![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
77 Cards in this Set
- Front
- Back
|
What types of psoriasis are acute forms? |
1. Guttate 2. Pustular 3. Erythrodermic |
|
|
What are non-acute forms of psoriasis? |
1. Psoriatic arthritis (distal joints of fingers (asymmetrical) and on feet) 2. Nail psoriasis ("oil spots", punctate pitting, and crumbling) |
|
|
Describe guttate psoriasis: |
- Explosive tear drop eruptions - Trunk and extremities - Precipitated by streptococcal infection, typically in children with no prior exposure |
|
|
Describe pustular psoriasis: |
Sterile pustules on palms and soles |
|
|
Describe erythrodermic psoriasis: |
Spontaneous, extensive peeling Can be a medical emergency, causing electrolyte imbalance and septicemia. |
|
|
What is considered mild, mild-moderate, and severe psoriasis? |
Mild: <3% Mild to moderate: 3-10% Severe: >10%
Severity is also based on thickness, scaliness, and redness. |
|
|
Treatment options for mild to moderate disease? |
Topical treatment: Emollients, keratolytics, corticosteroids, calcipotriol, tazarotene, coal tar, anthralin
Note: nails, palms, and soles do not respond well to topical treatment - need oral. |
|
|
Treatment options for severe disease? |
1. Phototherapy 2. Systemic immunomodulators 3. Systemic biologic agents |
|
|
How is phototherapy used? |
- used in conjunction with other treatment - dermatological referral - proposed mechanism: electromagnetic therapy that depletes cells involved in immune response |
|
|
Which immunomodulators are used? |
1. Methotrexate 2. Cyclosporine 3. Acitretin (Combination therapy in a rotational cycle is required for 1-2 years intervals) |
|
|
Which biologic agents are used? |
1. Anti-TNFs (infliximab, adalimumab, etanercept) 2. T-cell targeted (alefacept) 3. Monoclonal antibodies (ustekinumab) |
|
|
When should psoriatic patients be referred? |
1. All patients with psoriasis should be under care of doctors 2. Refer patients with moderate to severe psoriasis: - who has generalized disease, is acutely ill, or requires special treatment - who has localized disease that doesn't respond to treatment |
|
|
Which emollients are used? |
1. Vaseline 2. Silicone 3. Ceramides (occlusive bases) |
|
|
How do emollients treat psoriasis? |
Alleviate dryness by hydrating the stratum corneum and reducing water evaporation. They are applied after a 15 minute bath in water. |
|
|
Which keratolytics are commonly used? |
1. Salicylic acid 2. Sulfur 3. Urea 4. Lactic acid |
|
|
How are salicylic used? |
Salicylic acid and other keratolytics are used to remove scales. Can be used alone or with topical steroids or tar. Can also enhance penetration of other drugs. |
|
|
Define: salicylism |
When salicylic acid is acid is extensively applied and systemically absorbed, nausea, vomitting, tinnitis or hyperventilation can occur. |
|
|
Purpose and mechanism of action of coal tar? |
Coal tar (e.g. crude coal tar 5% or LCD (liquid carbonis detergens) have antimitotic and antipruritic activity. They can be combined with corticosteroids, anthralin, UVB light or oral therapy for psoriasis.
Also useful for corticosteroid resistance. |
|
|
Adverse effects of coal tar? |
- Messy/ stains - Malodor - Irritating and can cause folliculitis (when applied in circular motion) |
|
|
Describe: plaque psoriasis |
Most common form (chronic and stable) Affects scalp, elbows, knees, back, and is symmetrical.
Auspit'z sign (punctate bleeding when scales are scraped off) |
|
|
Describe: Inverse (flexural) psoriasis |
Affects gluteal folds, genitals, perianal, axillary No visible scaling |
|
|
Which areas of the body require 1. low 2. moderate and 3. high potency for corticosteroid use? |
Low: face, groin, intertriginous areas (skin folds) can be treated with 1%Hydrocortisone
Moderate: Scalp, elbows, knees can be treated with 0.1% betamethasone
High: very resistant plaques
Other: intralesion injections used for dormant, solitary lesions |
|
|
Regimen of topical corticosteroids? |
Use BID until skin is normal (3-4 weeks), then reduce potency and use on weekends only (intermittently) for maintenance.
If insufficient: 1. Occlusion (CS + plastic wrap QHS - caution with atrophy) 2. Combine CS with calcipotriene or tazarotene 3. Combine with coal tar and/or anthralin |
|
|
Side effects of topical corticosteroids? |
1. Stinging and burning 2. Skin atrophy, striae, purpura (easy bruising), local hair growth 3. Tachyphylaxis (decreased effect of drug over time) 4. Flares upon abrupt withdrawal 5. Pituitary-adrenal axis suppression |
|
|
What is calcipotriol, MOA, therapeutic use? |
- Topical vitamin D3 analogue, which affects calcium metabolism and regulates epidermal growth - Regulates keratinocyte proliferation and differentiation - Unpredictable response (70%), and takes 4-6 weeks - No stains, tachyphylaxis, atrophy or mess |
|
|
Cons of using calcipotriol? |
1. Unpredictable response and costly 2. Irritant (burns and stings) 3. Hypercalcemia risk (don't exceed 100g/ week) |
|
|
MOA and therapeutic use of anthralin? |
- Interferes with DNA synthesis, preventing proliferation - Used for widespread plaques - Can be used alone or in combo with UVB, topical steroids, coal tar, or oral therapy |
|
|
Cons of anthralin? |
Stains and burns, messy as a thick paste (Lassar's), and difficult to apply. |
|
|
What is the long contact time regimen for anthralin? |
Apply at bedtime, then rinse off in the morning. Gradually increase concentration from 0.1% to 0.5% as tolerated. |
|
|
What is the short time contact regimen for anthralin? |
Begin with 0.1% for 5 minutes once daily, then increase with tolerance up to 30 minutes once daily, then 2%. Wipe off oil before showering. |
|
|
Anthralin application method? |
1. Apply daily, then once or twice weekly for maintenance 2. Wear plastic gloves 3. Apply petrolatum to surround skin to avoid irritation 4. Don't apply to face, genitalia, or intertriginous skin areas 5. Remove skin stains with salicylic acid 5% ointment |
|
|
MOA of tazarotene? |
Vitamin A derivative. - Binds to retinoid receptors - Normalizes keratinocyte differentiation - Decreased proliferation and infl. - Similar in efficacy to moderate potency CS (slow onset but extended response) |
|
|
Disadvantages of tazarotene? |
- Burning, stinging, erythema, pruritis, dryness, peeling, photosensitizing - Expensive Pregnancy category X (contraception advised) |
|
|
When is tazarotene topical cream/ gel 0.05-0.1% used? |
Used to prevent steroid flair upon D/C (63% occurence using steroids alone, vs. 14% occurence with tazarotene) - Use with med-high potency topical steroid QD-BID and tazarotene gel QHS - after 2-4 weeks, decrease potent topical steroids to weekend use only - use for >4-6 weeks before d/c |
|
|
Indications for systemic therapy? |
- Failure to respond to adequate trial of topical treatment |
|
|
Which agent is more effective, vit. D or coal tar? |
- Vitamin D |
|
|
How does efficacy compare between use of steroid alone, versus steroid + vitamin D? |
- Combination therapy is more effective than steroid or vitamin D use alone |
|
|
Which agent causes more adverse skin events (such as skin irritation), potent corticosteroids or vitamin D agents? |
- Potent CS are less likey to cause local adverse events than vitamin D agents |
|
|
MOA of methotrexate? |
Folic acid antagonist - Binds to dihydrofolate reductase and inhibits pyrimidine synthesis - Decreased DNA replication, immunosuppression on activated T-cells, and antiproliferation in epidermal cells. |
|
|
Use of methotrexate? |
- Induction and maintaining remission for psoriatic arthritis and nails |
|
|
Dosing regimen of methotrexate? |
- 7.5-25mg divided TID every 12 hours once weekly - When D/C, contraception needed for 1 month (women) and 3 months for men (oligospermia) |
|
|
Adverse events of methotrexate? |
- Bone marrow suppression - Hepatic fibrosis (hepatotoxicity >1.5g cumulative dose) - Infection - Teratogenic |
|
|
Contraindications of methotrexate? |
- Abnormal liver or renal function |
|
|
Monitoring parameters for methotrexate use? |
- Perform baseline and blood count every 4 weeks |
|
|
What other medication should be used in conjunction with methotrexate therapy? |
Folic acid, 1mg daily - Protects against SEs such as stomatitis |
|
|
Drugs interactions with methotrexate? |
- Sulfonamides - ASA, NSAIDS, Penicillin (decreased renal elimination of methotrexate; toxicity) |
|
|
MOA of Acitretin? |
Systemic retinoid (vit. A derivative) - Etretinate metabolite (t1/2=120 days) with shorter half life (t1/2=2-4 days) - Regulates: 1. Epithelial cell proliferation + differentiation 2. Immunologic function |
|
|
Use of Acitretin? |
Faster response than methotrexate in acute inflammatory forms of psoriasis |
|
|
Disadvantages of Acitretin? |
- Poor (20-30%) response for psoriasis vulgaris (use with UVB, PUVA or CS) - Elevated liver enzymes (hepatitis) - Elevated lipids (TG and chol.) - Muscles aches - Teratogenic (3 yers DC tx( - Mucocutaneous (dry lips, nose, eyes, skin, alopecia) - Ossification disorder (hyperostosis) |
|
|
Dosing regimen for Acitretin? |
25-50mg daily with food until lesions resolve (8 – 12 weeks) |
|
|
Monitoring parameters for Acitretin? |
Liver function tests and lipids at baseline, every 1-2 weeks until stable |
|
|
MOA of cyclosporine? |
Immunosuppressive agent - inhibits calcineruin --> decreased IL-2 --> decreased helper T-cells --> immunosuppression |
|
|
Use of cyclosporine? |
- induces remission (90% clearance of lesions) within 10 weeks |
|
|
Dosing regimen of cyclosporine? |
- 2-5 mg/kg/day (based on ideal body weight) - Do not give continuously for longer than 1 year |
|
|
Monitoring parameters of cyclosporine? |
BP and renal function |
|
|
Disadvantages of cyclosporine? |
- when D/C, disease recurs within 2-4 months - Renal impairment (reversible) |
|
|
What are the 3 types of biologic therapies? |
1. T-cell modulators (Alefacept /Amevive) 2. TNF-a inhibitors (Infliximab /Remicade, Etanercept /Enbrel, Adalimumab /Humira) 3. Cytokine (interleukin) inhibitors (Ustekinumab /Stelara) |
|
|
Drugs ending with mab: |
Monoclonal antibodies |
|
|
Drugs ending with ximab: |
Chimeric (mouse + human) monoclonal antibodies and may for neutralizing antibodies |
|
|
Drugs ending with zumab: |
Humanized monoclonal antibodies, less likely to form neutralizing antibodies |
|
|
Drugs ending with cept: |
Involve the fushion of a receptor to antibody (the Fc portion of the humaN IgG1) |
|
|
Dosing regimen for Infliximab? |
5mg/kg IV at week 0, 2, 6 Maintenace: 5mg/kg every 8 weeks (IV over 2-3 hours) |
|
|
Dosing regimen for Etanercept? |
(Plaque) Initial: 50mg SC twice weekly x 3 months Maintenance: 50mg SC weekly |
|
|
Dosing regimen for adalimumab? |
80mg/week SC, then 40mg Q2 weeks |
|
|
Dosing regimen for alefacept? |
IM: 15mg once weekly x 12 weeks IV: 7.5mg once weekly x 12 weeks (follow by 12 weeks no tx) |
|
|
Dosing regimen for ustkinumab? |
SC: 45mg week 0, 4, then q12 weeks |
|
|
Treatment options for mild disease (= max 5% of BSA) |
Moisturizers, emollients, topical CS, coal tar, anthralin, calcipotriol, tazarotene |
|
|
Treatment options for moderate disease (= 10>PASA>8; 10%>BSA>5%) |
Mild treatment plus: phototherapy, systemic therapy (e.g. methotrexate, cyclosporine), oral retinoids, biologic agents |
|
|
Treatment options for severe disease (= PASI >10; BSA >10%) |
Mild treatment plus: phototherapy, systemic therapy (e.g. methotrexate, cyclosporine), oral retinoids, biologic agents |
|
|
MOA of UVB phototherapy? |
UVB radiation (290-320nm) - Reduces DNA synthesis of epidermal cells via an immunomodulatory effect |
|
|
UVB therapy regimen? |
UVB light exposure, 30s to 10min 3 x weekly for 20 sessions - 80% clearing of extensive psoriasis |
|
|
Define: Goeckerman technique |
Coal tar + UVB - Apply tar preparation; leave overnight - Remove tar in AM with mineral oil and bathe - Expose skin to UVB (minimal erythema) - Bathe and gently scrub scales - Apply tar or steroids under occlusion |
|
|
Define: Ingram Technique |
Coal tar + UVB + Anthralin - bathe in coal tar bath - expose to UVB light - Apply anthralin paste with spatula - Dust with talc, cover with gauze - Remove paste with mineral oil and base after 8-12 hours |
|
|
MOA of PUVA? |
Oral psoralens + UVA light (320-400nm) - suppress cell division - psoralen activated by UVA to chelate DNA |
|
|
Dosing regimen for PUVA? |
Methoxsalen (8-MOP): 0.6-0.8mg/kg given 2 hours before exposure to UVA. Repeat 2-4 times a week for 6 – 8 weeks. Clears 90% patients. - restrict to 150-200 treatments - use sunscreen at least 8 hours after treatment |
|
|
Disadvantages of PUVA? |
Cataracts, skin cancer (basal and squamous cell cancers, melanomas) |
|
|
Which treatment do you use first? a. TAR+UVB or NBUVB or PUVA b. Systemic treatment (acitretin, methotrexate, cyclosporine, etc.) |
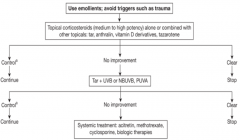
A. Switch to B when no improvement. |

