![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
125 Cards in this Set
- Front
- Back
|
Compare the glomerular filtrate to the plasma?
|
It has the same chemical composition but it contains almost no proteins b/c large molecules d not radily cross the glomerular wall.
|
|
|
what is the capillary filtration pressure of the glomerulus? how is this different from the rest of the body? how is this pressure regulated?
|
it's about 60mmHg w/c is about 2-3x higher than other capillary beds in the body. The filtration pressure & GFR are regulated by the constriction & relaxation of the afferent & efferent arterioles
|
|
|
What is the innervation of the afferent & efferent arterioles?
|
sympathetic nervous system
|
|
|
in the mechanism of transport in the nephron, what 2 substances are passively transported along [ ] gradients?
|
urea & water
|
|
|
Over half of all reabsorptive & secretory processes that occur in the tubulr system occur in w/c part of the nephron?
|
PCT
|
|
|
What is the role of glucose in the nephron?
|
it is freely filtered in the glomerulus & reabsorbed by energy dependent cotransport carrier mechanisms
|
|
|
W/c part of the nephron is affected by ADH?
|
Loop of Henle
|
|
|
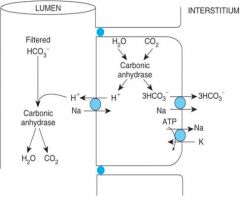
what transport mechanisms are found in PCT?
|
secondary active transport or cotransport of Na w/ glucose or aa from the tubules to the peritubular capillary
There is also a countertransport of Na in for H to go to the tubules. There is a primary counter transport that allows Na to the blood & K into the PCT cell but K leaks back into the blood. See Fig 30.7 |
|
|
The LOH as a whole, reabsorbs what? how is this different from PCT?
|
always reabsorbs more sodium & chloride than water. this in contrast to PCT w/ reabsorbs sodium & water in equal amounts
|
|
|
W/c part of the LOH is highly permeable to water?
|
the thin descending limb
|
|
|
Where is the highest osmolality of filterate in LOH?
|
at the elbow of the LOH
|
|
|
W/c part of the LOH is IMpermeable to water? what happens in this part?
|
ascending limb. solutes are reabsorbed but water cannot follow. As a result, the tubular filtrate becomes more & more dilute
|
|
|
what type of transport does the thick ascending LOH contain?
|
Na/K/2Cl cotransport system. The gradient for this cotransport is provided by Na/K ATPase pump on peritbular cap side
|
|
|
What does the reabsorption of Na, K, & Cl in the thick LOH do?
|
it leads to the development of a transmembrane potential that favors the passive reabsorption of small divalent cations such as Ca & Mg
|
|
|
Besides the ascending limb, what other part is IMpermeable to water
|
DCT
|
|
|
What type of transport is found in the DCT
|
There is a Na/Cl cotransport mechanism that allows reabsorption of these ions
|
|
|
Where in the tubules is Ca affected?
|
1st in the thick ascending LOH where it's passively reabsorbed. 2nd in the DCT where it is actively reabsorbed in a process that is largely regulated by PTH
|
|
|
Where in the tubule does aldesterone exert its action? what does it do?
|
in the late distal tubule & cortical collecting tubule. it exerts its action on Na reabsorption & K elimination
|
|
|
The cells in the thick ascending limb closest to Bowman's capsule (between the afferent and efferent arterioles) are specialized cells known as
|
the macula densa
|
|
|
What marks the end of the thick ascending limb and the beginning of the distal convoluted tubule?
|
The macula densa
|
|
|
collecting ducts eventually empty where
|
each empties into a calyx of the renal pelvis.
|
|
|
Each renal calyx is continuous with?
|
the ureter
|
|
|
w/c part of the nephron passes right between the afferent & efferent arterioles?
|
thick ascending limb of the nephron
|
|
|
T/F: afferent arterioles & glomeruli are found in the cortex and medulla
|
False: they are only found in the cortex
|
|
|
Substances that are present in the filtrate at the same concentration as found in the plasma are said to be?
|
freely filtered.
|
|
|
Give examples of things that are freely filtered?
|
ions sodium, potassium, chloride, and bicarbonate; the neutral organics glucose and urea; amino acids; and peptides like insulin and antidiuretic hormone (ADH).
|
|
|
in the PCT, secretion of what occurs?
|
It is the site of secretion of a number of organic substances that are either metabolic waste products (eg, urate, creatinine) or drugs (eg, penicillin)
|
|
|
how do you calculate RPF?
|
it's RBF of 1.1L/min * .55 (plasma) The renal plasma flow (RPF) = 0.55 x 1.1 L/min = 605 mL/min
|
|
|
what is the equation for net filtration pressure
|
NFP = (PGC – GC) – (PBC – BC),
|
|
|
what is the equation for GFR?
|
GFR = Kf (PGC – PBC – GC).
|
|
|
Ridding the body of a substance is often called?
|
clearance
|
|
|
The units of renal clearance are volume per time (not amount per time). Explain by example what this means?
|
The easiest way to think of this is to ask what volume of plasma contains the amount excreted in a given time. Suppose 5 mg of a substance is excreted per hour and 200 mL of plasma contains 5 mg. Then the clearance of the substance is 200 mL/h, ie, 200 mL of volume has been completely cleared of the substance. Again, note the units: volume per time (ie, the volume of plasma from which a substance is completely removed [cleared]).
|
|
|
Can something have a clearance greater than the GFR?
|
Indeed, yes. One such substance is para-aminohippurate (PAH).
|
|
|
What substance can approximately measure RBF? how?
|
PAH. It is freely filtered and also avidly secreted by the proximal tubule epithelium (via the transcellular route). The secretion rate is saturable. (That is, there is a maximum rate of PAH secretion into the tubule. However, at low plasma concentrations, about 90% of the PAH entering the kidney is removed from the plasma and excreted in the urine. Its clearance, therefore, is nearly as great as the renal plasma flow.
|
|
|
Can a freely filtered substance have a clearance value less than the GFR? give examples
|
Yes. insulin & glucose have 0 clearance b/c the first is completely degraded & the latter is completely reabsorbed. Ions have clearance less than GFR b/c most of their amount is reabsorbed back.
|
|
|
What can the clearance of a substance tell us, in another words, be familiar w/ secretion, reabsorption, & filtration of a substance?
|
If we know the GFR (as assessed from inulin clearance) and the clearance of a given substance, then any difference between clearance and GFR represents net secretion or reabsorption (or, in a few rare cases, renal synthesis). If the clearance of a substance exactly equals the GFR, then there has been no net reabsorption or secretion. If the clearance is greater than the GFR, there must have been net secretion. Finally, if the clearance is less than the GFR, there must have been net reabsorption
|
|
|
Define filtered load?
|
It’s the amount that is filtered per unit time.
|
|
|
The _________ __________ is what is presented to the rest of the nephron to handle?
|
Filtered load
|
|
|
What does a high filtered load mean?
|
It indicates a substantial amount of material to reabsorb
|
|
|
This term a mechanism through which renal blood flow and glomerular filtration rate are kept relatively constant across a wide range of systemic arterial pressures?
|
Autoregulation
|
|
|
What happens if autoregulation is absent? How would abesence of autoregulation affect the glomerular capillaries?
|
Urinary output would vary widely with changes in blood pressure produced by normal daily activities. glomerular capillaries (which have higher basal pressure than capillaries elsewhere in the body) would be at high risk of hypertensive damage during periods of exertion.
|
|
|
As mean arterial pressure goes up, smooth muscle in the walls of the arterioles is stretched. This induces the smooth muscle to constrict, thereby increasing vascular resistance?
|
Myogenic response
|
|
|
Cells of the macula densa respond to the level _______ in the distal tubule?
|
Na
|
|
|
Relate [Na] in distal tubule to GFR?
|
[Na+] in the distal tubule is high when GFR is high, and low when GFR is low.
|
|
|
High [Na+] in the distal tubule causes release of ‘transmitter agents’ from the JGA. These agents lower GFR in two ways, what are they?
|
1)By causing constriction of the afferent arteriole. 2) By causing contraction of the glomerular mesangial cells (decreasing surface area of the capillaries and thus KF).
|
|
|
T/F: Renal clearance does not indicate the amount of substance excreted per unit time.
|
True
|
|
|
How to calculate clearance in the proper units?
|
CS = US*V / PS Where: CS = clearance of S US = urine concentration of S V = volume of urine per unit time PS= plasma concentration of S.
|
|
|
What is the equation from excretion rate?
|
(US * V) is the excretion rate
|
|
|
renal clearance deals specifically with clearance performed by the ________. It should not be confused with _______ clearance rate, which may involve many additional processes.
|
Kidneys, metabolic clearance
|
|
|
In order to provide an accurate measure of GFR, a compound must meet the following criteria (5)?
|
1. freely filterable 2. not reabsorbed 3. not secreted 4. not synthesized by the tubules 5. not metabolized by the tubules.
|
|
|
What is the gold standard for accurate measurement of GFR? Why is this not used clinically?
|
Inulin. inulin clearance is cumbersome due to the requirement to infuse inulin to obtain constant plasma concentration.
|
|
|
What is used instead of inulin to measure GFR?
|
Creatinine clearance
|
|
|
Where do we get creatinine from?
|
Creatinine (end product of creatine metabolism) is constantly exported into our blood at a rate proportional to skeletal muscle mass
|
|
|
Does creatinin meat all five criteria for GFR measurement? Why or why not?
|
creatinine does not meet all five criteria; it is freely filtered, and not reabsorbed, however, it is secreted by the tubules in small amounts (10-20% of what is excreted).
|
|
|
B/c of its clearance, creatinine clearance slightly _________ GFR.
|
Overestimates GFR since it’s freely filtered but some is also secreted so its number is actually higher than GFR.
|
|
|
Rising plasma creatinine over time indicates what?
|
It’s a red flag that indicates a potential renal dysfxn
|
|
|
What happens to creatinine if one day GFR suddenly decreases by 50%?
|
This means that there is a possible blockage like a blood clot w/c will increase plasma creatinine
|
|
|
The epithelial cells between the tubule lumen & peritublular capillary have what names to those sides?
|
Apical membrane is to the side next to the lumen & basolateral membrane is to the side facing the capillary
|
|
|
Reabsorption thru the epithelial cells occurs thru what 2 mechanisms?
|
Either thru gaps between cells called paracellular reabsorption or thru the cells called transcellular reabsorption.
|
|
|
There is a lesser role for transepithelial voltage in paracellular transport. Where is this voltage difference & what does it do?
|
1) early in proximal tubule lumen is slightly negative of interstitium.
2) late in proximal tubule it is slightly positive. This enhances anion reabsorption early in the tubule, and diminishes it later. |
|
|
Transport mechanisms can be categorized by the properties of their limits as: what are the 2 transport mechanisms?
|
Tubular maximum-limited (Tm limited) systems
Gradient limited systems |
|
|
How does the Tm transport system work?
|
Tm systems reach an upper limit because transporters are saturated. From that point, increased plasma concentration does not produce increased reabsorption.
|
|
|
How does the gradient transport limited system work?
|
Gradient limited systems reach a limit because tight junctions are leaky, and any significant lowering of luminal concentration relative to the interstitum results in a leak back into the lumen as fast as the substance is transported out.
|
|
|
Increased sympathetic activity causes ____________ of the afferent & efferent arterioles & thus a ________ in RBF.
|
constriction, decrease
|
|
|
these are special hairpin shaped capillaries along the loops of Henle & found in the juxtamedullary nephrons
|
vasa recta w/c descend into the medullary portion of the kidney.
|
|
|
The __________ __________ is thought to prepresent a feedback control system that links changes in the GFR w/ RBF?
|
juxtaglomerular complex
|
|
|
The distal tubular site that is nearest the glomerulus is characterized by densely nucleated cells called _________ _________. in the adjacent afferent arteriole, the sm mm cells are modified as special secretory cells called ____________ cells
|
macula densa, juxtaglomerular cells
|
|
|
What is found in the juxtaglomerular cells?
|
granules of inactive renin
|
|
|
what is the function of renin?
|
it's an enzyme that fxns in the conversion of angiotensinogen to AG
|
|
|
How does tubular secretion occur?
|
like reabsorption, this an occur by diffusion or by transcellular transport mechanisms.
|
|
|
What does tubular secretion require?
|
Active transport across the basolateral or luminal membrane of epithelial cells
|
|
|
What happens in the kidneys during a fast?
|
cells of the renal tubules synthesize glucose and add it to the blood.
|
|
|
What type of metabolism occurs in the tubules?
|
They can also catabolize peptides, and a number of organic substances present in the tubular lumen or peritubular capillaries. This is also a form of excretion as catabolized substances are effectively eliminated from the body.
|
|
|
abnormality in the Na+ glucose cotransporter that mediates reabsorption of glucose in the proximal tubule. Leads to appearance of glucose in the urine.
|
familial renal glucosuria:
|
|
|
ability to absorb glucose is usually normal, but filtered load of glucose exceeds the threshold for the tubule to reabsorb. (lack of insulin or failure to respond to insulin leads to high blood sugar).
|
Diabetes mellitus:
|
|
|
What is the primary role of the PCT?
|
Reabsorb most the filtered water & non waste solutes
|
|
|
Urinary water excretion can vary from approximately 0.4 L/day to___________?
|
25 L/day!
|
|
|
Na+ reabsorption is an active process occurring in all tubular segments except where?
|
descending limb of the loop of Henle.
|
|
|
T/F: glucose is reabsorbed by the paracellular route?
|
False: transcellular route
|
|
|
T/F: Both Na+ and water undergo considerable reabsorption, but no secretion.
|
True
|
|
|
How does Na reabsorption achieve reabsorption of phosphate & sulfate?
|
Cotransport across the luminal membrane
|
|
|
How does Na achieve H ions secretion?
|
By countertransport across the luminal membrane
|
|
|
What are the secretion of H ions required for?
|
Reabsorption of bicarbonate
|
|
|
What is Na’s affect on Cl?
|
Achieves reabsorption of Cl by indirect cotransport (Cl-/base countertrasnporters depend on Na+/H+ countertrasnporters)
|
|
|
It can be said that the PCT promotes ________ osmotic volume reabsorption?
|
Iso-osmotic
|
|
|
What can be said about the transporters in the kidneys?
|
a given transporter selectively takes up one or a few substrates and ignores all others. However, there is not a separate transporter for every solute in the body. Two or more closely related substances may use the same transporter. For example, the amino acid transporters are distinct from those for glucose and other monosaccharides
|
|
|
w/ what mechanism is glucose reabsorbed in the PCT?
|
This involves removing glucose from the tubular lumen along with sodium via a sodium-dependent glucose symporter (SGLUT) across the apical membrane of proximal convoluted tubule epithelial cells, followed by its exit across the basolateral membrane into the interstitium via a GLUT uniporter
|
|
|
Although we sometimes say that the glomerular filtrate is protein-free, it is not truly free of all protein since small and medium-size proteins (eg, angiotensin, insulin) are filtered in considerable quantities. What eventually happens to these filtered proteins?
|
The proximal tubule is capable of taking up filtered albumin and other proteins, and we treat this protein uptake separately here to emphasize its importance. We use the word uptake rather than reabsorption because the proteins, although they are transported intact out of the lumen into the epithelial cells, are degraded into their constituent amino acids before being transported into the cortical interstitium. Thus, the term reabsorption in the context of proteins and peptides, although widely used, is actually a misnomer.
|
|
|
What are the steps for the reuptake of the proteins that filter thru?
|
The initial step for the uptake of larger proteins is endocytosis at the luminal membrane. This energy-requiring process is triggered by the binding of filtered protein molecules to specific receptors on the luminal membrane. Therefore, the rate of endocytosis is increased in proportion to the concentration of protein in the glomerular filtrate until a maximal rate of vesicle formation, and thus the Tm for protein uptake, is reached. The pinched-off intracellular vesicles resulting from endocytosis merge with lysosomes, whose enzymes degrade the protein to low-molecular-weight fragments, mainly individual amino acids. These end products then exit the cells across the basolateral membrane into the interstitial fluid, from which they gain entry to the peritubular capillaries
|
|
|
What happens if there is an increase in protein filtration?
|
The endocytic mechanism by which protein is taken up is easily saturated; however, any large increase in filtered protein resulting from increased glomerular permeability can cause the excretion of large quantities of protein
|
|
|
Where does ADH act in the tubules?
|
Cortical collecting ducts
|
|
|
How does ADH act in reabsorbing water?
|
It stimulates insertion of specific aquaporins into the luminal membrane. When aquaporins are present, water reabsorption is high, and urine concentration is increased.
|
|
|
w/ maximum reabsorption of water, final urine volume would be what compared to filtered water? Compare its osmolarity to plasma?
|
With maximum reabsorption, final urine volume can contain less than 1% of filtered water. In this situation urine is very hyperosmotic relative to plasma (as high as 1400 mOsmol /L vs. 285-300 mOsm /L).
|
|
|
What type of Na transport is seen in the thick & thin ascending limb?
|
In the thick: Na transport depends on Na-Cl co-transporters. In the thin: there is no Na-Cl co-transporters so Na reabsorption depends on simple diffusion
|
|
|
What is the permeability of water in the thick & thin limbs?
|
Both thick and thin ascending limbs of the loop of Henle are relatively impermeant to water, so in the entire ascending limb, salt is reabsorbed, but water is not.
|
|
|
What happens w/ water & Na in the the descending limb?
|
does not reabsorb Na+ but is highly permeant to water.
|
|
|
W/c 2 areas of the tubules are diluting segments?
|
Ascending limb & DCT
|
|
|
What channels are found in the DCT?
|
Na/K pump on basolateral membrane, Na/Cl symport on apical membrane, & Na channels on apical membrane
|
|
|
Where do thiazide diuretics target?
|
Na Cl symport in DCT
|
|
|
What is the osmolarity of the tubular lumen when it reaches the collecting ducts?
|
w/ the absence of vasopressin, water is not allowed to leave & therefore lumen will be hypo-osmotic in relation to the plasma
|
|
|
What is the permeability & transport of urea?
|
It’s small, polar, & water soluble. b/c it’s polar, it’s not very membrane permeant so movment across membranes is facilitated by uniporters
|
|
|
How does urea get into the tubules?
|
It’s freely filtered but ½ gets reabsorbed in the PCT. The amount reabsorbed gets secreted in the LOH. ½ of that gets reabsorbed in the medullary collecting duct.
|
|
|
What is the reabsorption mechanism of urea in the PCT?
|
By diffusion & paracellular
|
|
|
How does urea work in concentrating urine?
|
Since some of the urea gets reabsorbed, it is in the interstitial space & therefore contributes to the hyperosmotic conditions that are necessary to [ ] urine in the presence of ADH
|
|
|
Aldosterone is a steroid hormone produced by the_________ __________?
|
adrenal cortex
|
|
|
Function of Aldosterone & where does it act?
|
Aldosterone stimulates Na+ reabsorption by the distal convoluted tubule and the cortical collecting ducts.
|
|
|
In what situation would aldosterone be released?
|
Adrenal secretion of aldosterone is high when Na+ intake or blood volume is low
|
|
|
How is aldosterone regulated?
|
Aldosterone secretion can be regulated through several systems, however the core regulation is via the renin angiotensin system.
|
|
|
What cells release renin?
|
release of renin from the granular cells of the juxtaglomerular apparatus.
|
|
|
What 3 primary factors cause the release of renin?
|
1) arterial BP, 2) sympathetic input to the JGA, & 3) Na content in DCT as sensed by the cells of the macula densa.
|
|
|
What regulates vasopressin?
|
Depends on activity of discrete group of hypothalamic neurons; the input to these neurons comes from osmoR & baroR.
|
|
|
When do osmoR activated?
|
When there is excess water so they help to increase water excretion
|
|
|
Where are BaroR found & when do they decrease their firing?
|
Baroreceptors in the cardiovascular system decrease their firing rate when cardiovascular pressure deceases.
|
|
|
How is ADH affected when baroR are firing?
|
Baroreceptor firing normally reduces vasopressin secretion (through an inhibitory interneuron), so a reduction in baroreceptor firing leads to an increase in vasopressin release.
|
|
|
What is the major extracellular buffer in human physiology?
|
CO2/HCO3 system
|
|
|
How does the kidney maintain plasma pH?
|
by regulating excretion or reabsorption of bicarbonate as necessary to maintain proper plasma hydrogen concentration
|
|
|
What is the relationship of HCO3 & H in the kidneys?
|
excretion of bicarbonate increases plasma hydrogen ion concentration. addition of bicarbonate to the plasma lowers plasma hydrogen concentration.
|
|
|
What is the fate of bicarbonate in the kidneys?
|
Bicarbonate is freely filtered and normally is completely ‘reabsorbed’.
|
|
|
What happens to the filtered HCO3?
|
It’s converted to water & CO2 in the lumen of the tubules by carbonic anhydrase. For this reaction to occur, H must combine w/ bicarb.
|
|
|
How is bicarb reabsorbed & where in the tubule does it occur?
|
For each H that combines w/ bicarb in the lumen, a different bicarb is reabsorbed from the epithelial cell into the interstitium. see part 5 slide 8
|
|
|
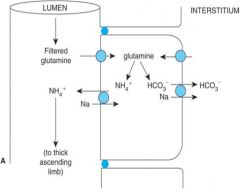
How does the kidney prevent acidosis? 2 mechanisms
|
Mechanism 1: If plasma begins to become too acidic, there will be more hydrogen secreted into the tubule than is necessary to reabsorb all the filtered bicarbonate. This leads excretion of hydrogen bound to non-bicarbonate buffers (and thus produces a net increase in bicarbonate in the plasma (preventing acidosis).
Mechanism 2: Glutamine is released from the liver as an additional byproduct of protein catabolism. Filtered glutamine enters tubular epithelial cells through both the basolateral and tubular membrane. Inside the epithelial cells, glutamine is metabolized producing both ammonium and bicarbonate. The ammonium is actively secreted via a sodium/ammonium antiporter. The bicarbonate is reabsorbed, causing a net increase in plasma bicarbonate. As before, this reduced plasma hydrogen ion concentration and helps prevent acidosis. |
|
|
How do the kidneys prevent alkalosis?
|
As alkalosis begins to occur, hydrogen ion secretion from the tubular epithelial cells will become insufficient to reabsorb all the filtered bicarbonate.
As a result significant bicarbonate will be secreted in the urine, and there will be little or no secretion of hydrogen on non-bicarbonate buffers. Similarly, glutamine metabolism can be temporarily slowed to prevent contribution of bicarbonate to the plasma from this source. Collectively, these mechanisms reduce plasma bicarbonate, raising plasma hydrogen ion concentration, and prevent alkalosis. |
|
|
What is the fate of K in the kidney? Where is it excreted?
|
K+ is freely filtered and heavily reabsorbed (normally not much K+ in urine). However if K+ intake exceeds needs, K+ can be excreted in the cortical collecting ducts.
|
|
|
What causes K to excreted? (2 mechanisms)
|
2 mechanisms: 1. increased activity of basolateral N+/K+ ATPase. 2. depolarization of cells in the adrenal cortex, and subsequent release of aldosterone.
|
|
|
Relate the activity of excitable cells to amount of K levels?
|
Both an increase & decrease in K will cause heart arrhythmias
|

