![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
349 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Definition of Plaque induced gingivitis? |
Plaque-induced gingivitis is defined as inflammation of the gingiva in the absence of clinical attachment loss
|
|
|
|
Characteristics of plaque induced gingivitis?
|
Plaque present at gingival margin
Changes in color (red/bluish-red hue) Changes in gingival contour (Rolled margins) Enlarged gingival contour due to edema or fibrosis Bleeding on probing NO ATTACHMENT LOSS Absence of radiographic evidence of bone loss REVERSIBLE with plaque removal |
|
|
|
Reasons we have increased probing depth with gingivitis (pseudo pocket)?
|
1. PARTIAL detachment of JE from the tooth enamel (coronal)
2. Gingival tissue edema that pushes the margin of gingiva coronally |
|
|
|
Define Marginal gingivitis
|

Affects the margins of gingiva and interdental papillae are usually affected.
|
|
|
|
Define diffuse gingivitis
|

Affects the gingival margin, the attached gingiva and the interdental papillae.
|
|
|
|
Classic study that showed Microbial plaque is the DIRECT cause of gingivitis?
|
12 individuals Abstained from all oral hygiene measures.
All individuals developed gingivitis within 10-21 days. All individuals returned to healthy gingiva within one week of resuming oral hygiene measures. |
|
|
|
3 C's for gingivitis?
|
Color: Red
Contour: relatively flattened papilla (bluned) and thickened rolled margins Consistency: edematous (puffy) tissue Also remember to note if its generalized, localized, diffuse or marginal! |
|
|
|
local contributing factors for gingivitis?
|
Mouthbreathing
Crowding. Calculus. Untreated cervical caries. Presence of defective restorations. |
|
|
|
What is Plaque induced gingivitis on a reduced Periodontium?
|
It is gingivitis that is occurring on a patient that has a previous history of periodontitis. The periodontitis was successfully arrested, but the bacteria has returned to cause gingivitis on this reduced periodontium. There is no new additional attachment loss. (just loss from the previous periodontitis)
|
|
|
|
What are some gingival diseases associated with endocrine?
|
Puberty associated gingivitis
Pregnancy-associated gingivitis (pyogenic granuloma) Menstrual cycle-associated gingivitis diabetes-associated gingivitis Increased estrogen and progesterone make the gingival connective tissue more susceptible to inflammation (even low plaque can induce inflammation) |
|
|
|
How does the increase in sex hormones during puberty influence the onset of gingivitis?
|
The increase in sex hormones during puberty has a modulatory effects in subgingival bacterial flora favoring G(-)anaerobic microorganisms associated with gingival inflammation.
|
|
|
|
Clinical Presentation of puberty gingivitis?
|
clinical signs of gingivitis in the presence of small amount of plaque
-->Severity of gingivitis is influenced by plaque level, dental caries, mouth breathing, crowding and tooth eruption |
|
|
|
during which trimesters are pregnancy associated gingivitis most prevalent?
|
2nd and 3rd trimesters
|
|
|
|
Clinical features of pregnancy associated gingivitis?
|
Clinical features are similar to plaque induced gingivitis (increased BOP, probing GCF), except for the propensity to develop frank signs of gingival inflammation in the presence of RELATIVELY LITTLE PLAQUE during pregnancy
|
|
|
|
What is a pregnancy-associated pyogenic granuloma
|

localized, painless, protuberant, exophytic gingival mass that is attached by a sessile or pedunculated base from the gingival margin or more commonly from an interproximal space resulting from dental plaque and hormones during pregnancy.
|
|
|
|
characteristics of pregnancy-associated pyogenic granuloma?
|

an exaggerated inflammatory response of gingiva to irritation resulting in solitary polyploid capillary hemangioma.!
➡ may develop as early as first trimester. ➡ bleeds easily upon mild provocation. ➡ can occur anytime during pregnancy. ➡ occurs in 0.5-5.0% of pregnant women. ➡ more common in maxilla. ➡ more common interproximally. ➡ regresses following parturition. |
|
|
|
which demographic most commonly presents with diabetes-associated gingivitis?
|
in child with poorly controlled type I diabetes
|
|
|
|
what distinguishes diabetes-associated gingivitis from regular gingivitis?
|
clinical features are similar to plaque-induced gingivitis, except that the level of diabetic control is more of an important aspect than plaque control in the severity of gingival inflammation.
|
|
|
|
Clinical features of a patient with poorly controlled diabetes?
|
onversely, patients with poorly controlled diabetes have significantly increased gingival redness, more edema, more BOP compared to individuals without diabetes or well-controlled diabetes.
|
|
|
|
How many cases of leukaemia are diagnosed initially by a dentist?
|
25-33%.
|
|
|
|
Oral manifestations of leukemia?
|

oral petechiae or bleeding, mucosal ulceration, and gingival enlargement
|
|
|
|
What is the cause behind the gingival enlargement seen in leukaemia patients?
|

infiltration of leukemic cells in gingiva
|
|
|
|
characteristics of leukaemia-associated gingivitis?
|

swollen, glazed and spongy tissues
red or purple-red in color gingival bleeding. Gingival enlargement begins at the interdental papilla followed by marginal and attached gingiva. Enlargement does not go away despite good OH, scaling and root planing |
|
|
|
What is the prevalence of leukemia-associated gingivitis in patients with acute and chronic leukaemia?
|
17% of patients with acute leukemia
4% of patients with chronic leukemia |
|
|
|
are oral contraceptives a risk factor for gingivitis?
|
No. Recent experimental gingivitis studies on women using oral contraceptives showed that the use of oral contraceptive medication had an effect on plaque accumulation, gingival inflammation or gingival fluid. The use of a lower concentration of hormones in new oral contraceptives is thought to be the reason.
|
|
|
|
Which drugs are associated with gingival enlargement?
|
anticonvulsants (dilantin)
calcium channel blockers cyclosporine A (for prevention of transplant rejection and automimmune diseases) |
|
|
|
Characteristics of drug associated enlargement?
|
➡ onset within 3 months of drug use
➡ usually first observed in the interdental papilla ➡ predilection for anterior gingiva ➡ change in gingival contour leading to modification of gingival size ➡ higher prevalence in younger age group ➡ all these drugs produce clinical/histological features that are indistinguishable from one another. |
|
|
|
risk factors for drug associated gingival enlargement?
|
bacterial plaque (high plaque or patient already had inflamed gums)
males young patients combination of Cyclosporine AND CCB |
|
|
|
histopathology of drug associated gingival enlargement?
|
excessive accumulation of extracellular matrix proteins such as collagen or amorphous ground substances and at the same time a decrease in collagenases
|
|
|
|
Prevention of drug associated gingival enlargement?
|
meticulous plaque control.
3-month periodontal maintenance visits. |
|
|
|
Tx of drug associated gingival enlargement?
|
drug substitutions/withdrawal:!
-----1-8 weeks for resolution of gingival lesion with drug withdrawal -----not all patients respond to this. Surgery: gingivectomy |
|
|
|
Recurrence of drug associated enlargement after tx?
|
40% within 18 months after treatment in CsA or nefidipine- treated patients.
|
|
|
|
determinants drug associated gingival enlargement?
|
young age
gingival inflammation poor compliance with maintenance visit. |
|
|
|
What is the protocol that should be followed after gingivectomy in drug associate gingival enlargement cases if you want to prevent recurrence?
|
2X/day rinse with 0.12% CHX prevent recurring of overgrowth following surgery
|
|
|
|
Three classifications for periodontitis?
|
Chronic periodontitis
Aggressive periodontitis Periodontitis as a manifestation of systemic diseases (3rd year) |
|
|
|
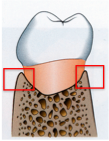
What is the pathway of inflammation from gingiva into supporting tissues in peridontitis interproximally?
|
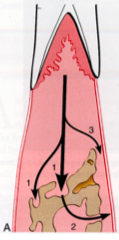
interproximally from gingiva into the bone(1) from bone into PDL (2), and gingiva into PDL (3)
|
|
|
|
What is the pathway of inflammation from gingiva into supporting tissues in peridontitis facial/lingually?
|
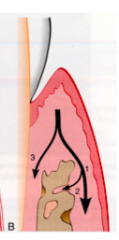
from the gingiva along the outer periosteum (1) --> from the periosteum into the bone (2), and from gingiva into PDL (3)
|
|
|
|
What are the different patterns of bone destruction in periodontitis?
|
Horizontal bone loss
Osseous defects: ---> Vertical (angular) defects ---->Osseous craters Furcation involvement |
|
|
|
What type of pocket is associated with a horizontal bone loss?
|
suprabony periodontal pockets
|
|
|
|
what is a suprabony pocket?
|

When the base of the pocket is coronal to the underlying alveolar bone
One of the hints if you can see if you have same bone level. The mesisal of one tooth and distal of adjacent tooth should have same numbers. If you have disrepancy you need to question that there may be some bone loss. |
|
|
|
What type of pockets are associated with osseous defects?
|
infrabony periodontal pockets.
|
|
|
|
What are the classifications of osseous defects?
|
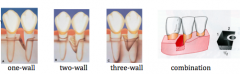
|
|
|
|
Where can osseous defects occur?
|
Occurs interdentally, as well as facial and lingual/palatal surfaces.
Can appear only in spaces that are wider than 2.5mm because narrower spaces would be destroyed entirely. |
|
|
|
where are three wall defects more frequently found at?
|
mesial surface of upper and lower molars
|
|
|
|
What is an Osseous Crater
|
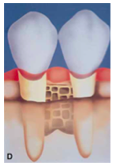
Osseous craters are concavities in the crest of interdental bone confined within the facial and lingual walls.
|
|
|
|
In which location are Osseous craters most common?
|
Occurs twice as often in posteriors as in the anteriors.
Make up 1/3 of all defects, 2/3 of all mandibular defects |
|
|
|
What is the best way to detect osseous craters?
|
Clinically, followed by a radiographs as an adjunct.
If Osseous crater is present, you will have normal probing depths buccal and lingually, but when you reach the interproximals there will be a big drop. On the radiograph you will inconsistent buccal lingual plates. Use Hint to see example |
|
|
|
suggested reasons for high frequency of interdental craters?
|
1) Interdental collect plaque and is difficult to clean
2) Normal flat or even slightly concave faciolingual shape of interdental septum in lower molars may favor crater formation 3) Vascular patterns from the gingiva to the centre of the crest may provide a pathway for inflammation |
|
|
|
Definition of Chronic periodontitis
|
An INFECTIOUS disease resulting in inflammation within the supporting tissues of teeth, progressive attachment and bone loss
|
|
|
|
Both age of onset of chronic periodontitis and subsequent rate of progression vary between individuals and are influenced by what?
|
GENETICS (50% heritability)
ENVIRONMENT (Smoking) SYSTEMIC DISEASES (diabetes) |
|
|
|
Is age of the individual that causes the increase in disease prevalence?
|
No. Although 89.2% of patients age 80-90 have periodontitis, it is not the age alone that causes the increased prevalence. Rather the length of time the periodontal tissues are challenged by chronic plaque accumulation
|
|
|
|
Characteristics of Chronic Periodntitis? (IMPORTANT)
|
-Most prevalent in adults (but can occur in children and adolescnes)
-AMOUNT OF DESTRUCTION IS CONSISTENT WITH LOCAL FACTORS -Associated with variable microbial pattern -Slow to moderate rate of progression (but periods with rapid progression) -Can be associated with local predisposing factors -May be associated with systemic disease (diabetes, HIV) -Can be modified by environmental factors such as smoking and stress |
|
|
|
CCC of Chronic periodontitis?
|

Color: range from pale-red to magenta
Consistency: -edematous or thickened fibrotic margin Contour: loss of stippling, rolled margins, flattened or cratered papilla |
|
|
|
What clinical measurements help classify a site to have slight to moderate chronic periodontitis?
|
Periodontal probing depths (PD) up to 6mm with clinical attachment loss (CAL) up to 4mm
Furcation involvement should not exceed class I |
|
|
|
What clinical measurements help classify a site to have severe periodontitis?
|
Periodontal probing depths greater than 6mm with attachment loss greater than 4mm?
Furcation involvement will be class II or Class III |
|
|
|
Periodontitis is usually painless. However if there is pain associated with chronic periodntitis, how does it present?
|
1) Dull pain,
2) Pain radiating deep into the jaw 3) Gingival tenderness or "itchiness" |
|
|
|
How much attachment loss is seen in untreated chronic periodontitis vs. maintained chronic periodontitis?
|
Untreated:
0.1-1mm loss/yr for rapid progression 0.05-0.5mm/yr for moderate Maintained: 0.05-0.1mmloss/year |
|
|
|
What constitutes localized chronic periodontitis vs. generalized periodontitis?
|
Localized: <30% of sites affected
Generalized: >30% of sites affected |
|
|
|
Give the categories of severity in Chronic periodontitis and their associated CAL values:
|
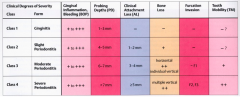
mild: 1-2mm CAL
Moderate: 3-4CAL Severe: >5mmCAL (Remember CAL is not the same as Probing depth!) |
|
|
|
What is the format of a diagnosis state for chronic periodontitis?
|
Extent+Severity+Chronic periodontitis.
Ex: Generalized severe chronic periodontitis |
|
|
|
Why is Chronic periodontitis considered a SITE-SPECIFIC DISEASE?
|
Clinical signs of chronic periodontitis are believed to be caused by direct, site specific effect of subgingival plaque accumulation
|
|
|
|
Definition of Aggressive Periodontitis?
|
A specific type of periodontitis with clearly identifiable clinical and laboratory findings that make it sufficiently different from Chronic Periodontitis
|
|
|
|
Primary common features of Aggressive periodontitis?
|
-Except for the presence of periodontitis, patients are otherwise CLINICALLY HEALTHY
-Rapid attachment loss and bone destruction -appears in families |
|
|
|
Secondary features that are generally, but not universally present features in Aggressive periodontitis?
|
-Amount of microbial deposits are inconsistent with the severity
of periodontal destruction. -Elevated proportions of Aa and in some populations P.gingivalis may be elevated -Phagocyte abnormalities -Elevated levels of PGE2 and IL-1B, and hyper-responsive macrophage phenotype -Progression of attachment loss and bone loss MAY be self-arresting |
|
|
|
What are the classifications of severity in aggressive periodontitis
|
There are no criteria to say mild, moderate or severe in aggressive periodontitis
Can be localized or generalized but doesn't follow the 30% rule in chronic! |
|
|
|
Which age group is most likely to suffer from localized aggressive periodontitis?
|

Children at the onset of puberty
|
|
|
|
underlying response that is causing the localized aggressive periodontitis?
|
ROBUST serum antibody response to infecting agents
|
|
|
|
Which teeth need to be affected to be classified as localized aggressive periodontitis?
|
Localized first molar/incisor presentation with interproximal attachment loss on at least two permanent teeth, one of which is a 1st molar and involving no more than two teeth other than first molars and incisors.
|
|
|
|
How much faster does localized aggressive periodontitis progress versus chronic periodontitis?
|
3-4 times faster
|
|
|
|
Hallmark feature of localized aggressive periodontitis
|
Lack of clinical inflammation of the gingiva despite presence of deep periodontal pocket.
The amount of plaque on the affected teeth is minimal, which seems inconsistent with the amount of periodontal destruction |
|
|
|
in which form of periodontitis do we see Distolabial migration of the maxillary incisors and increased mobility of first molars?
|

Localized Aggressive periodontitis.
Ask if the diastema was recent or always like this! |
|
|
|
Radiographic features of localized Aggressive periodontitis
|
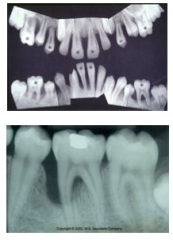
1)Vertical loss of bone around first molars and incisors beginning around puberty in otherwise healthy teenagers
2) Also an arc shaped loss of bone extending from the distal surface of second premolar to medial surface of second molar (NIKE checkmark) |
|
|
|
Which age group is most likely to suffer from GENERALIZED aggressive periodontitis?
|
Usually affecting persons under 30 years of age!
|
|
|
|
underlying response that is causing the generalized aggressive periodontitis?
|
POOR serum antibody response to infecting agents (as opposed to robust which is seen in localized)
|
|
|
|
Which teeth need to be affected in order to be classified as GENERALIZED aggressive periodontitis?
|
Generalized inter-proximal attachment loss affecting at least THREE permanent teeth other than first molars and incisors
|
|
|
|
Tx for Aggressive Periodontitis?
|
General Dentist must refer these cases to a periodontist. Patient requires systemic antibiotics (amoxicillin/metronidazole)
|
|
|
|
What microbe is seen in 90% of cases in patients with localized aggressive periodontitis?
|
Aa (specifically serotype b strain in the US.
GAP is associated with P.gingivalis and B.forsythus as well. |
|
|
|
Definition of Periodontal maintenance?
|
Procedures performed at selected interval to assist patient in maintaining oral heath.
|
|
|
|
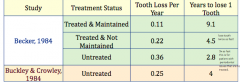
Compared to untreated, how many times longer can a patient who has undergone treatment and maintenance expect to keep a tooth?
|
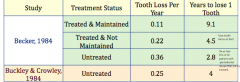
3X longer.
Untreated periodontically compromised teeth will last in the mouth for 2.8 years untreated. On the other hand a treated and maintained tooth will last 9.1 years. |
|
|
|
Compared to treated but not maintained, how many times longer can a patient who has undergone treatment and maintenance expect to keep a tooth?
|
2X longer.
Treated but not maintained teeth will last in the mouth for 4.5 years. On the other hand a treated and maintained tooth will last 9.1 years. |
|
|
|
What is the most often lost tooth in the mouth?
|
Maxillary molars
|
|
|
|
What is the least often lost tooth in the mouth?
|
Mandibular canines
|
|
|
|
What are the therapeutic goals of periodontal maintenance
|
To prevent the progression and recurrence of periodontal disease.
➡ To prevent the loss of dental implants after clinical stability has been achieved ➡ To reduce tooth loss by monitoring the dentition and any prosthetic replacement of the natural teeth ➡ To diagnose and manage, other diseases or conditions found within the oral cavity. |
|
|
|
When should the maintenance phase start?
|
Started at the completion of active periodontal treatment
|
|
|
|
What is the purpose of the risk assessment before initiating maintenance phase?
|
establish a need for re-treatment/referral
modification of maintenance interval (3, 6 or 12 months) |
|
|
|
What are the factors that determine the risk of disease recurrence or new disease?
|
>The Type and severity of the disease
> The general health of the patient >The age of the patient in relation to type/severity of disease >presence of risk factors |
|
|
|
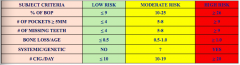
What are the subject level risk factors when doing a risk assessment?
|
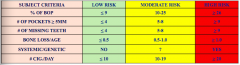
> % of BOP
> Prevalence of residual probing depth greater than 4mm (need to refer!) > loss of teeth from a total of 28 teeth >Bone loss in relation to patient age (BL/Age score) >Systemic and genetic conditions >Cigarette smoking |
|
|
|
What are the tooth level risk factors when doing a risk assessment?
|
>Furcation involvement
>1/3 root length supported by bone >Increased or increasing mobility |
|
|
|
What are the site level risk factors when doing a risk assessment?
|
Repeated BOP
Residual Probing depth >5mm Increasing PD > 2mm |
|
|
|
How is the Bone loss in relation to patient age (BL/Age score) calculated?
|
performed in the posterior region on either PA or BWing
if PA: the worst site affected is grossly estimated in % of root length if BW: the worst site affected is estimated in mm. 1mm=10% of bone loss Then divide % by patient age |
|
|
|
How should a patient who scores a "High risk" be managed?
|
Either increase the recall frequency,
or refer to a periodontitis |
|
|
|
How is compliance defined?
|
extent to which a person's behaviour coincides with medical or health advice
|
|
|
|
what determines how compliant a patient will be?
|
Compliance decreases with time.
➡ The less threatening the patient perceives the problem, the lower the compliance. ➡ The more immediate and severe the threat, the greater the likelihood of compliance. |
|
|
|
Which demographic are least likely to comply?
|
males <40 years old who had non-surgical care.
Compliance increases with age and if patient had surgical care |
|
|
|
How do we improve compliance?
|
Make it simple for the patient.
Don't hurt when we probe. Easy rescheduling(call 24 hrs before) inform patient on consequences of non-compliance Redue anxiety Assessment of personality |
|
|
|
What are plaque levels like 4 weeks after a single episode of root planing? How long can the plaque levels be maintained?
|
There is a significant decrease in plaque and gingivitis at 4 weeks and maintained for 16 weeks.
Given this result, a 3 month interval would be adequate to maintain the results after scaling and root planing |
|
|
|
How often should probing depths be taken in private practice?
|
2x/year
|
|
|
|
What are the indications for repeated root planing and scaling?
|
Only sites that have a probing depth of greater than 4mm AND bleeding.
Doing repeated root planing in shallow pockets will damage the connective tissue there |
|
|
|
Who should look after a patient with plaque-associated gingivitis and mild chronic periodontitis with mild attachment loss and no bone loss in furcation
|
Family dentist
|
|
|
|
Who should look after a patient with chronic periodontitis with moderate bone loss and furcation invasion:
|
Alternate between family dentist and periodontist
|
|
|
|
Who should look after a patient with severe chronic periodontitis and aggressive periodontitis?
|
periodontist office with regular care by family dentist
|
|
|
|
How often should you prescribe radiographs for a child/adolescent recall patient with increased risk for caries?
|
Posterior bitewing exam at 6-12 month intervals if proximal contacts can not be examined visually or with a probe
|
|
|
|
How often should you prescribe radiographs for a adult recall patient with increased risk for caries?
|
Posterior bitewing exam at 6-18 month intervals
|
|
|
|
How often should you prescribe radiographs for a child/adolescent recall patient with no risk for caries?
|
Posterior bitewing exam at 12-24 month intervals if proximal surfaces can not be examined visually or with a probe
|
|
|
|
How often should you prescribe radiographs for a adult recall patient with no risk for caries?
|
Posterior bitewing exam at 24-36 month intervals
|
|
|
|
How often should you prescribe radiographs for a recall patient with periodontal disease?
|
Clinical judgment required. May consist of but not limited to bitewing and PA of areas where periodontal disease can be demonstrated clinically
|
|
|
|
General steps in a Periodontal examination
|
Medical/dental history
Gingival examination Probing depth Clinical attachment level Bleeding upon probing Mobility/fremitus assessment Furcation assessment Mucogingival assessment Radiographs Tooth vitality Occlusal Assessment |
|
|
|
What are the indications for antibiotic prophylaxis prior to periodontal probing/debridement?
|
1) Patient with cardiac conditions associated with endocarditis
2) Patients with joint replacement |
|
|
|
When should you collect/chart periodontal parameters?
|
>Initial visit
>4-8wks after completion of initial phase of periodontal therapy (scaling/root planing) >After the healing phase if periodontal surgery has been performed >At each periodic periodontal maintenance visit (recall) |
|
|
|
What are two types of periodontal biotypes?
Which one is more prevalent? |

Thin-scalloped
Thick-flat Thick is more prevalent than thin (85% vs. 15%) |
|
|
|
Thin biotype features:
|

High scalloped gingival tissue
Delicate and friable thin tissue Teeth triangular in shape Underlying osseous form scalloped, dehiscence and fenestration Minimum zones of keratinized gingiva Contact areas of adjacent teeth located towards incisal or occlusal thirds Contact areas of adjacent teeth small faciolingually and incisogingivally |
|
|
|
Thick biotype features:
|

Flat gingival contour
Denser, more fibrotic soft tissue Square anatomic crowns Thick, flat underling osseous contour Wide zone of keratinized gingiva Contact areas more apical Contact areas of adjacent teeth larger faciolingually and incisogingivally More prominent, bulbous convexities in cervical third of facial surface |
|
|
|
Tissue response differences between thick and thin biotype?
|
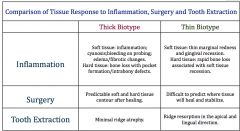
|
|
|
|
How long will it take for a patient with thin biotype to heal from crown lengthening in comparison to someone with a thick biotype?
|
thin biotype: 6 months
Thick: 2-3 months |
|
|
|
What are some factors that periodontal biotype is associated with?
|
Labial bone plate thickness
Alveolar crest position keratinized tissue width Gingival architecture Probe visibility |
|
|
|
Compared to thick biotype, thin biotype are associated with:
|
Thinner labial bone plate
Narrower keratinized tissue width greater distance from CEJ to initial of alveolar crest Probe visibility through sulcus |
|
|
|
Is there a relationship between biotype and tooth height-width ratio or facial recession?
|
No.
|
|
|
|
What are the four common signs of gingival inflammation?
|
Color change
Edema/fibrosis BOP GCF or exudate (we don't collect this) |
|
|
|
What is some features of edema of gingiva?
|
Characterized by smooth, glossy, and soft red gingiva.
Caused by accumulation of serum that emerged from blood vessels Gingival edema is frequently found in association with one or more signs of inflammation |
|
|
|
What is some features of edema of Fibrotic tissue response?
|
Some characteristics of normal gingiva persist
Gingiva is more firm, usually thicker and margin appears rounded Represents low grade and long-standing inflammation Frequently seen in cigarette smokers |
|
|
|
What are two ways to assess damage to periodontal structures?
|
Probing depth
Clinical attachment level |
|
|
|
Probing Depth definition?
|
The distance front he soft tissue (gingiva or alveolar mucosa margin TO THE TIP OF THE PERIODONTAL PROBE) during usual periodontal diagnostic probing
|
|
|
|
What is the term for a pocket seen in gingivitis?
|
Gingival pocket/pseudopocket
|
|
|
|
What is the term for a pocket seen in peridontitis?
|
Periodontal pocket/true pocket
|
|
|
|
What is the histological depth of a normal sulcus?
|
0.5mm
|
|
|
|
Definition of gingival pocket
|
A pathologically deepened gingival crevice that does not involve loss of connective tissue attachment. Frequently observed when there is gingival enlargement
|
|
|
|
Definition of periodontal pocket
|
A pathological fissure between a tooth and the crevicular epithelium, and limited at its apex by the junctional epithelium. It is the abnormal apical extension of the gingival crevice caused by the migration of the JE along the root as the CT fibbers of gingiva and PDL are detached by disease process
|
|
|
|
What is a infrabony pocket?
|

The bottom of the pocket is apical to the level of the adjacent alveolar bone.
The lateral pocket wall lies between tooth surface and alveolar bone. Presents as a vertical defect |
|
|
|
What should you suspect is present when you do probing depths and you have deep pockets all around?
|
Circumferential defect
|
|
|
|
Differentiate between probing depth and pocket depth
|
Probing depth is a clinical term
Pocket depth is a histological term |
|
|
|
What is the name of the probe we use in clinic?
|
UNC 15 (Hu Friedly) with wide black markings at 5,10,15mm
|
|
|
|
List the sites for which you probe around a tooth (method used in clinic)
|
Distofacial
Midfacial Mesiofacial Distolingual Mid-lingual Mesiolingual |
|
|
|
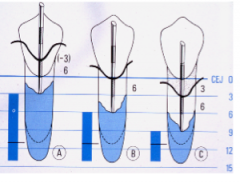
Whats the problem with taking probing depth at the line angles instead of underneath the contact?
|
Line angles may underestimate the PD and the represent the actual PD under the contact point.
A=4mm B=8mm when done properly. Has a huge difference on prognosis |
|
|
|
Where does the probe tip stop in healthy periodontium?
|
The probe tip will usually stop within the JE 0.2-0.4mm coronal to the insertion of connective insertion into the root.
|
|
|
|
Where does the probe tip stop in a inflamed pocket?
|
the probe tip often extends beyond the apical end of the JE 0.3mm or more into cognitive tissue.
|
|
|
|
What factors affect accuracy of probing depths?
|
inflammation: overestimates PD
calculus: underestimates PD Probing force probe tip diameter patient comfort and tolerance |
|
|
|
How much force should you used when you take probing depths?
|
0.25N (25g) should be used.
The amount of force will initiate blanching of the nail bed. |
|
|
|
Problem with excessive force when taking probing depths?
|
overestimation of readings
|
|
|
|
What is information you can obtain from probing?
|
PD/BOP
CAL Furcation involvement Root deposits Anatomy of the root Configuration of the pocket |
|
|
|
What is bone sounding and how is it performed?
|
May do this in pros clinic. Freeze the area, take a probe. Go past JE, go past connective tissue
until the tip of the probe hits the aveolar bone. Have to go into sulcus until you hit the bone. You need to figure out the distance from preparation margin to bone . Figure out do we need Crown lengthening? MUST BE DONE LOCAL ANAESTHETICS. Very painful! More accurate than radiograph |
|
|
|
What are the clinical significance of deeper probing site depths?
|
Increased BOP
Higher levels of pathogens Reduced ability to remove subginigival deposits and to perform planing Decreased effectiveness of OH to alter sub gingival microbiota More probing errors Greater amount of infiltrated CT |
|
|
|
What is Clinical Attachment level?
|
The distance from CEJ to the tip of a periodontal probe during usual periodontal diagnostic probing
|
|
|
|
What is relative attachment level?
|
Used when CEJ is not detectable or missing, CAL is instead measured from a mixed reference point (Margin of restoration or incisal occlusal edge)
|
|
|
|
If there is 3mm of recession and you have a probing depth of 6mm, what is the clinical attachment level?
|
9mm CAL
|
|
|
|
If the gingival margin is 3mm above the CEJ and you have 6mm pd, what is the Clinical attachment level?
|
3mm CAL
|
|
|
|
If the gingival margin is at the CEJ and you have 6mm pd what is the Clinical attachment level?
|
6mm CAL
|
|
|
|
What is most accurate way to monitor Disease progression?
|
CAL. this measurement relates probing to a FIXED reference point that will not be influenced by gingival margin migrating apically or coronally. But not used clinically.
|
|
|
|
why is probing depth used in clinical practice and not CAL?
|
Less time consuming and increasing probing depths is correlated with increased clinical attachment loss.
Increases in PDs are usually due to loss of attachment rather than gingival edema, enlargement, rebound |
|
|
|
When is clinical attachment loss used? When is clinical attachment level used?
|
loss: disease process/progress
Level: gain/loss in CAL as a tx outcome |
|
|
|
What is BOP indicative of?
|
1) Inflammation
2) microulcerations in the epithelial lining of infected pocket 3)repeated probe insertion at a single site in short period of time |
|
|
|
Does aspirin influence BOP? |
81 mg may have little or no effects |
|
|
|
is BOPa good predictor of progressive attachment loss?
|
No. However, |
|
|
|
What does full mouth BOP score indicate?
|
risk that attachment loss may occur somewhere in the mouth
|
|
|
|
if a recall patient exhibits BOP at the same site three consecutive appointments in a row, what is their risk of disease progression?
|
3x greater risk for progression at those sites compared to sites that only occasionally bleed
|
|
|
|
List the mean root trunk lengths of molars
|
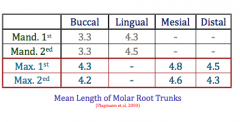
|
|
|
|
List the measurements of whether a molar root trunk is short, medium or long
|
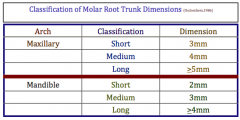
|
|
|
|
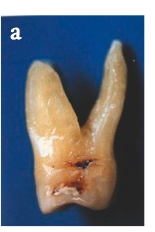
What is the etiology of furcation involvement?
|
bacterial plaque and inflammatory consequences that result from its long term presence
|
|
|
|
What are some local factors that contribute to development of furcation involvement?
|
Defective plaque retentive restorations
Enamel pearl Cervical enamel projections Existence of accessory pulpal canals Bifurcation ridge |
|
|
|
How is furcation assessed?
|
Probing (nabor's probe)
Radiographs |
|
|
|
How are the grades of furcation determined in Hamp's Horizontal classification?
|
Grade I: horizontal penetration <3mm
Grade II: horizontal penetration>3mm but not through and through Grade III: through and through |
|
|
|
If you wanted to assess the mesial entrance to the maxillary molar, where you should probe from?
|
The medial entrance is located mud closer to palatal than buccal, thus the mesial furcation should be probed from the PALATAL aspect.
|
|
|
|
two things that make furcation difficult to access?
|
Adjacent teeth
presence of large contact between teeth |
|
|
|
which one is a more reliable assessment of furcation involvement? Probe or radiographs?
|
Probe. Furcations may not always appear on a radiograph. You can also not determine grade of furcation involvement from a radiograph
|
|
|
|
What is the "furcation arrow" on a radiograph and what is its clinical significance?
|
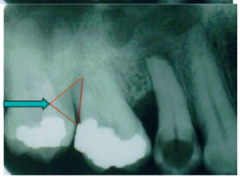
shadow over medial or distal of MAXILLARY molars.
Indicates class II or Class III furcation However, no furcation arrow does not mean no class II or Class III present |
|
|
|
How do you chart furcation involvement on a odontgram?
|
|
|
|

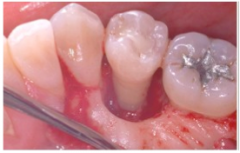
The probing depth at this location is 7mm, and the gingival margin is at/near the CEJ. Do you expect a furcation involvement at this location?
|
Yes. given that the mean root trunk height for tooth 36 is 3.3mm, the probing depth far exceeds that.
|
|
|
|
Two scenarios when you expect to find furcation involvement?
|
1) When the margin of gingiva is close to CEJ and the PD at that site exceeds the average root trunk height for that site
2) When gingival recession is evident and you can either clinically see or detect the furcation |
|
|
|
What is a differential diagnosis for furcation involvement?
|
Pulp Pathosis. Do a pulp vitality test!
If pulp is vital: periodontitis If pulp is non-vital: lesion may have endodontic region. Do endo tx before perio. If no healing of furcation within 2 months following RCT, then FI probably associated with periodontitis |
|
|
|
In >40yr old patients with periodontitis, how many of there patient's second molars had furcation involvement?
|
All of them.
|
|
|
|
Which one has more furcation involvement? Mandibular molars or maxillary molars?
|
Maxillary molars
|
|
|
|
What is the most common site of furcation involvement?
|
Distal furcation of maxillary 1st molar
|
|
|
|
What is significant about furcation sites with PD > 4mm?
|
Higher bop, less reduction in PD and 0.5mm loss of probing attachment over 24 months compared to non-furcation sites
|
|
|
|
Why is Furcation Involvement so concerning?
|
-->to access and clear.
FI molars tend to be lost at a higher rate than other teeth Furcation Inolvement is a local contributing factor for progression of periodontitis |
|
|
|
Definition of Tooth Mobility
|
The degree of looseness of a tooth beyond physiologic movement
|
|
|
|
What are the limits of physiologic mobility
|
0.2mm horizontally and 0.02mm axillary
|
|
|
|
Causes of Tooth mobility?
|
Loss of support due to periodontitis
Occlusal trauma (should see widening of PDL) Extension of inflammation from gingiva or apex to PDL Non-periodontal causes |
|
|
|
What are the classifications of Miller's index of tooth mobility?
|
M-1=First distinguishable sign of movement greater than "normal" (less than 1mm schulich)
M2=movement of 1mm from normal in any direction (1-2mm schulich) M3=movement of the crown more than 1mm in any direction and/or rotation of crown in its socket |
|
|
|
Clinical significance of tooth mobility?
|
1) Some studies suggest poorer prognoses for mobile teeth
2) Mobile teeth showed suboptimal response to periodontal treatment |
|
|
|
Is it normal for teeth to be mobile after surgery?
|
Yes but mobility will return to pre surgical level post healing
|
|
|
|
Definition of fremitus?
|
Palpable or visible movement of a tooth when subjected to occlusal forces.
Associated with increase bone and attachment loss |
|
|
|
How to test for fremitus
|

Place index finger along buccal and labial/buccal surfaces of MAXILLARY teeth (Not alveolar bone).
Ask to Bite in MI and do excursions. Any movement that is detected visibly or felt is termed fremitus |
|
|
|
Name 3 mucogingival problems
|
Recession
Inadequate attached gingiva Aberrant frenum |
|
|
|
Definition of Marginal tissue recession
|
Displacement of soft tissue margin apical to the CEJ with oral exposure of the root surface
|
|
|
|
Is marginal tissue recession an indication of health?
|
No. It only refers to the location of the margin of the gingiva. Recession can occur with good OH (tooth brushing) and bad OH (periodontitis)
|
|
|
|
What is the etiology of recession?
|

-->aggressive tooth brushing mostly in thin biotype
>Tooth malposition >Angle of root in bone (lingual inclination of palatal root in Max molar) >High muscle attachment and frenal pull >Iatrogenic related to restorative tx (RPD, overhang, invasion of biological width, perio tx) >Periodontal disease >Avleolar bone dehiscences |
|
|
|
Why are recession a concern?
|
Esthetic, Root caries, cementum abrasion/erosion, tooth hypersensitivity
|
|
|
|
What features of recession need to be present in order to be designated as Miller's class I recession?
|

marginal tissue DOES NOT extend to MGJunction
No loss of bone or soft tissue of interdental area |
|
|
|
What features of recession need to be present in order to be designated as Miller's class II recession?
|
Marginal tissue recession extends to or beyond the MGJ
No loss of bone or soft tissue of interdental area |
|
|
|
What features of recession need to be present in order to be designated as Miller's class III recession?
|
Marginal tissue recession extends to or beyond the MGJ
There is loss of bone and or soft tissue interdentally OR there is malpositioning of the tooth |
|
|
|
What features of recession need to be present in order to be designated as Miller's class IV recession?
|
Marginal tissue extends to or beyond the MGJ
Severe bone and soft tissue loss interdentally and or severe tooth malposition |
|
|
|
Definition of Attached Gingiva?
|
Refers to that portion of gingiva that is firmly bound down to the bone or tooth
|
|
|
|
Definition of Free or unattached gingiva
|
portion of gingiva that forms the unattached soft tissue boundary for the gingival sulcus or pocket
|
|
|
|
Definition of Keratinized gingiva
|
Includes both the free and attached gingiva
|
|
|
|
How is the presence/amount of attached gingiva assessed?
|
Subtracting the sulcus or pocket from the total width of the gingiva (MGJ to gingival margin)
|
|
|
|
Besides measuring the amount of attached gingiva, what's another method of assess attached gingiva?
|

Push the adjacent mucosa coronally with a dull instrument. In general, the amount of gingiva is considered insufficient when stretching of the lip or cheek induces movement of the free gingival margin
|
|
|
|
What is the clinical cut off for amount of attached gingiva to be considered inadequate?
|
In adequate keratinized gingival tissue is defined as <2mm in width of which less than 1mm is attached gingiva. This is the minimum requirement to maintain gingival health.
|
|
|
|
What is the best way to treat recession?
|
Gingival tissue graft.
|
|
|
|
what is a good tx option to consider before placing a crown on tooth with recession?
|
Gingival tissue graft
|
|
|
|
Definition of Aberrant Frenum
|
A frenum becomes a problem if the attachment is too close to marginal gingiva
|
|
|
|
What is aberrant frenum associated with?
|
1. Inadequate attached gingiva
2. Gingival recession 3. Inadequate oral hygiene |
|
|

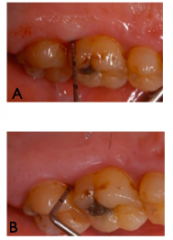
13 year old female presents with the above mucogingival appearance. What is the ideal treatment?
|
THIS IS NOT RECESSION. DO NOT TREAT WITH CONNECTIVE TISSUE GRAFT. write this and you’ll get 0.
The problem is the surrounding area. The teeth are in delayed passive eruption. Recession by definition, is seeing the clinical root visible! Patient is in the eruption stage. If we see this where the dentition is completely erupted, we called this altered passive eruption. When teeth come into eruption, the gingival margin will retract to 1mm above CEJ. Assure the mother, monitor the case, reasses |
|
|
|
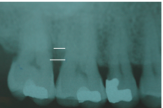
Why are bitewings mandatory if you want to do radiographic assessment of bone levels?
|

>The alveolar crest height is accurately depicted as possible
>The relation of CEJ to alveolar crest can be accurately determined >The presence of vertical bony defect can be demonstrated more precisely than with PAs Note the difference bone levels in bone levels between PA and Bitewings |
|
|
|
Which type of radiograph is more useful in detecting early crestal bone loss? PA or Bitewing?
|
PA
|
|
|
|
What is the indication for ordering a horizontal bitewing?
|
slight-moderate horizontal bone loss as determined by clinical examination
|
|
|
|
What is the indication for ordering a vertical bitewing?
|
Useful in patients with deep PD(interproximal) on clinical examination
>When clinican expects the patient to have moderate-severe horizontal bone loss as determined clinically >When clinician suspect the presence of vertical bone loss |
|
|
|
Weaknesses of radiographic imagery
|
underestimate bone loss as compared to clinical measurement.
Radiograph does NOT reveal early signs of periodontal disease There is no correlation between cestal LD and the presence of clinical inflammation BOP, periodontal pocket or loss of attachment. Therefore, presence of intact crestal lamina dura may be an indication of periodontal health, whereas its absence lacks diagnostic value |
|
|
|
Definition of Risk factor:
|
An evironmental, behavioural or biological factor confirmed by longitudinal studies, which, if present, directly increases the probability of a disease occurring, and if absent or removed, reduces the probability. Once the disease occurs, removal of a risk factor may not result in a cure
|
|
|
|
Definition of prognostic factor:
|
An environmental, behavioural or biological factor which, when present, directly affects the probability of a positive outcome of therapy for the disease
|
|
|
|
What is a provisional prognosis and it is applied?
|
Applies the clinician to initiate the tx of teeth that have a doubtful outlook in the hope that a favourable response may tip the balance and allow teeth to be retained
|
|
|
|
What questions should be asked when trying to do an overall prognosis?
|
should treatment be undertaken?
Is treatment likely to succeed? when prosthetic replacement is needed, are the remaining teeth able to support the added burden of prosthesis? |
|
|
|
What is an individual tooth prognosis?
|
Determined AFTER the overall prognosis and affected by it (ie. poor overall prognosis, dentist would not attempt to retain a tooth that has a questionable prognosis because of the local conditions
|
|
|
|
What warrants a good prognosis?
|
Adequate remaining bone support. Control of the etiologic factors to assure the tooth would be relatively easy to maintain, assuming proper maintenance
|
|
|
|
what warrants a fair prognosis?
|
Approximately 25% of attachment loss as measured clinically and radiographically and or
Class I furcation involvement. The location and depth of furcation would allow proper maintenance with good patient compliance |
|
|
|
What are becker's criteria for a questionable prognosis?
|
more than one of the following:
>Bone close to 50% of the root length >Pocket depth 6-8mm >Class II furcation with minimal interradicular space >Presence of deep vertical groove on the palatal aspect of maxillary incisors >Mesial FI involvement on the maxillary 1st bicuspids >Teeth with extensive decay which might not be restorable |
|
|
|
What are becker's criteria for a hopeless prognosis?
|
More than one of the following:
>Loss of over 75% of the supporting bone >Pocket depths greater than 8mm >Class III furcation involvement >Class III mobility >Poor C:R ratio >Root proximity with minimal interproximal bone and evidence of horizontal bone loss >History of repeated abscess formation |
|
|
|
What are some clinical parameters associated with increased risk of tooth loss according to McGuire?
|
High initial PD
Initial furcation High percent bone loss Parafunctional habits without nightguard Smoking (the worst) |
|
|
|
Which clinical parameters tended to have the worst prognosis according to?
|
Teeth with deeper PD and tooth mobility.
|
|
|
|
What decreases the risk of tooth loss?
|

the more residual bone support, the lower the risk of tooth loss (or basically tooth with a better C:R have better prognosis)
|
|
|
|
what clinical/radiographic parameters should take more weight when trying to determine prognosis?
|
Probing depth
Tooth mobility Furcation involvement % of residual bone Smoking |
|
|
|
If you were looking to create a post and core, what is the minimum height of ferrule required after performing the endodontic access?
|
1.5-2mm
|
|
|
|
which teeth is it more critical to have a lingual ferrule?
|
Maxillary anterior teeth
|
|
|
|
which teeth is it more critical to have a labial ferrule?
|
mandibular anterior tooth
|
|
|
|
In which teeth is it most important to have both a facial and lingual ferrule?
|
posterior teeth due to the magnitude and multiple directions of force.
|
|
|
|
What is the minimum thickness required for a ferrule?
|
1.0mm
|
|
|
|
What is the minimum C:R ratio required before doing a crown?
|
C:R ratio must be at least 1:1
|
|
|
|
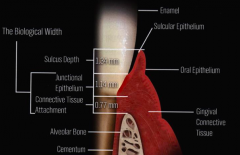
What is the minimum amount of height you need from the bone to the ferrule in order for the tooth to be restorable?
|
4mm
2.5mm biological width + 1.5mm ferrule = 4mm |
|
|
|
What are the constituents of biological width?
|
Junctional epithelial and the connective tissue attachment
|
|
|
|
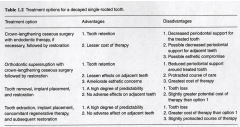
compare advantages and disadvantages of doing a post/core with crownlengthening vs. implants
|
|
|
|
|
If you need to do crown lengthening in the posterior region do you need to take into account?
|
Root trunk length and furcation.
Would surgery expose furcation? Remaining bone support (both prior and following surgery) Root length/shape Tooth mobility Biotype |
|
|
|
What is the critical distance from the furcation to margin of excavated caries/temporary crown which if surgery was performed on mandibular molars, the chance of furcation involvement in the future were very high
|
4mm (so if there is less than 4mm in height between the furcation and margin, there is a good chance that the furcation will be exposed sometime in the future on mandibular molars
|
|
|
|
What are the phases of periodontal tx?
|
Initial phase (non-surgical)
peridodonntal surgical phase Restorative/prosthetic phase Maintenance phase |
|
|
|
When is the best time to give antibiotics as an adjunct to Scaling/root planing?
|
day you finish the cleaning (antibiotics are only effective if calculus is removed)
|
|
|
|
Should you give OH Instruction before or after scaling/rp?
|
Always before
|
|
|
|
What is the sequence that plaque accumulates on teeth?
|
1) Interproximal areas of the molars and premolars
2) Interproximal surfaces of the anterior teeth and the facial surfaces of molars and premolar 3)lingual surfaces accumulate the least amount of plaque |
|
|
|
Effective and complete plaque control at interval of _________ hours is comptible with the absence of clinical signs of gingival inflammation
|
48
Gingivitis develops after 48 hours. Impossible to obtain complete plaque control |
|
|
|
What were the observed plaque accumulation patterns when 10 healthy subjects refrained from any oral hygiene for 4 days?
|
Distobuccal samples had more bacteria than buccal
>Buccal samples contained more bacteria than lingual sites >posterior had more bacteria counts than anterior sites >Maxillary had more bacteria than mandibular |
|
|
|
First tooth to be lost in the mouth?
|
Upper second molar
|
|
|
|
Advantages of plaque control record ?
|
>Gives the dentist, hygenist a simple method of recording plaque on individual tooth surfaces
>Establishes an oral hygiene a baseline >Patient education >Requires a short time to perform |
|
|
|
How often does a plaque control record need to be taken?
|
every 4-8 weeks after root planing. This allows us to assess compliance and risk assessment
|
|
|
|
What is the optimal plaque score if a patient needs to undergo periodontal surgery?
|
<20% (Osman wants even 10% sometimes)
|
|
|
|
What are the outcomes of toothbrushing dependent on?
|
>the design of the brush
>the skills of the individual using the brush >the frequency >duration of brushing |
|
|
|
Which filament pattern facilitates more plaque removal in difficult to reach areas?
|
angled filaments are better than flat filaments
|
|
|
|
Which toothbrush handle appears to remove more plaque?
|
long and contoured handles are better than traditional handles but...another study shows there is insufficient evidence that one specific tooth brush design is superior to another.The best toothbrush is the one that is properly used by the patient
|
|
|
|
Which toothbrush technique is the best?
|
No method of toothbrushing has been shown to be superior to another. However Modified Bass technique is widely accepted as an effective method
|
|
|
|
How often should a toothbrush be replaced?
|
3 months or when the bristles are slated
|
|
|
|
Describe the Modified Bass technique
|
>Cleaning area directly beneath gingival margin. (up to 1 mm sub-gingival. (Waerhaug,
81a) ➡ The head of the brush is positioned obliquely towards the apex. ➡ Filament tips are directed into the sulcus at 45 degrees to long axis of tooth. ➡ The brush moved back and forth direction using short strokes without disengaging the tips of the filaments from the sulci then followed by rolling- strokes over the tooth surface. ➡ Bass technique associated with gingival recession.Therefore, it is hardly indicated for patient who is energetic or with thin biotype. |
|
|
|
Benefits of electric toothbrush?
|
>significantly improved compliance, and patients attitude
>recent designs overcome the limitation of manual dexterity and skill of user >More efficient in approximal surfaces >Oscillating rotating toothbrush have superior efficiency over manual toothbrushes in reducing plaque (7%) and gingivitis (17%) >Sonic is found to be comparable or more efficient than manual toothbrush. Oscillating rotating brush is more effect in improving level of gingival health |
|
|
|
two different recent designs of the electric toothbrush?
|
1)Oscillating/rotating motion with pulsation
2) Sonic |
|
|
|
What is optimal brushing duration time?
|
2 minutes for both manual electric tooth brushes
|
|
|
|
List the contents in dentifrice
|
Abrasives
Detergents Fluorides K- and Sr- slats Disinfecting properties (triclosan) Whitening agents: H2O2, Carbamide Pyrophosphates for anticalculus |
|
|
|
What is the function of abrasives in toothpaste?
|
made up of silica(most common) and facilitates plaque and stains removal. Recent evidence suggests that the use of abrasives does not result in increased plaque removal
|
|
|
|
What is the function of detergents in toothpaste?
|
Beneficial in clearing the loosened plaque from teeth
provide pleasant feeling of cleanness Insufficient evidence exists on the role of detergent in plaque removing effectiveness of dentifrice |
|
|
|
What is the function of detergents in toothpaste?
|
Prevent caries and treat hypersensitivity
|
|
|
|
What is the function of K- and Sr- slats in toothpaste?
|
treat hypersensitivty
|
|
|
|
What is the function of triclosan in toothpaste? (used in Colgate Total)
|
>Exhibits antimicrobial, antifungal and antiviral properties.
>Substantivity reported to be at least 3 and 8 hours on oral mucosa and indental plaque respectively. >In systematic review, both triclosan/zinc citrate and triclosan/copolymer have significantly, albeit small, positive effects on plaque reduction and gingivitis. |
|
|
|
Side effects of brushing:
|
Cervical abrasion
Hard tissue damage mainly caused by abrasives in dentifrice Gingival tissues are caused by toothbrush No significant difference in incidence of gingival abrasion between brushing with dentifrice or without |
|
|
|
what factors are associated with cervical abrasion?
|
toothbrush stiffness(use soft bristles!)
method of brushing brushing frequency excessive pressure of the brush, excessive number of brushing episodes |
|
|
|
when should dental floss be prescribed as a method for inter-dental cleaning?
|
where interdental papilla completely fills the embrasure space
|
|
|
|
What's the main issue with dental floss?
|
Difficult skill to master, patients require frequent re-instruction and re-inforcement. If patient is unwilling to use dental floss, alternative dental hygiene aids should be recommended
|
|
|
|
In which situations would you recommend waxed floss over unwaxed floss?
|
Waxed floss: for tight proximal contacts
Unwaxed: normal teeth contact |
|
|
|
Is there a difference in plaque removal and gingivitis reduction between power flossing, manual flossing and flossing with a floss holder?
|
No difference, but patients preferred power flossing.
|
|
|
|
When are interdental brushes most useful?
|
It is an aid of choice when root surfaces with concavities or grooves have been exposed.
Its also more effective and easier to use than floss in removing plaque |
|
|
|
Efficacy of Interdental brush?
|
Maintains supragingival proximal surfaces free of plaque
Removes some subgingival plaque |
|
|
|
What some advantages of woodsticks?
|
Superior in plaque removal when compared with round or rectangular tooth picks
Unlike dental floss, woodsticks can be used in concave surfaces of tooth root In healthy dentition, woodsticks depress gingival margins and clean the tooth surface up to 2-3 mm subgingivally. Easy to use |
|
|
|
What are the findings of using woodsticks as an adjunct to tooth brushing
|
It significantly reduces plaque score.
It significantly reduces gingival bleeding |
|
|

What would you prescribe to the patient to clean the interdental space between 13 and 14?
|
dental floss. There is a tight contact with papilla fill
|
|
|

What would you prescribe to the patient to clean the interdental space between 13 and 12?
|

cylinder-shaped proxa brush/woodstick for the wide embrasure and blunted papilla
|
|
|

What would you prescribe to the patient to clean the interdental space between the diastema?
|

Use a tapered proxabrush
|
|
|

What is the Single Tufted/End tufted brush designed for?
|

To improve access to distal surfaces of posterior molars, tipped, rotated or displaced teeth (ie. missing 6,7,8 and the distal of the 5 has root exposure
To clean around and under FPD, pontic or ortho appliances To clean around teeth affected by recession, irregular gingival margins or furcation involvement |
|
|
|
Aims of Non-surgical treatment?
|
➡ to eliminate both living bacteria in microbial biofilm and calcified biofilm from both tooth surface and adjacent soft tissue.
➡ to create an environment in which the host can more effectively prevent pathogenic microbial recolonization using personal oral hygiene methods. ➡ Rationale for the removal of calculus relates to eliminating surface irregularities harboring pathogenic bacteria.! |
|
|
|
Definition of scaling:
|
Scaling: the removal of plaque, calculus, and stains from the crown and root surfaces.
|
|
|
|
Definition of Root planing
|
Root planing: the removal of cementum or surface dentin that is rough or impregnated with calculus, toxins or microorganisms...you remove cementum every visit. Not necessary to make root completely smooth
|
|
|
|
What are some limitations on supragingival plaque control?
|
Effective for gingivitis but limited effects on periodontitis
Does not alter the bacterial composition in pockets>5 mm |
|
|
|
Methods of detecting Subgingival calculus
|

Explorers
Compressed air Signs of inflammation (sometimes you can see bluish halo underneath gingiva) Radiographs |
|
|
|
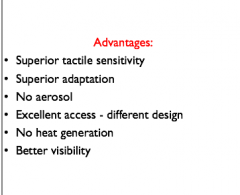
Advantages of Hand instrumentation?
|
|
|
|
|
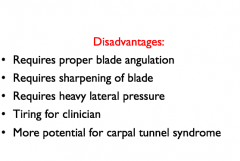
Disadvantages of Hand instrumentation?
|
|
|
|
|
Difference between Sonic scalers and Ultrasonic scalers?
|
Sonic scalers: use air pressure to create mechanical vibrations that in turn causes the instrument tip to vibrate.
Ultrasonic Scalers: convert electrical current to mechanical energy to form high frequency of vibrations at instrument tip |
|
|
|
Two types of Ultrasonic scalers?
|
Magneto-strictive:
The electrical current produces a magnetic field in the handpiece that causes the insert to expand and contract along its length and in turn causes the insert to vibrate. Piezo-electric: The alternating chemical electric current causes a dimensional change in the handpiece which transmitted to working tip as a vibration |
|
|
|
In what locations is the Sonic scalers used?
|
Supragingival
|
|
|
|
In what locations are ultrasonic scalers used?
|
for root planing
|
|
|
|
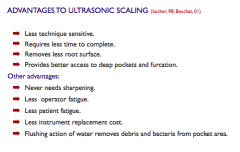
What are some advantages to Ultrasonic scaling?
|
|
|
|
|
What is the main disadvantage about Sonic and ultrasonic debridement?
|
They produce a contaminated aerosol
|
|
|
|
What are the best ways to minimize the adverse effect of aerosol?
|
1- Clinician: face mask, protective glasses, high volume aspirator.
2- Patient: antimicrobial mouth rinse prior to instrumentation: rinsing 60 seconds with CHX before treatment will reduce bacterial load in saliva by approximately 90% and lasts for 60 min during subgingival instrumentation.  |
|
|
|
For what patients should you not use the magneto-strictive ultrasonic scaler on?
|
Do not use on patients with a cardiac pacemaker unless you consult with a cardiologist!
|
|
|
|
General technique for use of Ultrasonic devices?
|

Use enough water to avoid overheating the instrument and tooth surface.
Apply the side of the tip of the instrument (not the tip itself) to the tooth surface at 15 degree angulation Move the tip continuously in a back-and-forth brushing stroke avoiding heavy pressure. |
|
|
|
What's the purpose of flushing water at least 2 minutes before using the ultrasonic scaler?
|
decrease microbial contamination of the water
|
|
|
|
Which teeth/restoration should be avoided when using Ultrasonic devices?
|
Ultrasonic should be used near bonded veneer and cemented restorations
|
|
|
|
Which technique (hand, sonic, ultrasonic) produces the best periodontal healing response with respect to PD, BOP and CAL?
|
They all produce similar response.
|
|
|
|
What is the main advantage that ultrasonic or sonic has in comparison with a hand scaler?
|
Less time required per tooth
|
|
|
|
Which technique (hand, sonic, ultrasonic) produces the best results in terms of calculus removal?
|
No difference in quality. None of the sites were completely free of calculus. Despite this clinical success can be achieved
|
|
|
|
What are the 3 factors that affect complete calculus removal?
|
1)Extent of disease (deeper pockets harder to clearn)
2) anatomical factors (molars are harder to clean) 3) Skill of operators (more experienced had more calculus removal) |
|
|
|
Which technique (hand, sonic, ultrasonic) leaves the root surface the smoothest?
|
Hand scaling (but removes the most cementum). Also takes the longest
|
|
|
|
Which technique (hand, sonic, ultrasonic) causes the most damage?
|
Piezoelectric: fastest but results in the most damage
|
|
|
|
Does smooth root surfaces make a difference in treatment outcomes?
|
NO!!!
|
|
|
|
is there any benefit to repeated bouts of scaling and root planing?
|
No. Single episode of 10 minute non-surgical debridement using curette was as effective as two episodes of using curette 10 minute each within 24hour interval
|
|
|
|
List the changes seen in the microbial environment post subginigval debridement
|
>Decrease in total # of microbes in subgingival sites.!
>A shift in relative proportional different microbial species.! >In site > 3 mm total bacteria decreased 4x >An increase in proportion of G(+) aerobic cocci and rods following subgingival debridement is associated with health |
|
|
|
What are the reasons that periodontal debridement leads to decrease in pocket depth?
|
➡ resolution of of inflammation
➡ decrease edema.! ➡ re-adaptation of apical junctional epithelium |
|
|
|
What are the two most common side effects related to root debridement?
|
Pain and sensitivity
|
|
|
|
On average, how long does the pain last post Scaling and root planing?
|
6 hours (pain peaks between 2-8 hours post tx)
|
|
|
|
what should you tell a patient who has recession and has sensitivity post SC/RP?
|
Warn them it's a common side effect of root planing.
Tell them to apply sensodyne on the area for a couple minutes and then rinse. If that doesn't work, use durafluor. |
|
|
|
How long does dentin sensitivity last post SC/RP?
|
decreases over 4 weeks
|
|
|
|
What factor predisposes a patient to have higher pain/sensitivity experience post Root planing and scaling therapy?
|
Pretreatment presence of anxiety, depression or stress.
Patients with sensitivity before tx also had higher levels of post sensitivity post tx. These patients may require tx post therapy |
|
|
|
What are the two different types of locally applied antimicrobials?
|
Mouthrinse
irrigation |
|
|
|
List some antimicrobials that act controlled released?
|
Tetracycline fibers (no longer on the market)
Chlorhexidine chips (periochip) Doxycycline gel Minocycline microsphere |
|
|
|
What are the indications for antimicrobial mouthrinses?
|
>Adjunct to S/RP during initial phase (patient has inflamed gingiva and heavy plaque build up)
>Handicapped patients/dexterity issues (use a cotton pellet to apply, don't rinse) >Immunocompromised patients >Orthodontic patients >Poster-periodontal surgery |
|
|
|
Disadvantages of mouthrinses?
|
➡ Contact time limited
➡ Compliance (metallic taste) ➡ Long term use not well researched ➡ DOES NOT ALTER SUBGINGIVAL FLORA (Aa and p. gingivalis not affected) Some effective in tx of gingivitis only, NOT periodontitis |
|
|
|
How can CHX affect subgingival flora indirectly?
|
By reducing supragingival bacterial load, you decrease GCF production from the body which is a source of nutrition for subgingival flora
|
|
|
|
What is the most effective mouth rinse?
|
Chlorhexidine digluconate
(brand name: Peridex/Periogard/OroClense) 33% reduction in plaque 25% reduction in gingivitis |
|
|
|
What does Peridex contain?
|
0.12% Chlorhexidine in 11.6% alcohol at a pH of 5.5
|
|
|
|
List some side effects of CHX
|

Increased Calculus accumulation
Altered taste sensation Staining (enamel, root, tongue and composite May cause mucosal ulceration |
|
|
|
Give a typical prescription for Chlorhexidine
|
RX: Chlorhexidine digluconate 0.12% mouthrinse
Disp: 475mL (One bottle) Sig: rinse with 15mL for 30 seconds 2x/day after breakfast and before bedtime for 14 days. DO NOT swallow |
|
|
|
What is the mechanism of action of CHX?
|
Cationic (+) molecule binds to negative charge on cell wall of bacteria and causes a alteration in the bacterial cell osmotic equilibrium. This leads to leakage of potassium and phosphorus resulting in a bacteriostatic effect.
At High concentration: the contents of bacterial cytoplasm precipitate, resulting in cell death |
|
|
|
What is the substantivity of CHX?
|
Absorbs into pellicle coated teeth and provides bacteriostatic action for 12 hours
|
|
|
|
List some medications that interact with CHX
|
None
|
|
|
|
Systemic Antibiotics advantages?
|
>Can readily reach microorganisms
>Can completely eradicate many pathogens from pockets >Can completely eradicate many pathogens from whole mouth >Time efficient |
|
|
|
Systemic Antibiotics disadvantages?
|
>Patient dependent (compliance)
>Patient sensitivity (allergic) >Superinfection (e.g. vaginitis) >Development of resistant strains >Drug-specific side effects |
|
|
|
Indications for systemic antibiotics as adjunct to conventional non-surgical tx?
|
>Aggressive types of periodontitis
>Recurrent or refractory periodontitis >Some cases of SEVERE chronic periodontitis with multiple deep peridontal pockets >Acute peridontal infections such as peridontal abscess or acute necrotizing periodontitis |
|
|
|
Should systemic antibiotics be prescribed for surgical tx?
|
No antibiotics for Crown lengthening
Membrane and bone graft require antibiotics because you are introducing foreign material (the rationale for the antibiotics is not for treatment rather for prevention). These patients can't brush for one week. |
|
|
|
If antibiotics are to be used as an adjunct to non-surgical mechanical debridement, when should they be used?
|
Antibiotic intake should start one the day of debridement COMPLETION. Debridement should be completed within a short time (<1week)
|
|
|
|
What systemic antibiotic is good against anaerobic bacteria?
|
Metronidazole (500mg TID for 8 days)
-->Not effective against Aa when used alone |
|
|
|
What systemic antibiotic is good for dealing with Abscesses
|
Clindamycine (300mg/TID for 8 days)
|
|
|
|
What systemic antibiotic is good against aerobic bacteria?
|
Amoxicillin
|
|
|
|
Which antibiotic cocktail should be prescribed for patients with aggressive periodontitis (where Aa is the primary instigator of the inflammation)
|
Metronidazole and Amoxicillin
(250mg of each drug TID for 8 days). |
|
|
|
What are the advantages of combination antibiotic therapy?
|
+Broadens the antimicrobial range of therapeutic regimen
+Prevents emergence of resistant bacteria +lowers dose of individual antibiotic |
|
|
|
What are the disadvantages of combination antibiotic therapy?
|
potential for antagonistic drug interaction with improperly selected antibiotics
|
|
|
|
Why should Tetracycline never be used with Metronidazole?
|
Tetracycline: Bacteriostatic
Metronidazole: Bacteriocidal Never combine bacteriostatic with Bacteriocidal. Bacteriocidal antibiotics only attack dividing cells. Bacteriostatic stops cell division. So essentially Tetracycline blocks Metronidazol from working. |
|
|
|
What treatments are included as part of the initial therapy after the Non-surgical phase?
|
>Removal of overhangs
>Correction of iatrogenic irritants (Bridge pontics) >Removal of natural plaque retentive areas (Odontoplasty of grooves, ridges, irregularities >Caries control >Removal of Overextended Crown Margins >Extraction of teeth with hopeless prognosis |
|
|
|
Should teeth be extracted before or after scaling/root planing
|
Doesn't matter. However, a potential benefit of extraction pre cleaning is that you reduce chance of calculus falling into socket and causing dry socket. Clean mouth may also help healing.
|
|
|
|
What are the 3 main objectives of re-evaluation?
|
1) To assess tissue response to the initial phase of therapy:
>Improvement in CCC? >Decrease in BOP? >how many sites have shown reduction in PD>2mm? 2) Assess patient's compliance with OH instruction 3) Do we need to consult with periodontist? > How many sites with PD>6mm? >Should I refer to a periodontist for periodontal surgery? >What should be appropriate interval for maintenance? |
|
|
|
Patient has just come in for a re-evaluation 8 weeks post initial phase. In quadrant 1 there is a isolated 7mm pocket on the distal of 16. Radiograph evaluation shows that there is localized horizontal bone loss in the area. Adjacent areas have only mild bone loss. Should surgery be done?
|
This situation is a "grey zone". For a isolated horizontal bone loss in a quadrant, we try to avoid raising a flap because we cause bone loss in the adjacent areas. We try to use local antibiotics instead
|
|
|
|
Patient has just come in for a re-evaluation 8 weeks post initial phase. In quadrant 1 there is a isolated 7mm pocket on the distal of 16. Radiograph evaluation shows that there is localized vertical loss in the area. Should surgery be done?
|
Yes. Vertical defects require raising a flap
|
|
|
|
Patient has just come in for a re-evaluation after 7 weeks post initial phase. Quadrant 4 has multiple sites with multiple deep pockets (7-8mm) with BOP. Should the patient enter the surgical phase?
|
Yes. Multiple sites in the same quadrant with sites greater than 6mm with BOP indicated for surgery.
|
|
|
|
Patient has a isolated class II furcation on 16. Patient wants to keep the tooth. What is the your next course of action?
|
We are required to refer a patient with a isolated class II furcation to a periodontist to receive a bone graft.
|
|
|
|
How long does it take for Connective tissue to repair after scaling and root planing?
|
4 weeks for Gingivitis
8 weeks for Periodontitis |
|
|
|
How long does it take for microbial repopulation after instrumentation in the absence of improved plaque control?
|
2 months. Therefore you should not wait longer than 2 months to have a re-evaluation because the pathogenic bacteria may have already repopulated the periodontal pockets
|
|
|
|
What is the ideal time frame to have re-evaluation appointment after initial root planing and scaling?
|
4-8 weeks
|
|
|
|
How long does it take for tooth mobility to reverse in a traumatized tooth after it's been removed from occlusion?
|
6-12 months
|
|
|
|
What data should be collected at the reevaluation?
|
Gingival tissue assessment
Probing depth/CAL BOP Mobility Marginal tissue recessions FURCATIONS Plaque score |
|
|
|
What results should we expect to see at re-evaluation?
|
Low plaque score (20% of surfaces with plaque)
Elimination or reduction in ginigval inflammation (Reduced BOP) A marked reduced number of surfaces with PD>4mm Decreased Mobility Pink and firm gingival tissue |
|
|
|
how much reduction in probing depth/gain in CAL should we expect to see after a single episode of supra/subgingival instrumentation?
|
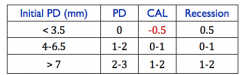
Notice. For PD less than 3.5, we actually LOSE clinical attachment. So don't jab shallow pockets!
For deeper pockets (greater than 7mm) we expect to see 1-2mm of CAL gain |
|
|
|
Fill in the blank:
Pockets >5mm associated with ________ rooted teeth will exhibit greater reduction in PD and gain in CAL |
Single
|
|
|
|
true or false?
"The amount of reduction is directly related to the intitial PD" |
True
|
|
|
|
Which teeth exhibit the greatest increase in PD and loss of attachment?
|
Teeth with furcation
|
|
|
|
Fill in the blank
The data collected at revaluation visit should be considered__________ that all following periodontal maintenance visits to be referred to |
baseline data
|
|
|
|
Fill in the blanks
If surgical phase is deemed necessary and has been undertaken, then the data collected at __________________ should be regarded as baseline data that all following maintenance visits should be referred to |
First visit following complete healing (3-6months post surgery)
|
|
|
|
What are the borders of the JE?
|
from base of gingival sulcus to CEJ
|
|
|
|
What is the turnover rate for JE?
|
4-6 days
|
|
|
|
Which bacteria are in the red complex?
|
P. gingivalis
T.forsythia T.denticola |
|
|
|
What type of bacteria are seen in healthy gingiva?
|
Gram +, aerobic
|
|

