![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
81 Cards in this Set
- Front
- Back
|
Describe Acute Toxicity
|
1-2 days with a single or multiple exposures
|
|
|
Describe Subacute Toxicity
|
repeated exposure of less than 3 months
|
|
|
Describe Chronic Toxicity
|
repeated exposure of greater than 3 months
|
|
|
What is the Therapeutic Index?
|
LD50/ED50
|
|
|
What is the Margin of Safety?
|
LD1/ED99
|
|
|
Define "Risk"
|
the probability that injury will result from exposure to a substance under SPECIFIED CONDITIONS of DOSE & ROUTE of administration
|
|
|
Define "Threshold Limit Values"
|
Safe ambient air concentrations in the work place
|
|
|
Drugs whose toxic mechanism of thru Receptor-ligand interactions
|
Nicotine
Most drugs |
|
|
Drugs whose toxic mechanism of thru membrane function (2)
|
General anesthetics
Hydrocarbons |
|
|
Drugs whose toxic mechanism is via cellular energy
|
Cyanide
Pentachlorophenol |
|
|
Drugs whose general mechanism of toxicity is via Covalent binding to biomolecules
|
Organophosphates
Alkylating agents Reactive intermediates |
|
|
Drugs whose general mechanism of toxicity is via Calcium Homeostasis
|
Oxalates
|
|
|
Drugs whose general mechanism of toxicity is via non-lethal alterations in somatic cells
|
Aflatoxin
|
|
|
Drugs whose general mechanism of toxicity is via Ligand-activated transcription factors
|
Dioxins
Glucocorticoids |
|
|
Drugs whose general mechanism of toxicity is via Programmed cell death (apoptosis)
|
Acetaminophen
Etoposide |
|
|
List the 4 primary determinants of toxicity
|
1. dose & dose rate
2. duration of exposure 3. route of exposure 4. CONCENTRATION X TIME = MOST IMPORTANT |
|
|
List the "ABCD's" in the management of a poisoned patient
|
Airway = should be cleared of vomitus or any other obstruction & an airway or endotracheal tube inserted
Breathing = assessed by observation & by measurements of arterial gases = pulse-oximetry; intubate & mechanically ventilage if needed Circulation -monitor pulse rate, blood pressure, & urinary output -start IV & draw blood for glucose & other laboratory determinants Dextrose -every patient with altered mental status -100 mg of Thiamine to alcoholic & malnourished patients to prevent Wernicke-Korsakoff syndrome |
|
|
What group of people are most frequently poisoned?
|
Children
|
|
|
What drugs cause CNS depression as their route of death to the patient?
|
Narcotics
Barbiturates Alcohol *lose airway protective reflexex & respiratory drive *likely to die as a result of airway obstruction, aspiration, or respiratory arrest |
|
|
What drugs can cause Hypotension as their mode of mortality?
|
1. TCA's = alpha blockade
2. Phenothiazines (Chlorpromazine) = alpha blockade 3. Beta-blockers 4. CCA's 5. Theophylline = increases cAMP 6. Barbiturates |
|
|
What drugs can cause Cardiac Arrhythmias as their mode of mortality? (5)
|
1. Amphetamines = releases stored catecholamines
2. Cocaine = uptake inhibitor 3. TCA's = anticholinergic effects = tachycardia 4. Digitalis 5. Theophylline |
|
|
What drugs may cause Cellular Hypoxia and result in death?
|
1. Cyanide
2. Hydrogen Sulfide 3. Carbon Monoxide *evident by: tachycardia, hypotension, acidosis, & cardiac ischemia |
|
|
What drugs may cause a combination of HYPERTENSION & TACHYCARDIA as vital signs?
|
1. Amphetamines = releases of Catecholamines
2. Cocaine 3. Antimuscarinics -Atropine -Scopolamine -Ipratropium -Tolterodine |
|
|
What drugs may cause a combination of HYPOTENSION & BRADYCARDIA as vital signs?
|
1. Beta blockers
2. CCA's 3. Clonidine 4. Sedative-hypnotics |
|
|
What drugs may cause a combination of HYPOTENSION & TACHYCARDIA? (4)
|
1. TCA's
2. Phenothiazines (Chlorpromazine) 3. Theophylline (Acute) 4. Beta-agonists = Beta-1 on heart; Beta-2 on venous smooth muscle |
|
|
What drugs may cause rapid respiration as a vital sign?
|
1. Salicylates
2. Carbon Monoxide 3. Chemical producing Metabolic Acidosis or Cellular Asphyxia |
|
|
What drugs can cause Hyperthermia?
|
1. Sympathomimetics
2. Anticholinergics = atropine 3. Salicylates 4. Pentachlorophenol = uncoupler of oxidative phosphorylation 5. chemicals producing seizures or muscular rigidity |
|
|
What drugs can cause Hypothermia or Poikilothermy? (2)
|
1. Phenothiazines (Typical Antipsychotics)
2. Ethanol & other sedatives |
|
|
What drugs can cause Pupil constriction (miosis)? (4)
|
1. Opioids
2. Phenothiazines (alpha-blockade) 3. Cholinesterase inhbitors 4. Alpha-blockers *Miosis is caused by Parasympathetic activation or Sympathetic inactivation |
|
|
What drugs can cause Pupil Dilation (Mydriasis)?
|
1. Amphetamines
2. Cocaine 3. LSD 4. Anticholinergics 5. Phencyclidine *Mydriasis = caused by sympathetic activation or parasympathetic blockade |
|
|
What drugs can cause HORIZONTAL NYSTAGMUS?
|
Sedative-hyptonics
1. PHENYTOIN 2. Alcohol 3. Barbiturates |
|
|
What drug do Vertical & Horizontal nystagmus strongly suggest?
|
Phenyclidine (PCP)
|
|
|
What drugs can cause Flushed, hot & dry skin?
|
Atropine
Antimuscarinics |
|
|
What drugs can cause Excessive sweating?
|
1. Cholinesterase inhibitors
2. Sympathomimetics 3. Nicotine |
|
|
What drugs can cause Cyanosis?
|
1. Hypoxemia
2. Methemglobinemia |
|
|
What drugs can cause Jaundice (liver toxicity)?
|
1. Acetaminophen
2. Erythromycin estolate (cholestatic) 3. Carbon Tetrachloride |
|
|
What drugs can cause Ileus? (3)
|
1. Antimuscarinics
2. Opioids 3. Sedatives |
|
|
What drugs can cause Hyperactive bowel sounds, cramping, & diarrhea?
|
1. Organophosphates
2. Iron 3. Arsenic 4. Theophylline 5. Mushrooms |
|
|
What drugs can cause twitching & muscular hyperactivity? (3)
|
1. Anticholinergics
2. Sympathomimetics 3. Cocaine |
|
|
What drugs can cause Muscular Rigidity? (2)
|
1. Antipsychotics (esp. Haloperidol)
2. Strychnine |
|
|
What drugs can cause Seizures? (7)
What do you usually treat with? |
Tx = Diazepam or Lorazepam
1. Theophylline 2. Isoniazid (treat with Pyridoxine = B6) 3. Cocaine 4. Amphetamines 5. TCA's 6. Diphenhydramine 7. Lidocaine (treat with Thiopental) |
|
|
How do you treat seizures caused by Isoniazid? Lidocaine?
|
Isoniazid = Pyridoxine (B6)
Lidocaine = Thiopental |
|
|
What drugs can cause Flaccid coma?
|
1. Opioids
2. Sedative-hypnotics 3. CNS depressants |
|
|
pO2 may appear normal in this poisoning b/c Arterial blood gases only measures dissolved oxygen & not oxyhemoglobin saturation
|
Carbon Monoxide
|
|
|
How do you calculate the Anion Gap? What is the normal range?
|
Anion Gap = (Na + K) - (HCO3 + Cl)
Normal = 12 +/- 4 |
|
|
What conditions can cause an elevated Anion Gap?
|
1. Renal failure
2. Diabetic Ketoacidosis 3. Shock-induced lactic acidosis 4. Drug-induced Metabolic Acidosis -Salicylates -Methanol -> formic acid -Ethylene glycol -> Oxalic acid -Isoniazid -Iron -Metformin -> lactic acidosis |
|
|
What 2 drugs cause both an Anion Gap & Osmolar Gap?
|
1. Methanol
2. Ethylene glycol |
|
|
What drugs cause an Osmolar Gap?
|
1. Ethanol
2. Methanol (also Anion gap) 3. Ethylene glycol (also Anion gap) |
|
|
How does one calculate the Osmolar Gap?
|
Calc. OG = 2(Na+) + (Glucose/18) + (BUN/2.8)
Osmolar Gap = Measured - Calculated |
|
|
Widening of the QRS complex
TCA's = Amytriptyline Antidote = IV Sodium Bicarbonate |
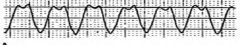
What is seen here? What drugs can cause this? What is the Antidote?
|
|
|
Torsades de Pointes
Caused by: 1. Quinidine 2. TCA's 3. Phenothiazines 4. "Non-sedating" Antihistamines -Astemizole -Terfenadine 5. Cisapride = 5-HT4 agonist used for GERD Prolonged QT caused by: 1. Beta-1 stimulationm (Epi, NE, Isoproterenol, Dobutamine, etc) 2. Intense sympathetic activation |
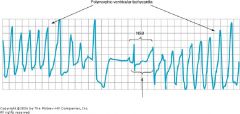
What is seen here?
What drugs can cause it? (5) |
|
|
What are 5 factors that can contribute to Torsades de Pointes?
|
1. Hypokalemia
2. Hypomagnesemia 3. Hypocalcemia 4. Ischemia 5. Tissue hypoxia **low everything |
|
|
What is the treatment for Torsades de Pointes?
|
Magnesium Sulfate
|
|
|
When is Gastric Lavage not recommended?
|
after 30 minutes to 4 hours
|
|
|
What are the Contraindications for Gastric Lavage & Induced Emesis?
|
1. More than 30 minutes have elapsed since ingestion of a CORROSIVE material
2. Hydrocarbon solvents have been ingested (ethanol, methanol) 3. Coma, stupor, delerium, or convulsions |
|
|
What is sometimes used to induce emesis?
|
Ipecac syrup
*often not recommended today |
|
|
This substance will absorb many toxins if given in slurry immediately before or after lavage
|
Activated Charcoal
|
|
|
What drugs are used as cathartics (laxatives) to enhance elimination of toxic drugs?
|
1. MgSO4
2. Sorbitol |
|
|
What drugs are given to get rid of Weak Acids in the urine?
|
Bases = HA -> A-
1. NaHCO3 = Sodium Bicarb 2. Acetazolamide |
|
|
This is used to Acidify the urine and increase the excretion of Weak Organis Bases
|
Ammonium Chloride
|
|
|
What is the rule of thumb in Hemodialysis & trying to remove a toxic drug?
|
the smaller the Vd = the more effective is Hemodialysis
|
|
|
Osmotic diuretic used to enhance the elimination of toxic drugs
|
Mannitol
|
|
|
Drug used as a chelator for Iron Poisoning
|
Deferoxamine mesylate
|
|
|
Drug used for Arsenic, gold, mercury, & acute lead poisoning
|
Dimercaprol
|
|
|
Metal chelator used for Lead poisoning
|
Edetate, Calcium Disodium = CaNa2(EDTA)
|
|
|
Chelating agent used for Wilson's disease (copper), cystinuria, & resistant cases of Rheumatoid Arthritis
Chelates copper; also used for lead |
Penicillamine
|
|
|
Oral chelator used for lead
|
Succimer
|
|
|
Drug that inactivates toxins & is used in Acetaminophen poisoning
|
N-acetylcysteine
|
|
|
Inactivating-toxin drug that is used for Cardiac Glycoside toxicity
|
Digoxin-specific FAB antibodies
|
|
|
Antidote to Cholinesterase Inhibitor poisons
-Neostigmine -Pyridostigmine -Physostigmine -Echothiophate |
Atropine = antimuscarinic
|
|
|
Cholinesterase reactivator given only for Organophosphates
|
Pralidoxime chloride = 2-PAM
|
|
|
Antidote for Benzodiazepine overdoses
|
Flumazenil
|
|
|
Opioid antidote
|
Naloxone
|
|
|
Cyanide antidote package = ?
|
Sodium nitrite
Sodium Thiosulfate Amyl Nitrite |
|
|
Antidote for Beta-blocker poisoning
|
Glucagon
|
|
|
Antidote for Methanol or Ethylene glycol poisoning
|
Ethanol
|
|
|
Alcohol Dehydrogenase inhibitor used for treatment of Methanol & Ethylene glycol poisoning
|
Fomepizole
|
|
|
Antidote for poisoning with Cardiac Depressants:
-TCA's -Quinidine |
Sodium Bicarbonate
|
|
|
Antidote for chemical-induced convulsions
|
Diazepam or Lorazepam
|
|
|
Antidote for Isoniazid poisoning
|
Pyridoxine
|
|
|
Antidote for Anticholinergic poisoning
|
Physostigmine
|

