![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
30 Cards in this Set
- Front
- Back
|
Name the four functions of gastric acid.
|
- facilitates digestion of protein
- facilitates the absorption of iron, B12, and calcium - prevents enteric infection and bacterial overgrowth (BOG) - facilitates the absorption of certain drugs such as thyroxin |
|
|
Grossly, the stomach can be divided into two functional areas: the oxyntic gland area or pyloric gland area. What are the anatomic areas that are in each?
|
Oxyntic = parietal, so that is the cardia, fundus and body, or 80% of the stomach
Pyloric gland area = antrum , 20% of the stomach |
|
|
True or False:
In the oxyntic gland, gastrin cells and somatostatin cells are coupled to each other and inhibit release of acid and histamine. |
FALSE. In oxyntic glands, aka glands with parietal cells (so in the fundus, body, cardia), ENTEROCHROMAFFIN-LIKE CELLS and somatostatin cells are coupled to each other to inhibit release of acid and histamine!
In antral gland, the gastrin and somatostatin cells are coupled together to inhibit gastrin secretion. |
|
|
The enteric nervous system consists of two main complexes: the [ myenteric / submucosal ] plexus, which innervates the circular and longitudinal muscle layers and regulates motility, and the [ myenteric / submucosal ] plexus, which innervates the mucosa and regulates secretion.
|
MYENTERIC PLEXUS = muscle layers
SUBMUCOSAL PLEXUS = mucosa and secretion |
|
|
Where are G cells located and what do they secrete?
|
G cells are located in the antral gland mucosa and secrete gastrin. Gastrin is one of three main stimulators of acid secretion. Other two are histamine and ACh.
Gastrin is a hormone that goes thru circulation to reach the parietal cells located in the upper stomach. Gastrin binds to gastrin receptors which are called CCK2 receptors. |
|
|
The three main stimulators of acid secretion are gastrin, histamine and ACh. Describe how each works (hormone/ neurotransmitter / paracrine pathway) and what receptors they bind to.
|
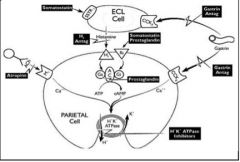
Gastrin - is a hromone, needs to go thru circulation to reach the parietal cells located in the upper stomach. Gastrin binds to gastrin receptors which are called CCK2 receptors.
Histamine - paracrine pathway. Secreted from ECL cells, which are near the parietal cells and teh histamine binds to H2 receptors on the parietal cell. There is then an increase in cAMP in the parietal cell which eventually leads to acid secretion. ACh- neurotransmitter secreted by the postgang neuron of enteric system and deposited onto the parietal cell's M3 receptor. |
|
|
________ is an acid secretor inhibitor. Inhibits histamine release indirectly and parietal cell directly.
|
Somatostatin
|
|
|
True or False:
H.pylori inhibits antral somatostatin secretion and thus stimulates gastrin adn acid secretion in patients with duodenal ulcer infected with the bacteria. |
TRUE
|
|
|
The final step in acid secretion involves activation of ______________. The pump, located on the canalicular membrane, reabsorbs _____ in exchange for _____. At the same time, membrane channels are activated that allow efflux of ___ and ____. The pump recycles most of the ____ exiting the parietal cell, the net result being the production of HCl.
|
The final step in acid secretion involves activation of H+K+ - ATPase. The pump, located on the canalicular membrane, reabsorbs K+ in exchange for H+. At the same time, membrane channels are activated that allow efflux of K+ and Cl-. The pump recycles most of the K+ exiting the parietal cell, the net result being the production of HCl.
|
|
|
Explain how acid secretion occurs with the H+ K+ - ATPase pump.
|
The final step in acid secretion involves activation of H+K+ - ATPase. The pump, located on the canalicular membrane, reabsorbs K+ in exchange for H+. At the same time, membrane channels are activated that allow efflux of K+ and Cl-. The pump recycles most of the K+ exiting the parietal cell, the net result being the production of HCl.
|
|
|
True or False:
PPIs work on the secretory cell (not resting parietal cell) so best to take it just prior to a meal. |
TRUE
Esp best with breakfast b/c new proton pumps are made while we sleep. If really severe, then best before breakfast and before dinner. |
|
|
Which of the following is FALSE regarding proton pump inhibitors?
A. The covalent inhibitors are prodrugs that circulate through the body after intestinal absorption. B. They are lipophilic C. They are weak bases D. They become activated sulfenamide and form ionic bonds with cysteines present in the extracellular loops of a subunit E. Acid secretion cannot resume until new enzyme is synthesized and inserted into the membrane F. Rebound acid hypersecretion can occur after stopping long-term (8+ weeks) PPIs |
The one that is FALSE is:
D. They become activated sulfenamide and form COVALENT DISULFIDE bonds with cysteines present in the extracellular loops of a subunit Note: Being lipophilic and membrane permeable, they gain access to all cells. However, being weak bases, they get protonated and trapped in acid spaces iwtha pH less than 4.0, such as secretory canaliculi of actively secreting parietal cells. |
|
|
What is Zolllinger-Ellison Syndrome (ZES)?
|
Gastroc acid hypersecretion due to an autonomous release of gastrin by an endocrine tumor, ex. a gastrinoma. (95% of gastrinomas are in the pancreas or duodenum)
|
|
|
How is gastric acid secretion measured in humans?
1. The sum of four 15-min collections during the first hour 2. The sum of four 15 min periods after pentagastrin 3. Twice the sum of the two highest consecutive 15 min periods after pentagastrin |
1. BAO, basal acid output
2. MAO, maximal acid output 3. PAO, peak acid output |
|
|
Define peptic ulcer dz.
|
A benign ulcerative lesion of the stomach (gastric ulcer) or duodenum (duodenal ulcer) that EXTENDS THRU THE MUSCULARIS MUCOSA.
|
|
|
What condition is described?
Imbalance between aggressive (ex. acid, pepsin, H.pylori, NSAIDs) and defensive (ex. epithelial cell integrity, mucus, bicarbonate, mucosal blood flow) factors. These disorders can be completely healed and remission maintained with antisecretory therapy. |
Peptic ulcer dz!
|
|
|
What is the treatment for peptic ulcer dz?
|
Antisecretory drugs (H2, PPIs)
Eliminate inciting factor (H.pylori, NSAIDs) Surgery (highly selective vagotomy) |
|
|
How can you detect the presence of Helicobacter pylori with regards to peptic ulcer dz?
|
Histologic stains, rapid urease test (urease activity metabolizes urea to NH3 and CO2), urea breath test, serology, culture.
|
|
|
Which of the following is FALSE about Helicobacter pylori?
A. is a spiral shaped gram negative bacterium with 4-6 unipolar flagella B. rapid urease test can detect its presence C. associated dzs include peptic ulcer dz D. patients with low grade MALT lymphoma should NOT be tested for H.pylori |
D. patients with low grade MALT lymphoma should NOT be tested for H.pylori
YES THEY SHOULD, in addition to patients with proven peptic ulcer dz! |
|
|
What are four conditions/diseases associated with Helicobacter pylori?
|
DU and GU (50-70%)
Chronic active superficial gastritis (100%) MALT lymphoma (marginal zone B-cell lymphoma) Gastric cancer |
|
|
True or False:
There is sufficient data to recommend anti-H.pylori therapy in patients with non-ulcer dyspepsia or patients with abdominal complaints but no documented ulcer. |
FALSE.
INSUFFICIENT DATA. |
|
|
Group the following into their appropriate suggested 14 day anti-H.pylori treatment regimens.
Amoxicillin BID Bismuth QID Clarithromycin 500 mg BID Clarithromycin 500 mg BID Lansoprazole BID Metronidazole 250 mg QID Metronidazole 500 mg BID Omeprazole BID Tetracycline QID |
1. Bismuth QID, Tetracycline QID, Metronidazole 250 mg QID
2. Metronidazole 500 mg BID, Omeprazole BID, Clarithromycin 500 mg BID 3. Amoxicillin BID, Clarithromycin 500 mg BID, Lansoprazole BID |
|
|
Which of the following is TRUE of helicobacter pylori?
A. Eradication is enhanced by regimen of antibitioics and cyclosporine. B. Patient must be off PPI for one month to prevent false negative rapid urease test, HP histology, and breath test. C. Serology may take up to 2 years to convert to negative after eradication |
C. Serology may take up to 2 years to convert to negative after eradication
The others would be true if... A. Eradication is enhanced by regimen of antibitioics and PPI, not cyclosporine! B. Patient must be off PPI for TWO WEEKS (not one month) to prevent false negative rapid urease test, HP histology, and breath test. |
|
|
GERD can occur after H.pylori is eradicated! This occurs in ____% of patients.
|
33%!
|
|
|
NSAIDs inhibit which enzyme?
|
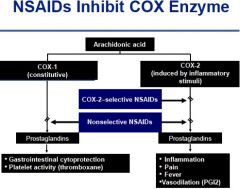
COX enzyme!
|
|
|
How do you prevent an NSAID-induced ulcer?
|
D/C NSAID (change it, decrease dose)
Take misoprostol Take a PPI Take a COX-2 selective NSAID like Celecoxib |
|
|
Who should receive prophylaxis (PPI) versus an NSAID-Induced Ulcer? (4)
|
1. Age > 65
2. History of Peptic Ulcer Dz and/or Upper GI bleeding 3. Concomitant steroids/ anticoagulants 4. Major co-morbid conditions |
|
|
20% of patients with multiple endocrine neoplasia type 1 (MEN-1) have this condition.
A. H.pylori bacterial overgrowth B. Peptic Ulcer Dizease C. Zenker's Syndrome D. Zollinger-Ellison Syndrome (ZES) |
D. Zollinger-Ellison Syndrome (ZES)
This is gastric acid hypersecretion due to an autonomous release of gastrin by an endocrine tumor, ie. a gastrinoma. Usually that gastrinoma is in the pancreas or duodenum. Clinical features are: pain only (25%), diarrhea only (20%), pain and diarrhea (50%), dysphagia/heartburn (30%) |
|
|
What are the clinical features of Zollinger-Ellison Syndrome (ZES) and how is it diagnosed?
|
Clinical features: pain only (25%), diarrhea only (20%), pain AND diarrhea (50%), dysphagia/heartburn (30%).
Diagnosed by: Elevated fasting gastrin (>1k pg/mL) and gastric pH < 2.5 OR Elevated fasting gastrin (<1k pg.mL) and gastric pH <2.5 and positive secretin test (+/- gastric analysis) |
|
|
How does one manage Zollinger-ELlison Syndrome?
|
Control acid hypersecrtion with PPIs, localize the tumor (if no liver mets, evaluate MEN-1 status), if no MEN, exploratory laparotomy
|

