![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
78 Cards in this Set
- Front
- Back
|
What are the 2 physiologic features of Asthma?
|
1. increased bronchial and tracheal responses to stimuli
2. widespread narrowing of airway passages |
|
|
What are the pathologic features associated with Asthma?
|
1. Contraction of airway smooth muscles
2. Mucosal thickening from edema and cellular infiltration 3. thickening in the airway lumen of viscid mucus plugs |
|
|
Bronchoconstriction from smooth muscle contraction is most easily reversed by __1__ drugs, while reversal of edema and cellular infiltration requires sustained treatment with __2__ drugs
|
1. Bronchodilator
2. Anti-inflammatory |
|
|
Antiasthmatic drugs classified as "short-term releivers"? "Long-term" controllers?
|
Short-term = Bronchodilators
Long-term = Anti-inflammatory agents |
|
|
Explain the Immunopathogenesis of the Early Rxn of Asthma (occurs within 2 hrs)
|
1. initial allergen exposure
2. production of IgE that bind to mast cells of airway mucosa 3. Re-exposure to allergen cross-links Ag-Ab complexes 4. Mast cell degranulation of Anaphylatoxins 5. Smooth muscle contraction 6. Bronchoconstriction and immediate fall in FEV1 |
|
|
The early reaction of Asthma is mediated by these factors
|
Histamine
Tryptase PGD2 LTC4 PAF |
|
|
Explain the immunopathogenesis of the late reaction of Asthma (occurs 2-8 hrs later)
|
1. release of cytokines, IL's, and various factors from T cell and Mast cells
2. Activate Eosinophils and Neutrophils that release proteins and PAF 3. Edema, mucus hypersecretion, Smooth muscle contractions 4. Bronchoconstriction and increased bronchial reactivity with late fall in FEV1 |
|
|
Describe the Reflex response causing Bronchoconstriction
|

1. Afferent vagal pathway sends signal to CNS upon irritant stimulation
2. Efferent vagal pathway goes to Autonomic ganglia 3. Postganglionic fibers release ACh which binds to Muscarinic receptors on bronchial smooth muscle -> Bronchoconstriction |
|
|
What are the 2 separate ways in which inhaled irritants can cause Bronchoconstriction?
|
1. releasing chemical mediators from Mast cells
2. stimulating Afferent Vagal receptors to initiate reflex bronchoconstriction |
|
|
What 2 things does Bronchospasm in Asthma result from?
|
1. Mediator release
2. Bronchial hyperreactivity |
|
|
Class of antiasthmatic drugs that relax smooth muscles, but will not relieve mucosal edema, cellular infiltration, or mucus formation
|
Bronchodilators
|
|
|
List the 5 B2-adrenergic agonist Bronchodilators
|
Albu-terol
Bitol-terol Pirbu-terol Meta-proter-enol Terbut-aline |
|
|
List the 2 Long-acting B2-adrenergic agonist Bronchodilators
|
Salme-terol
Formo-terol |
|
|
List the 3 Sympathomimetic Bronchodilators
|
Epinephrine
Ephedrine Iso-proter-enol |
|
|
List the 4 Methylxanthine Bronchodilators
|
Amino-phylline
Theo-phylline Dy-phylline Pentoxi-fylline |
|
|
List the 3 Muscarinic Antagonist Bronchodilators
|
Ipra-tropium
Tio-tropium Atropine |
|
|
Class of Antiasthmatic drugs that reduce bronchial responsiveness
|
Anti-inflammatory
|
|
|
List the 6 Glucocorticoids used as anti-inflammatories to treat Asthma
|
Beclo-methasone
Bud-eso-nide Dexa-meth-asone Flu-nisolide Flu-tic-asone Momet-asone |
|
|
List the 2 Leukotriene antagonists used as Anti-inflammatories to treat Asthma
|
Monte-lukast
Zafir-lukast |
|
|
Anti-IgE Antibody used as anti-inflammatory to treat Asthma
|
Omalizumab
|
|
|
What is the mechanism of action of prophylactics used to prevent asthma?
|
prevent Mast cell degranulation
|
|
|
Name the 2 prophylactic anti-asthmatic drugs
|
Cromolyn sodium
Nedo-cromil sodium |
|
|
What is the theoretical goal of the Aerosol delivery of antiasthmatic drugs?
|
-producing high local drug concentration in the lungs
-LOW systemic absorption |
|
|
Aerosol delivery to the lungs with low systemic absorption is especially important for these 2 groups of antiasthmatic drugs
|
B2-adrenergic agonists
Glucocorticoids **have potentially serious side-effects when absorbed systematically |
|
|
Even under ideal conditions, only __1__% of the aerosolized drug is deposited in the lungs and most of the remainder is __2__
|
1. 2-10%
2. Swallowed |
|
|
In order to have minimal systemic effects, Aerosolized drugs should have one of these 2 properties
|
1. poor absorption from GI tract
2. rapidly inactivated by first-pass hepatic metabolism |
|
|
The ratio of inhaled to swallowed drug can be improved by these 2 things
|
1. Large-volume 'spacer'
2. proper technique |
|
|
What is Bronchodilation promoted by?
What 2 things can cause this and how? |
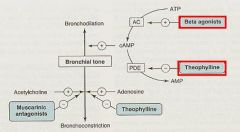
cAMP
1. B2-adrenergic agonists = increase cAMP synthesis by activating Adenylyl Cyclase 2. Phosphodiesterase inhibitors (Theophylline) to slow cAMP degradation |
|
|
What 2 things can inhibit Bronchoconstriction?
|
1. Muscarinic antagonists (Ipratropium)
2. Adenosine antagonists (Theophylline) |
|
|
What are each of the following Methylxanthines found in?
1. Theophylline 2. Theobromine 3. Caffeine |
1. Tea
2. Cocoa 3. Coffee |
|
|
How are aminophylline, dyphylline, pentoxifylline, and theophylline administered?
|
Oral sustained-release or Parenteral preps
|
|
|
The Methylxanthines are declining in use b/c of greater effectiveness of other drugs except one...which one and why?
|
Theophylline b/c it is cheap
|
|
|
What is Theophylline's mechanism of action? (2)
|
1. inhibits Phosphodiesterase that usually degrades cAMP = causes increase intracellular cAMP = Cardiac stimulation and Smooth Muscle relaxation
2. acts partly as Adenosine Antagonist |
|
|
What is the main therapeutic action of Theophylline (Methylxanthine)?
|
Bronchodilation
|
|
|
List the Pharmacodynamics of the Methylxanthines
|
1. CNS stimulation results in alertness and deferred fatigue
-side effects = nervousness, insomnia, tremors, convulsions 2. Positive Inotropic and Chronotropic effects with increased Cardiac Output may produce Arrhythmias and increase BP 3. Stimulate secretion of Gastric Acid and Digestive enzymes 4. are weak Diuretics due to increased GFR and diminished tubular Na+ reabsorption 5. Improve contractility of Skeletal muscle and the diaphragm; improved diaphragmatic fxn will diminish dyspnea **think of Caffeine's effects |
|
|
What is the most effective Methylxanthine bronchodilator?
|
Theophylline
|
|
|
Theophylline relieves airflow obstruction in __1__ and reduces symptom severity in __2__
|
1. acute asthma
2. chronic asthma |
|
|
Sustained-release oral tablets of Theophylline produce therapeutic blood levels for how long?
|
12 hours or more
|
|
|
When should Theophylline only be used? Why?
|
When blood levels can be measured
b/c Therapeutic and Toxic effects are related to plasma levels |
|
|
What may toxic doses of Theophylline cause?
|
Insomnia
Anorexia NVD Heachache Anxiety Arrhythmias Seizures ***Neurotoxicity and Cardiotoxicity |
|
|
Would Theophylline toxicity be increased in Liver or Renal disease? Why?
What 3 drugs increase the toxicity of Theophylline? |
Liver b/c that is what metabolizes it = toxicity may increase in liver disease...beware!!!
Cimetidine, Fluoroquinilone (-floxacin's), & Macrolides (Erythromycin) |
|
|
What is the mechanism of action of the Beta-2-Adrenergic agonists?
|
stimulate Adenylyl Cyclase -> increase cAMP -> Smooth muscle relaxation and bronchodilation
|
|
|
What is the drug of choice for Acute Asthmatic attacks?
|
β2-adrenergic agonists
-Albuterol -Terbutaline -Metaproterenol -Pirbuterol -Bitolterol |
|
|
Which β2-adrenergic agonists are used for Prophylaxis?
|
Longer acting
= Sal-met-erol & Formo-terol |
|
|
β2-adrenergic agonists have a longer duration of action than _______ when given orally or by inhalation
|
Epinephrine
|
|
|
The bronchodilation with β2-adrenergic agonists is maximal by __1__ and lasts for __2__
|
1. 30 min
2. 3-4 hrs |
|
|
What are the common adverse effects of β2-adrenergic agonists?
|
Skeletal muscle tremor
Nervousness Occasional weakness **generally safe and effective when given in doses that avoid adverse systemic effects |
|
|
What are the 2 Sympathomimetics used as Bronchodilators?
|
Ephedrine
Epinephrine |
|
|
What is the downside of the Sympathomimetics?
|
by stimulating β1-adrenergic receptors they cause more cardiac side-effects = tachycardia, arrhythmia, worsening of angina
**also stimulate β2-adrenergic receptors to cause Bronchodilation |
|
|
Sympathomimetic that is administered by inhalation or SubQ injection, is effective and rapid acting for Acute Asthmatic attacks
|
Epinephrine
|
|
|
Mechanism of action of Muscarinic Antagonists?
|

block Acetycholine at muscarinic receptors = prevent Bronchoconstriction
|
|
|
What 2 effects do Muscarinic Antagonists ultimately cause?
|
1. inhibit vagal stimulation to relax bronchial smooth muscle = prevent bronchoconstriction
2. decrease mucus secretion **but do so without affecting those to NONMUSCARINIC stimuli |
|
|
Why do Muscarinic Antagonists not always work?
|
Parasympathetic involvement in bronchospastic responses varies widely
|
|
|
Muscarinic Antagonist that is given by IV or by Inhalation and produces Bronchodilation lasting for 5 hours, but may cause dry mouth, urinary retention, tachycardia, loss of visual accomidation, and agitation
|
Atropine
|
|
|
Muscarinic antagonist that is given by Aerosol or Nasal spray and allows delivery of large doses because it is poorly absorbed and therefore has minimal CNS effects
|
Ipra-tropium bromide
|
|
|
Muscarinic antagonist that has a longer duration of 24 hours
|
Tio-tropium
|
|
|
List the 6 Corticosteroids used to treat Asthma
|
1. Beclo-methasone
2. Budes-onide 3. Flu-niso-lide 4. Flu-tica-sone 5. Mo-metasone 6. Triam-cino-lone |
|
|
What is the mechanism of Corticosteroids in treating Asthma?
|
Inhibit the production of Inflammatory cytokines
1. reduce bronchial reactivity 2. increase airway caliber 3. reduce frequency of asthmatic attacks |
|
|
By what modes of administration are the Glucocorticoids given?
|
Orally
Injection Aerosol |
|
|
Which routes of administration of Glucocorticoids may produce severe adverse effects?
|
Oral or Parenteral
|
|
|
When is systemic administration of Glucocorticoids only given?
|
patients requiring urgent treatment
|
|
|
Inhaled preparation of Corticosteroids may cause what 2 adverse effects?
|
1. Oropharyngeal candidiasis
2. Hoarseness from vocal cord irritation |
|
|
What 2 Leukotrienes are potent Bronchoconstrictors secreted in Asthma and Anaphylaxis?
|
LTC4 & LTD4
|
|
|
What 2 drugs are LTD4-receptor antagonists?
|
Monte-lukast
Zafir-lukast |
|
|
How are Monte-lukast and Zafir-lukast administered? Who are they especially useful for? What type of asthma are they especially good for?
|
Orally
children unable to comply with inhalation therapy Aspirin-induced asthma |
|
|
Antileukotriene that inhibits 5-lipoxygenase to reduce leukotriene formation but has been withdrawn due to Liver toxicity
|
Zi-leu-ton
|
|
|
What is the mechanism of action of Omalizumab?
|
Monoclonal Ab that inhibits binding of IgE to mast cells
***does NOT inactivate already bound IgE |
|
|
Antiasthmatic that lessens the severity of asthma and reduces corticosteroid requirement
|
Omalizumab
|
|
|
Lowers plasma IgE levels and reduces bronchospastic antigen responses
|
Omalizumab
|
|
|
2 antiasthmatic drugs that are only effective when given prophylactically
|
Cromolyn
Nedocromil |
|
|
Cromolyn and Nedocromil have an acute protective effect when given before these 2 things
|
1. Exercise
2. Allergen exposure |
|
|
Cromolyn and Nedocromil inhibit bronchial hyper-reactivity in these 2 things
|
Antigen- & allergen-induced asthma
|
|
|
Cromolyn and Nedocromil do not affect these 2 things
|
Bronchial smooth muscles
Asthmatic bronchospasm |
|
|
What is the mechanism of action of Cromolyn and Nedocromil?
|
Alter delayed chloride channels in cell membranes to:
1. inhibit mast cell activation 2. reduce release of histamine and other mediators |
|
|
How are Cromolyn and Nedocromil administered? Why?
|
Aerosols b/c of poor GI absorption
|
|
|
Cromolyn and Nedocromil are less potent or effective when compared to _________
|
inhaled Corticosteroids
|
|
|
What are the characteristics of Mild Asthma?
|
Occasional symptoms occuring on exposure to allergens or pollutants, after exercise or Upper Respiratory viral infection
|
|
|
What are the characteristics of Severe Asthma?
|
Frequent attacks of wheezing dyspnea especially at NIGHT, resulting in limitation of activity
|

