![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
25 Cards in this Set
- Front
- Back
|
Where does inflammation occur for UC? |
Large intestine, limited to inner lining of the intestinal walls. |
|
|
For IBD, there is an increased number of which innate immune cells in the lamina propria, causing an elevation in which cytokines? |
1. TNF-alpha 2. IL-1beta 3. INF-gamma, cytokines of the interleukin-23-Th17 pathway |
|
|
What are common symptoms to both UC and CD? (6) |
|
|
|
What are complications to IBD? (3) |
1. Obstructions in bowel 2. Ulcers 3. Malnutrition |
|
|
Define: Distal colitis |
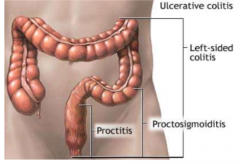
Proctitis and proctosigmoiditis |
|
|
Define: Left-side colitis |
Colitis up to the splenic flexure |
|
|
Define: extensive colitis |
Colitis up to the hepatic flexure |
|
|
Define: Pancolitis/ ulcerative colitis |
Colitis affecting the whole colon |
|
|
Ulcerative colitis has an increased risk for colonic cancer if disease is ____ years. |
>10 |
|
|
How is mild UC defined? |
|
|
|
How is moderate UC defined? |
|
|
|
How is severe UC defined? |
|
|
|
How is fulminant UC defined? |
|
|
|
Goals of treatment of IBD? (6) |
|
|
|
What is induction vs. remission? |
Induction: getting back to normal state
Remission: maintaining normal state |
|
|
What is first line therapy to induce remission? |
5-ASA per rectum topical Stay on 5-ASA to maintain remission |
|
|
What is second line therapy to induce remission? |
Steroid PO Oral prednisone |
|
|
What is third line therapy to induce remission? |
Oral prednisone and immunosuppresive treatment, biological therapy or surgery. |
|
|
What are the treatment options for mild UC? (9) |
|
|
|
Define: informed decision |
Patient knows all there is to know about medication before making a decision on whether to take it or not. This includes symptoms, side effects, interactions, monitoring and duration of therapy. |
|
|
What is the first line therapy for severe UC? |
Oral prednisone 30-60mg/day, tapering down to 0 (12-16 weeks). |
|
|
What is the second line therapy for severe UC? |
IV steroids in hospital (3-10 days) If remission occurs, switch to oral prenisone and taper down to 0. Continue or restart oral 5-ASA.
If failure, biological therapy, iv cyclosporine, or colonectomy |
|
|
When is cyclosporine used in UC? |
It is offered for patients that refuse surgery or biological therapy. |
|
|
What are contraindications and adverse events with using infliximab? |
Active infections, TB and other opportunistic infections, invasive fungal infections, congestive heart failure, or hypersensitivity. Risk of lymphoma. May cause liver toxicity (increase ALT and AST). |
|
|
Why do you use azathioprine in addition to infliximab? |
In 14-19% of patients, antibodies for infliximab develop. This is reduced to 1-2.5% if used with azathioprine. |

