![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
80 Cards in this Set
- Front
- Back
|
What is the difference between the desiccated thyroid medication and the synthetic thyroid medications? |
Desiccated thyroid -Natural thyroid derived from the thyroid of pigs and cattle -The term desiccation refers to the drying process used to make the med -This thyroid medication id rarely use d/t the possibility of allergic reactions to animal proteins. Synthetic Thyroid -a synthetic version of the human thyroid hormone -Eg. Levothyroxine (T4) (one to know) Liothyronine (T3) (NOT COVERED) |
|
|
What is levothyroxine used for (indication)? what is it's mechanism of action? What is it's pharmacological classification? |
Indication -Hypothyroidism Mechanism of Action -Given to replace what the thyroid gland cannot produce to achieve normal thyroid levels (euthyroid) -Work the same way as the endogenous thyroid hormone T4 (Thyroxine). Pharmacological Classification -Synthetic isomer of thyroxine |
|
|
What is the peak of the drug levothyroxin? |
Peak : 3-4 weeks ** Onset of action: 3-5 days Half-life: 6-7 days (PO) Duration of action: 1-3 weeks |
|
|
Why does levothyroxin require careful dosaging? |
Due to the narrow therapeutic index,and the high protein binding percentage (99.9%) careful dosage titration is required in order to prevent the over- or under-treatment of the drug. |
|
|
How does a health care professional know that levothyroxin is working? |
The therapeutic response is characterized by the disappearance of symptoms of hypothyroidism (depression, constipation, loss of appetite, weight gain, cold intolerance,syncope, and dry and brittle hair) For example, the pt should exhibit improved energy levels as well as improved mental and physical stamina. If the pt was receiving inadequate dosaging, a return of symptoms may occur |
|
|
What are the adverse effects of levothyroxine? |
Usually the result of an overdoes /too high a dose -**Most serious are cardiac dysrhythmias with risk for life threatening or fatal irregularities -other affects: Insomnia, tremors, headache, anxiety, nausea, diarrhea, cramps, menstrual irregularities, weight loss, sweating, heat intolerance, fever Refer to table 32-2 pg 613 |
|
|
Anti-thyroid drugs are used to treat what? |
Hyperthyroidism |
|
|
Propylthiouracil falls under what drug classification? |
Anti-thyroid drugs |
|
|
What is the mechanism of action of propylthiouracil? |
Mechanism of action -Impedes the formation of thyroid hormone** -Thereby normalizing the overall metabolic rate** -Reduces plasma concentrations of thyroid hormones (T3, T4). The drug is actively transported into the thyroid gland. Propylthiouracil depletes performed thyroid hormone stores and inhibits synthesis of thyroid hormones |
|
|
What are the indications for the use of propylthiouracil? |
Indications -medical treatment of hyperthroidism in pt's with Graves' disease -Preparative therapy to render pt euthyroid prior to receiving radioactive iodine (RAI) treatment or while awaiting ablative effects of radioactive iodine -Preperative therapy for stabilizing thyroid function prior to a thyroidectomy -Treatment of thyroid storm in addition to other therapeutic measures (eg. beta-blockers) |
|
|
What are the interactions and adverse effects for the use of propylthiouracil?
|
Interactions -Oral anticoagulants (increased activity), bone marrow suppressants (additive leukopenic effects) Adverse effects -Most serious: Liver and bone marrow toxicity (More on pg 615 table 32-4) |
|
|
How does a health care professional know that Propylthiouracil is working?
|
The therapeutic response is characterized by the disappearance of symptoms of hyperthyroidism -Weight gain, decreased pulse, B/P returned back to normal, decreased serum T4 levels -Symptoms indicating that a pt is not receiving adequate doses include tachycardia, insomnia, irritability, fever, and diarrhea, as well as continued signs and symptoms of hyperthyroidism |
|
|
Define insulin resistance in regards to diabetes mellitus |
Normally, Insulin attaches to the receptor sites on the cell to unlock the cell to allow glucose to enter. In insulin resistance the insulin receptor sites don't work properly, Therefore, the glucose is unable to enter the cell and remains in the bloodstream. |
|
|
How is type 1 diabetes treated? |
-Treatment includes administration of insulin, proper diet, and exercise. -onset is usually younger than 20 years of age |
|
|
How is type 2 diabetes treated?
|
-Controlled by diet, exercise, oral antihyperglycemic agents, and sometimes insulin. -Onset: older than 40 yrs of age but increasing in young adults, adolescents and children r/t rising prevalence of obesity |
|
|
How is gestational diabetes treated?
|
-Treatment includes proper diet, and exercise -Administration of insulin, if not controlled with diet and exercise. -Oral antihyperglycemics are contraindicated during pregnancy d/t lack of evidence r/t safe use during pregnancy** |
|
|
Antihypergycemis agents are also called _______ drugs |
Antidiabetic drugs |
|
|
Rapid acting insulins -What is the onset, peak, and duration? |
Rapid acting insulin -Onset: 10-15 mins -Peak: 1-1.5 hrs -Duration: 3-5 hrs Mnemonic: 15 mins feels like an hour during 3 rapid responses |
|
|
Short acting insulins
-What is the onset, peak, and duration? |
Short acting insulin -Onset: 30 mins -Peak: 2-3 hrs -Duration: 6.5 hrs Mnemonic: Short staffed nurses went from 30 pts 2 (to) 6 pt. |
|
|
Intermediate acting insulins
-What is the onset, peak, and duration? |
Intermediate acting (NPH) -Onset:1-3 hrs -Peak: 5-8 hrs -Duration: up to 18 Mnemonic: Nurses Play Hero 2 (to) 8 18 year olds. |
|
|
long acting insulins
-What is the onset, peak, and duration? |
Long acting -Onset: 90 mins (1.5 hrs) -Peak: N/A -Duration: up to 24 hrs Mnemonic: The 1.5 long nursing shifts never peaked but lasted 24 hrs. |
|
|
What is an insulin sliding scale? |
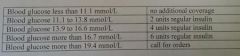
Sliding scale therapy approximates daily insulin requirements. The term “sliding scale” refers to the progressive increase in the pre-meal or nighttime insulin dose, based on pre-defined blood glucose ranges.
image from ch 33, work sheets |
|
|
What are the contraindications to diabetic medications? |
Contraindications -All antihyperglycemics-hypoglycemia -Oral medications: Allergy to sulfonamide antibiotics; potential for cross sensitivity -All oral antihyperglycemics-pregnancy** -Oral medications: Alpha glucosidase inhibitor-because of adverse GI effects; not recommended for pt's with inflammatory bowel disease, malabsorption, or intestinal obstruction |
|
|
What lab test is used to monitor the mean plasma glucose (PG) levels over the previous 3-4 months? |
Hgb (hemoglobin) A1C |
|
|
What is the general target for A1C plasma glucose (PG) for diabetic pt's? |
Target range is ≤ 7.0% in order to reduce the risk of microvascular complications -FPG or prepradinal (before meals) PG target of 4.0-7.0 mmol/L and PPG or postpradinal (after meals) of 5.0-10.0 mmol/L |
|
|
What are the interactions with anti-diabetic medications? |
Insulin: Corticosteriods (Increases plasma glucose (PG) levels) Metformin: Diuretics, Steroids (Additive hypoglycemia) Gliclazide: Coumarin derivatives, salicyles, propranolol, ACE inhibitors (increase hypoglycemia) Diuretics (decreased effectiveness; so induces hyperglycemia) |
|
|
A pt is experiencing the following signs and symptoms: -trembling -palpitations -sweating -anxiety -hunger confusion, headaches and dizziness What are they experiencing? |
Hypoglycemia |
|
|
What are the signs and symptoms of hyperglycemia? |
-Fatigue -Polydipsia (thirst) -Polyuria (frequent urination) -Blurred vision |
|
|
When is epinephrine use indicated? |
-Anaphylaxis -Bronchodilator (relieve bronchospams) - acute asthma, Chronic bronchitis -Cardiac Arrest- to restore cardiac rhythm -Emphysema, COPD -Adjunct in local anesthetics |
|
|
Beta 1 Adrenergic receptors does what? |
they are in the heart and increases the force of contraction and heart rate |
|
|
Beta 2 Adrenergic receptors does what?
|
they are in the lungs and cause bronchodilatory effects |
|
|
Alpha 1 Adrenergic receptors does what? |
Low doses -cause vasoconstrictor effects High doses -elevate B/P due to vasoconstriction |
|
|
What is the mechanism of action and indication for salbutamol? |
Mechanism of action -produces bronchodilation through stimulation of beta 2-adrenergic receptors in bronchial smooth muscle, thereby causing relaxation of bronchial muscle fibers Indications -the symptomatic relief and prevention of bronchospams due to bronchial asthma, chronic bronchitis and other bronchopulmonary disorders in which bronchospams is a complicating factor -The prevention of exercise-induced bronchospam |
|
|
What are the theraputic and pharmacological classifications of salbutamol? |
Therapeutic classification -Bronchodilator Pharmacological Classification -Short-acting selective beta 2 agonist |
|
|
The nurse is teaching a group of pts about the use of bronchodilators. It is important to remind them that using bronchodilators too frequently may cause which adverse effects? (select all that apply) a) Blurred Vision b) Increased Heart Rate c)Decreased Heart Rate d)Nausea e)Nervousness f)Tremors |
b) Increased Heart Rate
d)Nausea e)Nervousness f)Tremors |
|
|
A pt experiences a status asthmatics. What priority drug should the nurse prepare to administer? a)salbutamol sulphate (Ventolin) b)epinephrine c)theophylline (Theolair) d)montelukast |
b)epinephrine
|
|
|
In addition to status asthmatics, what is another indication for epinephrine? a)COPD b)Anaphalysis c)Emphysema d)Influenza |
b)Anaphalysis
|
|
|
ipratropium bromide (Atrovent) is what kind of drug? |
anticholinergic |
|
|
What is the mechanism of action of ipratropium bromide (Atrovent)? How is this drug administered? |
Mechanism of action -blocks acetylcholine (ACh) receptors to prevent bronchoconstriction. Routes -inhalation solution -Nasal Spray |
|
|
What are the indications of caffeine? |
Indications -CNS stimulant -Analeptic (restorative drug) -Promotes alertness -Heart stimulant in infants with bradycardia (NICU) -Enhancement of respiratory drive in infants (NICU) |
|
|
What is the mechanism of action and indication for Montelukast (singulair)? |
Mechanism of action -Inhibits the activity of leukotrienes, which decreases arachidonic acid-induced inflammation and allergen-induced bronchoconstriction. Indications -Prevention and treatment of asthma in adults and children 2 y/o and older. Note: this is a non-bronchodilating respiratory drug and falls under the therapeutic classification of Antileukotrine drugs |
|
|
What is the mechanism of action and indication for fluticasone propionate (flovent)? |
Mechanism of action -Prevent inflammation commonly provoked by the substances released from the mast cells Indications -the prophylactic management of steroid-responsive bronchial asthma in adults and children. For children, this includes pts not controlled on currently available prophylactic medication |
|
|
What are the adverse effects of fluticasone propionate (flovent)? |
Adverse effects -Mainly-Pharyngeal irritation, hoarseness, coughing, dry mouth, and oral fungal infections |
|
|
What are the 4 types of acid-controlling drugs? |
-Antacids -H2 antagonists -Proton Pump Inhibitors (PPIs) -Miscellaneous Acid Controlling drugs |
|
|
What are the 2 types of antacids? |
-Calcium carbonate (Tums) -Aluminum hydroxide-magnesium hydroxide-simethicone (Divol plus) |
|
|
What are the indications, Contraindications, an interactions with calcium carbonate (Tums)? |
Indications -symptomatic management of dyspepsia (heartburn) and mild gastroesphageal reflux disease (GERD) Contraindications -Hypercalcemia and hypercalciuria (eg. in hyperparathyroidism, vit D overdose, decalcifying tumors such as plasmacytoma, bone metastases) Interactions -Many (see table 39-1 for more) -Digoxin -Levothyroxin Iron supplements -Thiazide diuretics |
|
|
What is the therapeutic classification and dosage forms for Aluminum hydroxide-magnesium hydroxide-simethicone (Divol plus)? |
Therapeutic classification -Antacid-anti-flatulent Dosage forms -Suspension -Tablets |
|
|
What are the indications and contraindications for Aluminum hydroxide-magnesium hydroxide-simethicone (Divol plus)? |
Indications -heartburn -acid indigestion -Gas Contraindications -Hypermagnesemia; impaired renal function (b/c of Mg++, magnesium salts, in the presence of renal insufficiency, may cause CNS depression |
|
|
A pt with kidney failure wabts to take an antacid for "sour stomach". The nurse needs to consider that some antacids may be dangerous when taken by pts with kidney failure. Thus, which of the following types of antacids should be recommended? a)Sodium-containing antacids b)Aluminum-containing antacids c)Calcium-containing antacids d)Magnesium-containing antacids |
b)Aluminum-containing antacids
|
|
|
What are the therapeutic and pharmacological classifications of rantidine (Zantac)? |
Therapeutic Classification -Antiulcer Pharmacological classification -Histamine H2-receptor antagonist |
|
|
What is the mechanism of action, indication, and route for rantidine (Zantac)? |
Mechanism of Action -Antagonist of histamine at gastric H2-receptor sites. Inhibits both basal (mealtime) gastric secretions and gastric secretions induced by histamine -Blocks the G2 receptor of acid-producing parietal cells (results: decreased hydrogen ion secretion from the parietal cells, which results in an increase in the pH of the stomach and relief of symptoms associated with hyper-acidity Indication -Peptic ulcer disease (PUD), dyspepsia, stress ulcer prophylaxis, and GERD Route -PO, IV |
|
|
What is the therapeutic and pharmacological classifications of Omeprazole magnesium (losec)? |
Therapeutic -Antic-ulcer Pharmacological -H+, K+ -ATPase (the protein pump) inhibitor Note: this is given only PO and is in delayed response capsules and tablets |
|
|
What is the mechanism of action and indications of Omeprazole magnesium (losec)?
|
Mechanism of action -Omeprazole is a proton pump inhibitor that suppresses gastric acid secretion by secretion by secretion by specific inhibition of the H+/K+ -ATPase (the proton pump) in the gastric parietal cell, By acting specifically on the proton pump, omeprazole blocks the final step in acid production, thus reducing gastric acidity Indications -Duodenal ulcer -Gastric ulcer -NSAID-associated gastric and duodenal ulcers -Reflux esophagitis -Symptomatic gastroesophageal refluc disease (GERD) (ie heartburn and regurgitation -Zollinger-Ellison syndrome (Pathological hypersecretory condition) -Eradication of H. pylori |
|
|
What is Losec triple therapy? |
Losec in combination with clarithromycin and amoxicillin pr metronidazole, is indicated for the treatment of pts with peptic ulcer disease associated with H. pylori infection. -PPI + 2 antibiotics (metronidazole is generally used for those with penicillin allergies) |
|
|
What are the three types of antidiarrheals? |
1)Absorbents -Bismuth subsalicylate (pepto bismol) 2) Antimotility drugs -Opiates (loperamide (imodium)) 3) Probiotics (intestinal flora modifiers) -Bacterial replacement drugs (lactobacillius acidophius or lactofil, florababy ) |
|
|
What is the mechanism of action, therapeutic and pharmacological classifications of bismuth subsalicylate (Pepto Bismol)? |
Mechanism of action -Firms the stool, binds bacterial toxins, and exhibits antimicrobial activity Therapeutic classification -Antiacid-antidiarrheal Pharmacological classification -Absorbents |
|
|
What is the mechanism of action, therapeutic and pharmacological classifications of loperamide (Imodium)?
|
Mechanism of action -Binds to the opiate receptor in the gut wall; inhibits the release of acetylcholine prostaglandins and, thereby decreasing propulsive peristalsis, and increasing intestinal transit time. Increased tone of the anal sphincter, thereby decreasing in continence and urgency Therapeutic Classification Antidiarrheal Pharmacological classification opiates |
|
|
What is the mechanism of action, therapeutic and pharmacological classifications of lactobaccillus?
|
Mechanism of action -Restores normal bacterial balance and suppress growth of diarrhea-causing bacteria Therapeutic classification Antidiarrheal Pharmacological classification Probiotics |
|
|
What are the 5 types of laxatives? |
1)Bulk Forming -Psyllium hydrophillic mucilloid (Metamucil) 2)Emollient -Docusate salts or docusate sodium (colace) 3)Hypersosmotic -glycerin (glycerin suppositories) -Lactulose -Polythylene glycol 3350 (Klen-Prep, PegLyte) 4)Saline -Magnesium hydroxide 5) Stimulant laxatives -bisacodyl (Dulcolax) -senna (Senokot) |
|
|
What is the mechanism of action, therapeutic and pharmacological classifications of Psyllium hydrophillic mucilloid (Metamucil)?
|
Mechanism of action -Combines with H2O in the intestine, to form an emollient gel that promotes peristalsis and decreases transit time Therapeutic classification Laxative Pharmacological classification Bulk Forming |
|
|
What is the difference between gram-positive and gram-negative bacteria? |
Both -Have a layer of peptidoglycan Gram-positive -The peptidoglycan layer is thicker than the negative -have a thick outer capsule -Appears dark violet or purple after staining, retains the color of crystal violet after washing with alcohol Gram-negative -Cell wall structure is more complex, with smaller outer capsule, and 2 cell membranes (an outer and inner membrane) -Has a thick lipid bilayer on the outside, which is selectively permeable; not everything can pass through it, and one of those things is in the gram stain. -Appears pink or red after staining, color of crystal violet will not be retained after washing with alcohol |
|
|
What is the pharmacological and therapeutic classification of sulfamethoxazole-trimethoprim? |
Pharmacological classification -sulfonamide (bacteriostatic) & trimethoprim (bacteriostatic or bactericidal depending on the organism and conditions); combo is bacterial. Folate antagonists Therapeutic classifications -Antibacterial Note: Broad spectrum- active against many Gram-pos and Gram-Neg bacteria |
|
|
What is the difference between bactericidal antibiotics and bacteriostatic antibiotics? |
Bactericidal: Antibiotics that kill bacteria bacteriostatic: Antibiotics that do not kill bacteria but rather inhibit their growth. |
|
|
What are the 4 sub-classes of Beta-lactam Antibiotics? |
1)Penicillins (Pen G, Pen V; natural penicillin's*) -Effective against gram-positive bacteria, little ability against gram negative 2)Penicillinase-resistant penicillins -Effective against gram-positive, little ability to kill gram negative 3)Aminopenicillins (Amoxicillin*) -Broad spectrum 4)Extended-spectrum penicillins -Excellent gram-positive and gram-negative coverage |
|
|
A pt is started on penicillin medication therapy to treat an infection. What priority drug substance(s) should the nurse teach the pt to avoid to prevent drug interactions? (select all that apply) a)Alcohol b)Oral contraceptives c)digixin d)non-steroidal anti-inflammatory drugs e)Warfarin f)Anticonvulsants |
Oral Contraceptives: Whether penicillins decrease the effectiveness of oral contraceptives is controversial. Some clinicians recommend adding an alternative method of contraception for the duration of the cycle when a penicillin is taken.
NSAID’s: Compete for protein binding. More free and active penicillin [may be beneficial]. Warfarin: reduced Vit K from the gut flora. Enhanced anticoagulant effect of warfarin. |
|
|
Cephalosporins have how many generations of drugs? whats the main difference between them? |
1st generation (cefazolin IV/IMcephalexin (Keflex))
-Gm pos bacteria; limited activity against Gm neg bacteria 2nd generation (cefoxitin sodium IV,cefaclor po) -Gm pos and Gm neg bacteria 3rd generation (Cefixime po, Ceftriaxone IV) -Most potent against Gm neg bacteria; less potent than 1st and 2nd generation against Gm pos bacteria 4th generation (Cefepine hydrochloride - IV) -Activity against Gm neg & Gm pos bacteria Note: The earlier generations have more gram-positive coverage. The later generations have the most gram-negative coverage.The level of Gram neg coverage increases with each successive generation. |
|
|
A pt is to receive an antibiotic therapy with a cephalosporin. When assessing the pts drug history, the nurse recognizes that an allergy to which type of drug may be a possible contraindication to cephalosporin therapy? a)Cardiac glycosides b)Thiazide diuretics c) Penicillins d) Macrolides |
Answer: C Patients who are allergic to penicillins have an increased risk of allergy to other β -lactam antibiotics. The incidence of cross-reactivity between cephalosporins and penicillins is reported as between 1 and 4%. Patients reporting penicillin allergy need to describe their prior allergic reaction; it is important to document the type of reaction. The decision to treat with cephalosporin therapy in such cases is often a matter of clinical judgement, based on the severity of reported prior reactions to penicillin drugs, the nature of the infection, the drug susceptibility of the infective organism if known, and the availability and patient tolerance of other alternative antibiotics. Generally speaking, only those patients with a history of throat swelling or hives from penicillin should not receive cephalosporins. Some patients may require skin testing and desensitization. Penicillins and cephalosporins are practically identical in their mechanisms of action, drug effects, therapeutic effects, adverse effects, and drug interactions. Their use is contraindicated in patients who have shown a hypersensitivity to them and any patient with a history of life-threatening allergic reaction to penicillins. |
|
|
A patient prescribed azithromycin (Zithromax) expresses concern regarding GI upset that was experienced when previously prescribed an erythromycin antibiotic. What is the nurse’s best response?
a) “Take an over-the-counter antiemetic to lessen the nausea.” b)“Stop taking the drug if you experience heartburn and diarrhea.” c)“I will call the health care provider and request a different antibiotic.” d)“This drug is like erythromycin with less gastrointestinal adverse effects.” |
d)“This drug is like erythromycin with less gastrointestinal adverse effects.”
|
|
|
What are the 7 classes of antibiotics? |
1)Sulfonamides
-sulfamethoxazole-trimethoprim 2) β – lactam Antibiotics -Penicillins 3) Macrolides -azithromycin 4)Tetracyclines -doxycycline hyclate 5)Aminoglycosides -gentamicin 6)Quinolones -Ciprofloxacin 7) Other drugs -Metronidazole |
|
|
This is a general term that encompasses all types of clinical problems related to medication use.
|
An adverse drug event |
|
|
a preventative ADE(adverse drug error) in which there is a compromise of the 10 Rights of med admin. These can occur during the prescribing, dispensing, administering or monitoring of drug therapy.
|
medication error |
|
|
is any reaction to a drug that is unexpected and undesirable and occurs at therapeutic drug dosages.Adverse Effects: predictable adverse drug reactions (ADR’s). Listed in your drug guide or e-CPS.
|
Adverse drug reaction |
|
|
is not the result of a known pharmacological property of a drug or patient allergy but instead occurs unexpectedly in a particular patient. Such a reaction is a genetically determined abnormal response to ordinary doses of a drug. The study of such traits, which are solely revealed by drug administration, is called pharmacogenetics (see Chapter 5 ).These reactions are usually caused by a deficiency or excess of drug-metabolizing enzymes. Many pharmacogenomics disorders exist, for example, glucose-6 phosphate dehydrogenase (G6PD) deficiency .
|
idiosyncratic reaction
|
|
|
During antibiotic therapy, the RN must monitor for S & S of an anaphylactic reaction. Which of the following may indicate an anaphylactic reaction? (Select all that apply.)
-Wheezing. -Nausea and vomiting. -Shortness of breath. -Hypertension. -Swelling of the tongue. -Itching. -Black, hairy tongue. -Hives. -Hypotension. -Tachycardia. -Bradycardia. -Fainting. -Tingling sensation. |
Wheeze, N & V, SOB, Swelling of the tongue, itching, hives, hypotension, tachycardia, fainting, tingling sensation.
|
|
|
Quinolones are a class of antibiotics known for several significant complications. Which are possible adverse
a)Ototoxicity b)Nephrotoxicity c)Tendon rupture d)Prolongation of the QT interval |
Answer: C, D
Adverse Effects: More worrisome is a heart effect that involves prolongation of the QT interval on the electrocardiogram (ECG). Dangerous cardiac dysrhythmias are more likely to occur when quinolones are taken by patients who are also receiving class Ia and class III antidysrhythmic drugs, such as disopyramide and amiodaronehydrochloride. For this reason, such drug combinations are best avoided. A labelling warning is required by Health Canada for all quinolones because of the increased risk of tendinitis and tendon rupture with use of these drugs. This effect is more common in older adults, patients with kidney failure, and those on concurrent glucocorticoid therapy (e.g., prednisone). In addition, a second labelling warning was required concerning worsening symptoms such as muscle weakness and breathing difficulties in patients with myasthenia gravis. Central nervous system (CNS) stimulation in the form of seizures has been reported. |
|
|
What is the therapeutic classification and indication for acyclovir? |
Therapeutic classification -Antiviral Indications -PO: initial episodes, and unusually frequent recurrences of genital herpes; acute treatment of herpes zoster (shingles) and varicella (chickenpox) -Cream: topical management of genital herpes -Ointment: Management of initial episodes of genital herpes, non-life threatening cutaneous herpes infections in immunocompromised pts -IV: inital and recurent herpes viruses (HSV-1 and HSV-2) and herpes Zoster (VZV) in immunocompromised pts |
|
|
The nurse is administering acyclovir (Zovirax) and recalls that it is considered the drug of choice for treatment of which viral infection(s)? Select all that apply.
a)Herpes Simplex Virus (HSV) b)Human immunodeficiency virus (HIV) c) Respiratory syncytial virus (RSV) d)Varicella-zoster virus (VZV) |
a)Herpes Simplex Virus (HSV)
d)Varicella-zoster virus (VZV) |
|
|
What is the mechanism of action, indication and therapeutic class for amantadine? |
Mechanism of action -Inhibits viral uncoating through interference of M2 ion-channel function Indication -Prevention and treatment of influenza A infections Therapeutic classification -Antiviral-antiparkinsonian agent |
|
|
A patient calls the clinic nurse to ask for oseltamivir (Tamiflu) “because I was exposed to the flu over the weekend at a family reunion.” The nurse knows that oseltamivir is used for which of the following? Select all that apply.
a)Prevention of infection after exposure to influenza virus types A and B b)Reduction of the duration of influenza in adults c)Treatment of topical herpes simplex virus infections e)Reduction of the severity of shingles f)Treatment of lower respiratory tract infections caused by respiratory syncytial virus |
a)Prevention of infection after exposure to influenza virus types A and B
b)Reduction of the duration of influenza in adults |
|
|
The nurse is preparing to administer the aerosol form of ribavirin. Which condition is a contraindication to this drug? a)Asthma b)Pregnancy c)Hypertension d)Type 2 diabetes |
Answer: B
Ribavirin aerosol is contraindicated in women or girls who are or may become pregnant during exposure to the drug. Ribavirin may cause fetal harm, and respiratory syncytial virus infection is self-limited in this population. Ribavirin is not completely cleared from human blood even 4 weeks after administration. Although there are no pertinent human data, ribavirin has been found to be teratogenic and/or embryolethal in nearly all species in which it has been tested; however, pregnant baboons given up to 120 mg/kg/day of ribavirin over a 4 day period within the 20 days of organogenesis during gestation failed to exhibit any teratogenic effect. (Canadian Pharmacists Association, 2016g) |

