![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
60 Cards in this Set
- Front
- Back
|
to echo); what is this type of MRI used for
|
- it is the FAT image bc it has a high SI for fat
-it is used for normal ANATOMY |
|
|
T2 weighted pulse sequence has a long TE and a long TR; what is it used for
|
- it is the WATER image
-it is used for FIT -Fluid (edema, hematoma) -Infection, Inflammation -Tumor |
|
|
what is a STIR sequence used for (short T1 Inversion recovery)
|
-used for evaluating edema in high lipid regions such as bone marrow
-also useful in evalauting articular caritlage bc hte joint fluid is bright and the cartilage is darker -tissues with longer T1 values will be such as water will have high SI and those with short T1 such as fat will be supressed |
|
|
what is a bone contusion and how will it appear on T1 and T2 MRI
|
-trabecular microfracture with edema and hemorrhage (Note: a bone contusion that involves cartilage is known as osteochondral or transchondral lesion)
--low SI on T1 -high SI on T2 bc of hemorrhage |
|
|
what is a stress fx and how does it appear on MRI
|
-gradual and progressive resorption and replacement of bone
-linear zone of decreased SI surrounded by less defined area of low SI onT1 -linear zone with decreased SI, but with surrounding edema of higher SI -inc SI in STR bc fatty bone marrow is supressed |
|
|
neuropathic osteoarthropathy - what is it and how does it appear on MRI
|
-difficult to distinguish from OM
-marrow signal changes w/o involvement of periosteum/cortex -T1: decreased in SI in medullary and cancellous bone -T2; mild increase in SI (less then with OM) STIR-inc in SI |
|
|
how does acute OM appear on MRI
|
T1- involement of medullary bone has inc SI
T2 and STIR-inc SI in medullary portion of involved bone, this rep. dec in normal fat content and localized pus and edema |
|
|
chronic osteomyelitis on MRI
|
-sinus tracts show as linear areas of increased SI on T2
-foci may have "rim sign" (low SI area surrounded by an area of local active disease |
|
|
what sequences are used for soft tissue infections on MRI; how do they appear
|
-T2 and STIR are best for cellulitis and abscesses
-inc SI in cellulitis from distortion of tissue -well marginated homogenous high SI is seen in abscesses -if abscess has gas contained in it will be low SI on all sequences |
|
|
what is the hallmark of osteonecrosis (AVN) on MRI
|
-"reactive interface"; distinct layer of inflammatory tissue between viable and infarcted bone
|
|
|
how does AVN (osteonecrosis) of bone appear on MRI
|
T1- well defined line of decreased SI (this is granulation replacement of fat)
T2 - decreased SI STIR- "double rim sign" |
|
|
what is the "double rim sign"
|
-it is AVN as seen on STIR
-the inner margin is inc SI (represents granualtion tissue) -the outer margin is dec SI (represents mineralization) |
|
|
late stage AVN has fibrosis and sclerosis taking place (rather then the necrosis and hemorrhage); how does MRI appear
|
-dec on T1 and T2
|
|
|
how do osteochondral lesions appear on MRI
|
T1 - dec SI within subchondral bone
T2- SI may be increased STIR - inc SI |
|
|
how do tendons appear on MRI
|
-low SI on all sequences due to lower water content
-T2 and STIR; optimizes contrast b/w darl tendon and abnormal increase in water content of the tendon |
|
|
how do soft tissue masses appear on MRI
|
-such as lipoma, hemangioma, ganglions
-low on T1, high on T2 |
|
|
septic arthritis on MRI
|
-T2 and STIR; inc signal with in surrounding soft tissues as well as joint fluid (but you need clinical correlation-hot, swollen, tender restricted joint)
|
|
|
which type of metal cant be used in an MRI
|
-ferro-magnetic objects bc they have their own magnetic field
-most ortho implants are non ferromagnetic |
|
|
AVN
|
|

|
osteomyelitis
|
|
|
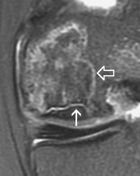
Partal thickness tear of PT tendon
|
|

|
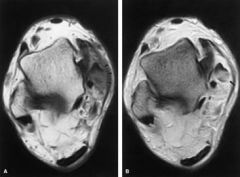
T1 of charcot (note that fat is still intact, so this differs it from OM)
|
|

|
T1 stress fx of calcaneus
|
|

|
T2 bone contusion
|
|
|
What is the science behind using Technitium 99
|
- the isotope binds directly to calcium hydorxyapatite to form soluble salts
-it is referred to as a "bone seeking agent" -the isotope concentrates in active new bone formation due to osteoblastic activity related to bone injury |
|
|
when will you have positive Tech 99 bone scans be used for
|
-OM
-Neuropathic osteoarthropathy -bone tumors -fracture -recent surgery -arthritis -RSD (reflex symapthetic dystrophy) -ischemic necrosis of bone |
|
|
what is the half life of tech 99
|
6 hours
|
|
|
there are areas of the body where increased levels of Tech 99 isotope occurs in normal bone; what are these areas
|
-cancellous bone>cortical
-metaphyseal bone -periarticular regions -epiphyseal plates -tips of scapula -stermum -costochondral margin of ribs |
|
|
how many phases of bone scanning are there
|
-4 phases
1. Angiogram (2-3 secs after injection several images are taken to show arterial flow to LE) 2. Blood Pool (images taken 2-5 mins post injection shows blood pooling in veins and cap beds) 3. delayed phase (2-4 hours later images show isotope seeks bone and shows osteoblastic activity 4. fourth phase (images taken 5-24 hours post injection to show more bone activity and less soft tissue activity) |
|
|
how long do you wait to take images for a 3rd phase bone scan
|
-2-4 hours post injection to show osteoblastic activity
|
|
|
increased diffuse uptake in phase 1 and phase 2 of bone scan
|
-cellulitis
|
|
|
increased focal uptake in all 3 phases
|
OM
|
|
|
with inflammation, the blood flow is increased due to the dilation of capillaries, which phase of a bone scan does this show on
|
phase 2 (blood pool phase)
|
|
|
why does phase 3 and 4 of a bone scan show more bone activity and less soft tissue activity
|
-because of the 6 hour half life of tech 99, urination has decreased the amt of isotope in the soft tissue
|
|
|
how do you differentiate soft tissue infections from bone infections using a bone scan
|
-look at phase 3 and 4 for bone infections
|
|
|
describe how OM would look on phase 2,3,4 of bone scan
|
-focal uptake on 2nd
-hot on 3rd -hot on 4th |
|
|
describe how cellulitis would look on 2,3,4 phase of bone scan
|
-diffuse uptake on 2nd
-neg on 3rd -neg on 4th |
|
|
describe how septic arthritis would look on 2,3,4 phase of bone scan
|
-diffuse uptake on all phases
|
|
|
when gallium is used for bone scans - what areas does gallium localize to
|
-areas of acute inflammation and infection by binding to bacteria and leukocytes
-suggested to be more accurate in bone and joint infections in kids then Tech scan |
|
|
how long after Gallium injection should images be taken
|
-48-72 hours after injection of isotope
|
|
|
how is an indium 111 bone scan performed
|
-WBC are isolated from the blood and labeled with indium 111 and injected back into the pt
-scan is performed 24 hours later |
|
|
why does acute OM show up positive on Indium scan, but chronic OM is negative on indium scan
|
-acute OM is a neutrophil response
-chronic OM is a lymphocytic response -remember you are tagging WBC with indium |
|
|
what is the half life of indium
|
67 hours
|
|
|
what type of scan can help differ b/w OM and osteoarthropathy
|
-Indium 111 scan
-acute OM will have positive scan, but chronic OM and osteoarthropathy will be negative |
|
|
list the following in order of highest density to lowest density on CT scan; ligament, tendon, cartilage, calcification, cortical bone, cancellous bone, nerve, fat, air
|
Highest density
cortical bone calcification cancellous bone nerve tendon ligament cartilage fat air |
|
|
what would give a cold spot on a tech 99 bone scan
|
-is due to NO delivery of the tracer as a result of poor circulation, necrosis, or a
fulminant destructive osteomyelitis not accompanied by significant reparative processes which is also due to poor circulation |
|
|
99m Technetium-MDP is currently the most frequently used radionuclide; which part attaches to hydroxy apatite crystal of bone and which is just the label
|
-MDP absorbs to bone
-Tech 99 is just the label |
|
|
how does tech 99 imaging compare to Gallium imaging
|
-Tech 99 uses less time, exposure and money
|
|
|
Tech 99 scans can be used for acute and chronic (inactive) OM, charcot, fracture, septic arthritis and cellulitis; which can Gallium and Indium also be used for
|
-septic arthritis
-cellulitis -acute OM |
|
|
when is indium 111 WBC labeling use for the bone scan
|
This technique is reserved for complicated posttraumatic
or post-surgical patients with equivocal conventional bone scans, in cases where 99mTc MDP scanning reveals false positive results because of rapid turnover. |
|
|
uorAn imaging modality in which x-rays are produced
continuously on demand to give a real-time, dynamic image that is displayed on a television screen. |
fluorscopy
|
|
|
What are the basics of how MRI work
|
In the human
body, protons (H+) spin randomly. When the body is placed in the MRI machine, most of the protons line up parallel to the magnetic field of the machine. Feeding radiowaves into the body (RF), the protons are excited and energy is released producing an image. |
|
|
if an MRI image has TR500/TE30 on it, what does that mean
|
-T1 image
|
|
|
Cortical bone and tendons have fewer moveable protons (low water content), making them appear how on MRI
|
dark
|
|
|
Dark areas on T1
|
tendons, subchondral cortex of bone, blood vessels
with moving blood, ligaments, muscles, tumors |
|
|
Dark areas on T2
|
-ligaments
-compact bone |
|
|
Light areas on T2
|
-stationary blood
-tumor |
|
|
Light areas on T1
|
-fat
-medullary bone -non moving blood |
|
|
tarsal coalitions, MRI or CT
|
CT
|
|
|
Good for the diagnosis of capsular or ligamentous tears
|
Arthrography - inject contrast medium into the joints and xray
|

