetylation |
|
|
Other Biotransformation through Hepatic Microsomal Enzymes |
Mainly in Hepatic Smooth Endoplasmic Reticulum, also kidneys, GI tract, adrenal cortex Enzymes Cyto P-450 Acetyl Co-enzyme A Trensferases(Methyl, Sulfo, N-acetyl,UDP-gluuronpsyl) |
|
|
Inducers of CP450 3A4 |
Phenobarbital Carbamazepine Rifampin St. John's Wart Phenytoin |
|
|
Inhibitors of CP450 3A4
|
Ketoconazole Fluconazole Cimetidine Antibiotics (not azithromycin) Grapefruit Juice Chronic Alcohol ingestion |
|
|
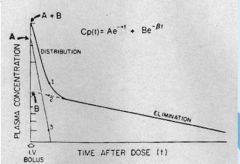
Phases of Elimination |
Alpha-Distribution phase the redistribution of drug from vessel rich group to the peripheral tissues Beta-Elimination phase after redistribution slows continuous elimination from the central compartment |
|
|
nothing |
|
|
Elimination Half-Life |
When 95% of the drug is eliminated 5 half-lifes needed to reach 96% eliminated 6 Half-lifes needed to reach 98% eliminated |
|
|
Context Sensitive Half-Time |
Time necessary for plasma concentrations to reach 50% after discontinuing an IV infusion |
|
|
Zero Order Kinetics |
Plasma Concentration exceeds capacity of metabolizing enzymes Constant rate metabolism, decreasing Half-time Alcohol, Aspirin, Phenytoin |
|
|
First Order Kinetics |
Constant fraction of available drug metabolized Half-Life is Constant Most drugs use this pathway |
|
|
Clearance |
the volume of plasma cleared of a drug by excretion or metabolism by unit of time proportional to dose and inversely related to half-life C=Q(blood flow)xE(extraction ratio) |
|
|
Hepatic Clearance |
Perfusion dependent elimination High hepatic extraction ratio>0.7 Blood flow dependent, min hepatic enzymes Capacity dependent elimination Low hepatic extraction ratio<0.3 Not blood flow dependent |
|
|
Drugs with Low Hepatic Extraction Ratios |
Diazepam Lorazepam * Methadone Phenytoin Rocuronium * Theophylline Theopental |
|
|
Drugs with Intermediate Hepatic Extraction Ratios |
Alfentanil Methohexital Midazolam Vecuronium |
|
|
Drugs with High Hepatic Extraction Ratios |
Bupivacaine Diltiazem Fentanyl * Ketamine * Lidocaine Meperidine Metoprolol Morphine Naloxone Nifedipine Propofol * Propranolol Sufentanil |
|
|
Renal Clearance Formula |
CrCl(ml/min)=140-age(years)xbody weight(kg) --------------------------------------------- 0.815xserum creatinine(micromol/L) |
|
|
Renal Clearance involves |
Glomerular Filtration (reduce by protein bound) Active tubular secretion (active transport) Passive Tubular Reabsorbtion (pH and renal tubular flow) |
|
|
Excretion |
Kidneys primary source Non-protein bound drugs freely pass No ionized fraction of drug reabsorbed Altering Urine pH can change renal excretion(inverse) |
|
|
Drugs with significant renal excretion |
Aminoglycosides * Atenolol Cephalosporins * Digoxin Edrophonium Nadolol Neostigmine * Nor-Meperidine Pancuronium Penicillan Pyridostigmine Rocuronium* |

