![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
59 Cards in this Set
- Front
- Back
|
Arachidonic acid is released or mobilized from cell membranes phospholipids by: (3) |
1. Phospholipase A2 2. Phospholipase C 3. Diglyceride lipase |
|
|
What are isoprostanes?
What are their functions? |
Prostaglandin stereoisomers.
They can bind to prostaglandin receptors as a potent vasoconstrict and may contribute to inflammation. |
|
|
How are isoprostanes synthesized? |
Formed by perioxidation of arachidonate by free radicals while part of cell membrane.
COX (cyclooxygenases) not needed. |
|
|
How does COX -1 and COX-2 differ, in terms of how they are expressed. |
COX 1 - expressed all the time, in all cells
COX 2 - expression is inducible |
|
|
Which enzymes synthesize prostaglandins? |
COX (cyclooxygenase) |
|
|
What group of drugs blocks COX? (giggle giggle) |
Non-steroidal anti-inflammatory drugs (NSAIDs) |
|
|
The precursor for prostaglandins and thromboxanes: |
PGH2 |
|
|
T/F: Most cells make several types of prostanoids. |
False.
Most cells make one or two dominant ones. |
|
|
T/F: Specific isomerases and synthases required for each type of prostaglandin. |
True. |
|
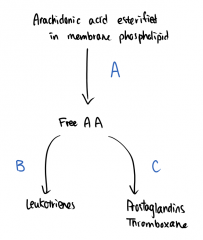
Label A, B, and C. |
A - Phospholipase A2, Phospholipase C and Diglyceride B - Lipoxygenase C - Cyclooxygenase |
|
|
Which receptors do PGE2 act on? (4) |
EP1 EP2 EP3 EP4 |
|
|
Effects of EP1? (4) |
1. Mediate stress response 2. Inflammatory thermal hyperalgesia (e.g. sunburn) 3. Activate GI smooth muscle 4. Protect against NSAID ulcers (stomach) |
|
|
Effect of EP2? (3) |
1. Facilitate pain transmission (spinal cord) 2. Join inflammation 3. Fertility and uterine contraction |
|
|
Effects of EP3? (6) |
1. Fever generation 2. Angiogenesis (inflammation and cancer) 3. Activate GI smooth muscles 4. Inhibit gastric secretions 5. Protect against NSAID induced ulcers (intestines) 6. Mediates pain associated from viruses |
|
|
Effects of EP4? (6) |
1. Increase bone turnover |
|
|
Which receptors do PGD2 act on? |
DP (1, 2) |
|
|
Effect of DP (1,2)? (3) |
1. Bronchoconstriction 2. Inhibits platelet aggregation 3. Promotes sleep |
|
|
Which receptor does PGI2 act on? |
IP |
|
|
Effects of IP? (7) |
1. Vasodilation 2. Bronchodilation 3. Inhibit platelet aggregation 4. Angiogenesis (cancer) 5. Increase renal H2O and Na clearance 6. Uterine relaxation 7. Sensitize nocireceptors |
|
|
Which receptors does PGF2a act on? |
FP (A, B) |
|
|
Effects of FP (A,B)? (5) |
1. Vasoconstriction 2. Activate GI smooth muscles 3. Bronchoconstrictor 4. Uterine contraction 5. Regulate IOP |
|
|
Which receptor does TXA2 act on? |
TP (A,B) |
|
|
What did sushi A say to sushi B? |
WASABI!! |
|
|
Effects of TP(A,B)? (7) |
1. Potent vasoconstrictor 2. Potent bronchoconstrictor 3. Mitogen (smooth muscle) 4. Promotes platelet aggregation 5. Angiogenesis (cancer) 6. Decrease renal function 7. Uterine contraction |
|
|
Which prostaglandins (and receptors) protect against NSAID ulcers? (2) |
1. PGE2 - EP1 - Stomach 2. PGE2 - EP3 - Intestines
|
|
|
Which prostaglandins (and receptors) regulate vasodilation and constriction? (4) |
1. PGE2 - EP4 - Vasodilation 2. PGF2a - FP (A,B) - Vasoconstrict 3. PGI2 - IP - Vasodilate 4. TXA2 - TP(A,B) - Potent vasoconstrictor |
|
|
Which prostaglandins (and receptors) cause bronchoconstriction? (3) |
1. PGD2 - DP(1,2) 2. PGF2a - FP(A,B) 3. TXA2 - TP(A,B) |
|
|
What is the function of corticosteroids? (2)
|
1. Blocks synthesis pathways for PG and LT
2. Blocks phospholipase A2 |
|
|
How do NSAIDs act as analgesics? |
Blocks synthesis of PGE2 in periphery and CNS. |
|
|
How do NSAIDs treat dysmenorrhea? |
Blocks synthesis of PGE2 and PGF2, which cause contractions. |
|
|
How do NSAIDs treat patent ductus arteroisis? |
Blocks PGE2 synthesis. PGE2 keeps fetal ductus arteriosus open. |
|
|
How are prostaglandins metabolized? |
They are oxidized by prostaglandin 15-OH dehydrogenase, and also undergo hydrate to inactive metabolites. Inactive metabolites are excreted in urine. |
|
|
1. MOA and 2. therapeutic use of Alprostadil? |
1. Is a prostaglandin agonist - PGE2 analogue (also know as PGE1)
2. Is a vasodilator, for treatment of ED (intracavernosal injection; secondary option) and ductus arteosus patent in neonates awaiting cardiac surgery. |
|
|
Adverse effects of Alprostadil? |
Penile pain, common in IC injections (NO REALLY.) |
|
|
What is Bruce Lee's favourite drink? |
wa-TAAAAAA! |
|

1. MOA and 2. therapeutic use of Dinoprostone? |
1. EP receptor agonist (PGE1 derivative). Promotes uterine contraction and cervical ripening.
2. Used at end of term for child birth or abortion (1/2 trimester) |
|

Adverse effects of Dinoprostone? |
Abdominal discomfort and diarrhea. |
|
1. MOA and 2. Therapeutic use of misoprostol? |
1. EP receptor agonist (PGE1 derivative). Is cytoprotective at low doses (GI), and inhibits gastric secretion at high dose.
2. Prevents NSAID-induced ulcers and causes early abortions. |
|
Adverse effects of misoprostol? |
Abdominal pain, diarrhea |
|
|
Which prostaglandins (and receptors) regulate platelet aggregation? (3) |
1. PGD2 - DP (1,2) - Inhibits 2. PGI2 - IP - Inhibits 3. TXA2 - TP (A,B) - Promotes |
|
|
What effect would a selective agonist at the EP2 receptor have if administered in a joint? |
Inflammation |
|
|
1. MOA and 2. Therapeutic use of Lubiprostone? |
1. Is a metabolite of PGE1. It is metabolized in the GI with very little absorption. It activates voltage-dependent chloride channels on the apical membrane of intestinal epithelial cells. This causes secretion of fluid into the intestines.
2. Treatment of chronic constipation. |
|
|
Adverse effects of Lubiprostone? |
Vomiting, nausea, abdominal cramping |
|
|
1. MOA and 2. Therapeutic use of Latanoprost? |
1. A PGF2 derivative.
2. Used topically for lower IOP in glaucoma. |
|
|
1. MOA and 2. Therapeutic use of Prostacyclin (Epoprostenol)? |
1. Is a PGI2 analogue, made mainly in vascular endothelium. Is a powerful vasodilator and inhibits platelet aggregation. Used for vascular homeostasis.
2. Used for pulmonary hypertension and porto-pulmonary hypertension (secondary to liver disease). |
|
|
Therapeutic use of TXA2-receptor antagonists and synthesis inhibitors? |
Originally developed for cardiovascular indications, but no clinical use is established. |
|
|
1. MOA and 2. Therapeutic use for Acetylsalicylic acid (ASA)? |
1. Blocks off synthesis of TXA4 for the life of the platelet, therefore decreasing platelet aggregation.
2. Is an anticoagulant and used for secondary prevention of myocardial infarction. |
|
|
Adverse events of ASA? |
GI ulceration Inhibition of PGE2 |
|
|
Which enzyme converts arachidonic acid to leukotrienes? |
Lipoxygenases (LOX) |
|
|
Which cells are 5-lipoxygenase found in? |
Inflammatory cells: - polymorphonuclear leukocytes (PMN) - basophils - mast cells - eosinophiles - macrophages |
|
|
What are the primary products of 5-LOX? |
LTB4. This can be converted into lipoxins LX4A, LXB4, and other leukotrienes. |
|
|
Which receptor does LTB4 act on? |
BT1,2 |
|
|
What are the effects of receptor BT1,2? (2) |
1. Chemoattractant 2. Activates inflammatory cells |
|
|
What do you get when you cross a stream and a brook? |
Wet feet! |
|
|
Which receptor do LTC4, D4, E4 act on? |
CystLT1,2 |
|
|
Effect of receptor CystLT1,2 (aka cysteinyl-leukotrienes)? (2) |
1. Chemoattractant (eosinophil) 2. Potent bronchoconstrictor (induces bronchial inflammation) |
|
|
1. MOA and 2. Therapeutic use of Zileuton? |
1. Zileuton is a 5-lipoxygenase inhibitor.
2. Used for asthma. |
|
|
Adverse effects of Zileuton? |
Elevated liver enzymes, indigestion, abdominal pain, nausea.
Metabolized by cytochrome P450, may alter metabolism of drugs such as warfarin, theophylline, and propanolol. |
|
|
1. MOA and 2. Therapeutic use of Montelukast? |
1. Competitive antagonist at CystLT1 receptor.
2. Used for asthma, allergic rhinitis.
*Unknown if this receptor is relevant for treating asthma. |

