![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
97 Cards in this Set
- Front
- Back
|
Kidneys filter __1__L of plasma daily to form __2__ L of urine
|
1. 180
2. 1.5 |
|
|
What does the Nephron consist of?
|
1. Glomerulus = filtering aparatus; filtration is nonselective
2. Long tubular portion = reabsorbs and conditions glomerular filtrate |
|
|
What are the 3 basic renal functions?
|
1. Filtration
2. Reabsorption 3. Secretion |
|
|
Urine composition is determined mainly by __1__ and modified by __2__
|
1. Reabsorption
2. Secretion |
|
|
What are the 3 main goals of Renal Function?
|
1. Reabsorb substances that the body needs
2. maintain acid-base balance 3. Excrete waste and foreign products that have to be eliminated |
|
|
Glomerulus:
-all __1__ plasma molecules are filtered while __2__ and __3__ remain in the blood -the most prominent filtered constituents are __4__ & __5__ with smaller amounts of __6__ & __7__ |
1. small = electrolytes, aa's, drugs, glucose, metabolic wastes
2. large = lipids, proteins 3. cells 4. Sodium 5. Chloride 6. Bicarbonate 7. Potassium |
|
|
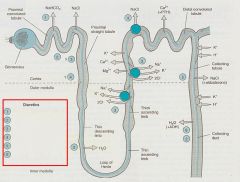
What does the Proximal Convoluted Tubule absorb? (5)
|
1. NaCl
2. NaHCO3 3. Glucose 4. Amino Acids 5. Organic solutes *water is reabsorbed passively to keep osmolarity constant |
|
|
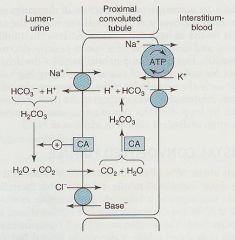
Reabsorption of NaHCO3 in the Proximal Convoluted Tubule depends on what?
|
Carbonic Anhydrase activity
|
|
|
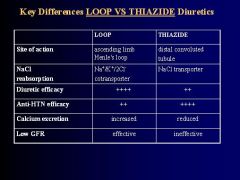
Tubular segment between the Proximal and distal convolutions that actively reabsorbs 35% of NaCl but is impermeable to water so that the tubular fluid becomes diluted
|
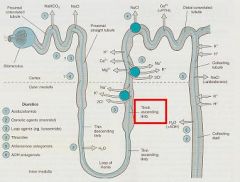
thick ascending Loop of Henle
|
|
|
What transport system is contained within the luminal membrane of the Thick Ascending limb of the Loop of Henle?
|
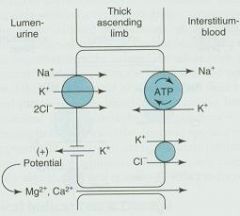
Na+/K+/2Cl-
|
|
|
Specialized cells in the thick ascending limb of the Loop of Henle that act as chemoreceptors to influence Renin secretion by sensing NaCl influx as tubular fluid leaves the loop
|
Macula Densa
|
|
|
Tubule segment between the Loop and Collecting Tubule that contains the NaCl transporter which reabsorbs 10% of filtered NaCl
|

Distal Convoluted Tubule
|
|
|
Part of Nephron that has Principle and Intercalated cells with ion channels for Na+ and K+
-Na+ is reabsorbed in exchange for secreting K+ |

Collecting Tubule
|
|
|
Nephron part that determines the final Na+ concentration in the urine
|
Collecting tubule
|
|
|
The coupling of Na+ reabsorption to K+ secretion in the Collecting Tubule is regulated by what?
|
Aldosterone
*high Aldosterone = high Na+ reabsorption / high K+ secretion |
|
|
What happens to the concentration of NaCl in the lumen of tubules as you get further away from the Glomerulus?
|
NaCl will decrease
**important b/c it affects the action of diuretic drugs |
|
|
Differentiate between 'diuresis' and 'natriuresis"
|
Diuresis = increase in urine volume
Natriuresis = increase in renal sodium excretion -> causes diuresis |
|
|
Diuretic drugs increase urine __1__ or __2__ by blocking the __3__ functions of the renal tubules
|
1. volume
2. flow 3. transport |
|
|
Explain how diuretic drugs exert their action
|
Block sodium and choloride reabsorption
-increase intratubular osmotic pressure ➡ prevents passive reabsorption of water ➡ increases urine flow |
|
|
Which diuretics will have a greater effect, early acting or late acting ones? Why?
|
Early acting b/c they will block Na+ reabsorption the most (b/c that is where the most Na+ reabsorption occurs)
|
|
|
What clinical conditions are Diuretic drugs used for?
|
1. HYPERTENSION
2. acute and chronic HEART FAILURE 3. acute and chronic renal failure 4. Nephrotic syndrome 5. Cirrhosis |
|
|
List the 5 clases of Diuretics
|
1. Carbonic Anhydrase inhibitors = Acetazoleamide
2. Osmotic agents 3. Loop diuretics 4. Thiazides 5. Potassium sparing |
|
|
List the 2 groups of Carbonic Anhydrase inhibitors and their respective drugs
|
1. Oral Preparation
-Acet-azol-amide -Di-chlor-phenamide -Meth-azol-amide 2. Ophthalmic preparations -Brin-zolamide -Dor-zolamide |
|
|
Carbonic Anhydrase is located in the luminal membranes of the __1__ cells where it catalyzes dehydration of __2__ for __3__ reabsorption
|

1. Proximal tubule
2. Carbonic acid (H2CO3) 3. NaHCO3 |
|
|
How do Carbonic Inhibitors produce diuresis?
|
by blocking the reabsorption of NaHCO3
|
|
|
Why does the diuretic effectiveness of Carbonic Inhibitors diminish after several days?
|
Bicarbonate depletion eventually enhances NaCl reabsorption
|
|
|
Prototype CA inhibitor used rarely as a diuretic nowadays, but is used instead to inhibit CA at sites other than the kidneys
|
Acet-azol-amide
|
|
|
CA inhibitors given orally to treat Glacoma
CA inhibitors applied topically for Glaucoma to avoid metabolic effects or Diuresis |
Acet-azol-amide
Meth-azol-amide Di-chlor-phenamide Brinzol-amide Dorzol-amide |
|
|
Explain how CA inhibitors help in treating Glaucoma
|
CA in the ciliary body normally catalyzes HCO3 secretion into the Aqueous Humor, CA inhibition reduces intraocular pressure by decreasing Aqueous Humor formation
|
|
|
Other than Glaucoma, list 5 other things CA inhibitors are used for
|
1. Urinary Alkalinization
2. Correction of Metabolic Alkalosis 3. preventtion of acute mountain sickness 4. adjuvant epilepsy treatment 5. increase phosphate excretion during |
|
|
Explain the mechanism of Carbonic Anhydrase
Explain Acetazolamide's action |
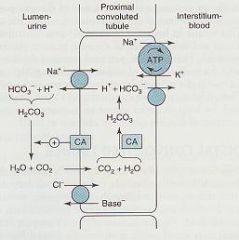
1. counter-current across the apical membrane moves Na+ into the cell & H+ into lumen
2. In the lumen, H+ reacts with HCO3- to produce Carbonic Acid (H2CO3) 3. H2CO3 dissociates to form CO2 + H20; this rxn is catalyzed by cytoplasmic CA Acetazolamide = inhibits CA to reduce reabsorption of Na+ & HCO3- |
|
|
List 4 Osmotic Diuretics
|
1. Glycerin
2. Isosorbide 3. Urea 4. MANNITOL |
|
|
What is the mechanism of action of Mannitol?
|
1. freely filtered at glomerulus, undergo limited tubular reabsorption, relatively inert
2. Mannitol 5-25% injected IV in large amounts increases osmolarity of plasma and tubular fluid to produce diuresis by causing water retention in the PROXIMAL TUBULE and DESCENDING LIMB of HENLE |
|
|
What 2 conditions are Osmotic Diuretics used to treat?
|
1. reduce Intracranial pressure in neurologic conditions
2. reduce Intraocular pressure before opthalmic procedures |
|
|
What are the adverse side effects of Osmotic Diuretics
|
1. Severe Dehydration
2. Loss of free water 3. Hypernatremia 4. Headache, nausea, vomiting |
|
|
What are Osmotic Diuretics contraindicated in? Why?
|
pts with Congestive Heart Failure
b/c of rapid expansion of EC fluid volume and hyponatremia occuring before diuresis may produce Pulmonary Edema and complicate CHF |
|
|
List the 4 Loop Diuretics
|
1. Bumet-anide
2. Furo-semide 3. Tor-semide 4. Ethacrynic acid **BuFET |
|
|
Diuretics formerly referred to as 'high-ceiling' b/c they are the most effective diuretics now available
|
Loop Diuretics
|
|
|
All Loop Diuretics are derivatives of __1__, except __2__
|
1. Sulfonamide
2. Ethacrynic acid |
|
|
How can Loop diuretics be administered? Which way produces extremely rapid diuresis?
|
Orally, IV, IM
IV |
|
|
What is the mechanism of action of Loop Diuretics?
|

inhibit Na+/K+/2Cl- cotransporter in the Thick Ascending Limb of Henle = decreased NaCl Reabsorption
|
|
|
List the important effects of Loop Diuretics
|

1. Increased delivery of Na+ to the Late Distal Tubule & Collecting Tubule = enhances K+ & H+ secretion -> HYPOKALEMIA
2. Reduced NaCl reabsorption -> more Na+ stays in the tubular fluid -> reduced NaCl influx across the Macula Densa chemoreceptors -> INCREASED RENIN SECRETION 3. reduced Ca++ reabsorption in the Loop -> increased Ca++ excretion but hypocalcemia rarely occurs b/c Ca++ is actively reabsorbed downstream in Distal tubule 4. Increase in Mg+ excretion -> HYPOMAGNESEMIA 5. Direct vascular effect due to increased Prostaglandin synthesis may INCREASE RENAL BLOOD FLOW |
|
|
1. Block the Na+/K+/2Cl- cotransporter to prevent reabsorption of Na+ and Cl- and thereby increase tubular excretion
2. Also decrease potential difference generated by recycling of K+ which normally drives divalent reabsorption 3. The reduced electrical potential thus increases excretion of Ca2+ and Mg2+ |
Explain the mechanism of Loop Diuretics (List 3 things)
|
|
|
What is the most common use of Loop Diuretics?
|
relief from EDEMA due to CHF, kidney disease, or hepatic necrosis
** = 1st choice for any kind of Edema |
|
|
When would you use Loop Diuretics for Hypertension?
|
only if Thiazides do not work
** = 2nd line choice for HTN |
|
|
How would you use Loop Diuretics to treat Severe Hyperkalemia?
|
Use together with NaCl and Water administration to enhance urinary K+ secretion
|
|
|
Diuretic used to treat Acute Renal Failure = converts oliguric to nonoliguric failure; are effective EVEN WHEN GFR IS LOW
|
Loop Diuretics
|
|
|
What are the side effects of Loop Diuretics?
|
OH DANG
1. Ototoxicity 2. Hypokalemic metabolic alkalosis = from enhanced K+ & H+ secretion / Hypokalemia leading to cardiac arrhythmias 3. Dehydration & Hyponatremia leading to hypotension, circulatory collapse, reduced GFR, thromboembolic events 4. Allergy = due to Sulfa 5. Nephritis (interstitial) 6. Gout & hyperuricemia = due to increased uric acid reabsorption in the Proximal tubule |
|
|
Hypokalemia leading to Cardiac Arrhythmias caused by Loop diuretics is more common when patients are taking what other drug?
|
Digoxin
|
|
|
With what Loop Diuretic are Allergic Rxns less common? Why?
|
Ethacrynic acid
b/c it is not a Sulfonamide derivative |
|
|
With what Loop Diuretic is Ototoxicity more common?
|
Ethacrynic Acid due to inhibition of the Na+/K+/Cl- transport for endolymph production in the cochlea
|
|
|
Loop diuretic that can be used in patients who are either allergic to sulfa drugs or those who have gout
|
Ethacrynic acid
|
|
|
Most Thiazide diuretics end in -thiazide, but the Sulfonamide Thiazides do not. List 4 of them
|
1. Chlor-thalidone
2. Indapa-mide 3. Met-ola-zone 4. Quin-etha-zone |
|
|
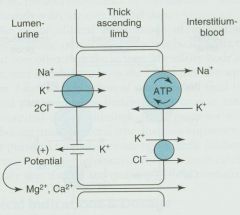
What is the mechanism of action of the Thiazide diuretics?
|

block the NaCl transporter in the Distal Convoluted Tubule = inhibit NaCl reabsorption from lumen
|
|
|
Why are Thiazide diuretics only moderately effective at increasing NaCl excretion?
|
B/c 90% of the filtered load has been reabsorbed before it reaches the distal tubule
|
|
|
What 2 "-emia's" do Thiazide diuretics produce?
|

Hypokalemia = due to increased K+ secretion
Hyperuricemia = due to decreased uric acid secretion |
|
|
What do Thiazide diuretics reduce the excretion of by enhancing the reabsorption in the Distal Convoluted Tubule?
|

Ca++
|
|
|
Diuretic that is INEFFECTIVE when GFR is low
|
Thiazide
**unlike Loop Diuretics |
|
|
Thiazide diuretics
-inhibit NaCl transporter to decrease reabsorption of Na+ and Cl- -reabsorption of Ca++ is enhanced b/c the increased Na+ concentration gradient across the basolateral membrane stimulates the Na+/Ca++ counter-transport |
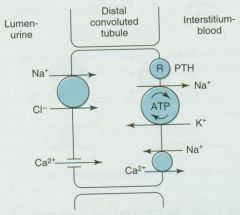
What Diuretic has its action here? Explain what happens
|
|
|
What are Thiazide's the first choice in treatment of?
|
Hypertension
|
|
|
What are Thiazides second in line to Loop Diuretics in treatint?
|
Congestive Heart Failure
|
|
|
Diuretic used to treat Nephrolithiasis due to idiopathic Hypercalciuria = to reduce urinary calcium concentration
|
Thiazides
|
|
|
Diuretic used to treat Nephrogenic Diabetes Insipidus = to reduce polyuria and polydipsia
What is the paradoxical effect due to? |
Thiazides
**the paradoxical effect is due to plasma volume reduction |
|
|
What are the adverse effects of Thiazides
|
hyperGLUC
1. hyperGlycemia = due to decreases in pancreatic releace of insulin and tissue glucose utilization 2. hyperLipidemia 3. hyperUricemia 4. hyperCalcemia --------------------- 5. hypokalemic metabolic alkalosis 6. hyponatremia due to elevated ADH 7. Allergic rxns 8. weakness, fatigability, paresthesias 9. Impotence |
|
|
Diuretic that may induce Hemolytic anemia, thrombocytopenia, and acute necrotizing pancreatitis
|
Thiazides
|
|
|
Diuretic that causes Impotence 4-times more often than Beta-blockers
|
Thiazides
|
|
-
|
-
|
|
|
List the 2 classes of Potassium-sparing Diuretics and the drugs within them
|
Aldosterone antagonists
- Eple-reone - Spirono-lactone Na+ channel blockers - Amilo-ride - Triam-terene **the K+ STAys |
|
|
Diuretics seldomly used alone, but used to counteract Hypokalemia caused by Loop or Thiazide diuretics
|
K+ sparing diuretics
-Spirinolactone -Triamterene -Amiloride -Eplereone |
|
|
What is the mechanism of action of Spironolactone and Eplereone?
|

inhibit K+ secretion by antagonizing the Mineralcorticoid receptors (where Aldosterone binds)
**Aldosterone promotes Na+ reabsorption and K+ secretion in the collecting tubules |
|
|
What is Aldosterone's mechanism of action?
|
Promotes Na+ reabsorption & K+ secretion in the Collecting Tubules = water retention effect
|
|
|
What is the mechanism of action of Triamterene and Amiloride? Why is K+ spared?
|

Block Na+ channels in apical membranes of the Collecting Tubule
b/c its secretion is coupled to Na+ entry |
|
|
1. The inward diffusion of Na+ creates a negative potential in the lumen to drive efflux of K+
2. Amiloride and triamterene block apical Na+ channels to cause loss of potential (decreases the driving force for K+ secretion) and reduce K+ and H+ secretion 3. Aldosterone receptors (MR) decrease Na+ excretion and increase K+ and H+ secretion; opposite effects are produced when blocked by spironolactone or eplerenone |

What Diuretics work here? Explain
|
|
|
What are the clinical uses of the Potassium-sparing diuretics? (3)
|
1. Primary Mineralcorticoid hypersecretion = such as in Conn's Syndrome or Ectopic ACTH production
2. Secondary Aldosteronism = due to CHF, Hepatic Cirrhosis, Nephrotic Syndrome, and other conditions associated with salt retention & reduced fluid volume 3. used together with Thiazide or Loop Diuretics to minimize potassium depletion |
|
|
Diuretic than can be used to reduce Digoxin toxicity during treatment of CHF
|
Spironolactone
|
|
|
List the toxic effects of the Potassium-sparing diuretics
|
1. Hyperkalemia
2. Hyperchloremic metabolic acidosis = due to inhibition of H+ secretion with the reduced K+ secretion 3. Gynecomastia |
|
|
Acute renal failure may occur when this diuretic is combined with Indomethacin
|
Triamterene
|
|
|
Kidney stones may occur with this Potassium-sparing diuretic due to its poor solubility
|
Triam-terene
|
|
|
What are the 2 most common clinical uses of Diuretics?
|
1. reducing fluid volume in Edematous states (CHF, Kidney or Hepatic disease
2. HTN |
|
|
What things increase the risk of Hyperkalemia when using Potassium-sparing diuretics?
|
1. Renal disease
2. drugs that reduce Renin-angiotensin activity - Beta-blockers - ACE inhibitors - Angiotensin antagonists |
|
|
Explain how diuretics help in the treatment of CHF
|
Reduce extracellular fluid volume -> reduce Preload = reduce Cardiac Work
|
|
|
When treating CHF with diuretics, what will concurrent treatment with any Vasodilator cause?
|
Reduced renal blood flow and inhibit the diuretic effectiveness
|
|
|
Diuretic that has reduced the MORTALITY from CHF
|
Spironolactone
**but Loop Diuretics are still 1st line treatment |
|
|
When are Loop diuretics only used for HTN?
|
1. in presence of Renal Insufficiency
2. in presence of Cardiac Failure |
|
|
When are Potassium-sparing diuretics used to treat HTN?
|
only in combination to avoid Hypokalemia
|
|
|
Diuretic of choice for treatment of HTN?
|
Thiazides
|
|
|
In what groups of people are Thiazides more effective than other anti-HTN agents?
|
1. Blacks
2. Elderly |
|
|
1. Acet-azol-amide
2. Osmotic agents 3. Loop agents 4. Thiazides 5. Potassium sparing 6. ADH sparing |
Fill in the diuretics
|
|
|
Carbonic Anhydrase Inhibitors
|
What drug works here?
|
|
|
Diuretics that increase Urine NaCl
|
All of them
|
|
|
Diuretics that increase Urine K+
|
All except K+-sparing
|
|
|
Diuretics that lower the blood pH (acidosis)
|
Carbonic Anhydrase inhibitors
K+-sparing |
|
|
Diuretics that increase the blood pH (Alkalosis)
|
Loop diuretics
Thiazides |
|
|
Diuretics that increase Urine Ca++
|
Loop diuretics
|
|
|
Diuretic that decreases Urine Ca++
|
Thiazide
|
|
|
Why do Loop Diuretics have less of an effect on HTN than Thiazides?
|
Loop Diuretics cause decreased NaCl influx across the Macula Densa chemoreceptors in the Thick Ascending Limb --> Renin secretion --> Angiotensin II formation --> Vasoconstriction & Aldosterone release ( = Na+ reabsorption in Collecting Tubule)
|
|
|
Diuretic whose allergic rxns include cross-reactivity with other Sulfonamides, photosensitivity, and generalized dermatitis
|
Thiazides
|

