![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
118 Cards in this Set
- Front
- Back
|
In order for the kidney to function normally, what 3 things must occur?
|
There must be adequate blood flow thru the GC. The glomerulus must be intact, and tubules must be able to reabsorb & excrete normally
|
|
|
a condition in which the kidneys fail to remove the metabolic end products from the blood and to regulate fluid, electrolyte, and pH balance of the extracellular fluids.
|
Renal failure
|
|
|
What are some underlying causes of renal failure?
|
Renal or systemic dz
|
|
|
progressive, slow development of renal failure – course of years
|
Chronic
|
|
|
Chronic renal dz can affect w/c areas of the kidney?
|
Glomerulus, renal tubules, blood perfusion
|
|
|
T/F: many of the chronic renal disorders are reversible?
|
False: they are usually NOT reversible
|
|
|
As renal dz progresses, how can we find the origin of the dz?
|
Although renal dz can start in any area of the kidney, as the dz progresses it’s often difficult to determine the original cause since all of the kidney can become destroyed or scarred.
|
|
|
Name a kidney dz that involves the glomerulus?
|
Glomerulonephiritis
|
|
|
Name 2 kidney dzs that inolve the renal tubules?
|
Pyelonephritis & polycystic kidney dz
|
|
|
Name a dz that interferes w/ blood perfusion of the kidneys?
|
nephrosclerosis
|
|
|
a rapid decline in kidney function, resulting in an inability to maintain fluid and electrolyte homeostasis and failure to excrete nitrogenous wastes.
|
Acute renal failure
|
|
|
Acute renal failure is characterized by a sudden drop in __________ & fall in ______________?
|
Urine output & fall in GFR
|
|
|
T/F: Acute renal failure is considered a reversible dz?
|
True
|
|
|
In acute renal failure, dysfunction can be in w/c 3 places?
|
Dysfunction can be pre-renal (blood flow), Post-renal (obstruction), or renal (acute tubular necrosis)
|
|
|
What is a common indicator of ARF?
|
Azotemia
|
|
|
What are the 3 characteristics of ARF?
|
1) Is associated w/ an increased morbidity & mortality 2) more susceptible in the elderly, 3) more common in seriously ill pts in ICU
|
|
|
This refers to retention of nitrogenous wastes, either through inability of the kidney to excrete them or through their failure to be delivered to the kidney?
|
Azotemia
|
|
|
Azotemia is reflected by an increase in __________?
|
BUN
|
|
|
Complex syndrome characterized by variable and biochemical and clinical changes that occurs when azotemia becomes symptomatic- all organs affected?
|
Uremia
|
|
|
In uremia, what changes are seen in the body?
|
Volume derangements, acid/base problems, electrolyte imbalances, endocrine changes
|
|
|
T/F: uremia can lead to metabolic alkalosis?
|
False: metabolic acidosis
|
|
|
What electrolyte imbalances are seen in uremia? This can cause what?
|
Hyperkalemia & hypocalcemia w/c can cause arrhythmias & mm weakness
|
|
|
What endocrine changes are seen in uremia?
|
Renal osteodystrophy due to calcium disturbances/2° hyperparathyriodism, anemia
|
|
|
What other things can be seen w/ uremia?
|
Anorexia, pericarditis, uremic encephalopathy, inflammation, atherosclerosis
|
|
|
What are the leading causes of CKD?
|
DM & HTN
|
|
|
What is the mortality rate of ARF?
|
>50%
|
|
|
Number of Americans that suffer from kidney stones?
|
One million between 20-40 yrs of age
|
|
|
Number of pts suffering from CKD? # that die?
|
26 million w/ 90,000 die each yr
|
|
|
As many as ______% of the nephrons may need to be destroyed before significant functional impairment (clinical) is seen?
|
90%
|
|
|
A person is generally asymptomatic until how much of the renal function is lost?
|
>60%
|
|
|
What needs to be done for Dx?
|
Must ID subclinical diagnostics by different testing procedures such as urine analysis or renal biopsy & others.
|
|
|
What are 6 biochemical assessments that can be done to assess renal fxn?
|
1. Proteinuria ( a problem if >150mg/day)
2.hematuria 3. H ion [ ] (normal is 4.5-8 4.specific gravity 5. GFR 6. Tubular fxn test |
|
|
What does it mean if there is hematuria? How do u test for it?
|
Suggestive of dzs of lower urinary tract or renal dz. Can test for it by dipstick test or microscopic exam
|
|
|
What does it mean to have proteinuria? How do u test for it?
|
Suggestive of glomerular problem. Can test by dipstick
|
|
|
What is normal urine pH? How do u test?
|
4.5-8. Tested by dipstick
|
|
|
Changes in pH occur in w/c cases?
|
Increases after a meal (alkaline tide) & decreases during sleep (hypoventilation) & fever (metabolic acidosis)
|
|
|
In what condition is there an acidic urine? Alkaline?
|
Uric acid in gout & alakaline w/ phosphate stone w/c is suggestive of UTI
|
|
|
What is the normal specific gravity?
|
1.010-1.025
|
|
|
What is specific gravity in dehydration?
|
Could go up to 1.040
|
|
|
Specific gravity is a measurement of what?
|
Osmolarity
|
|
|
What happens to specific gravity in CKD? What is a sign of this?
|
Kidney loses ability to [ ] urine first in chronic renal disease, then lose ability to dilute urine. Nocturia is one of the 1st signs to be seen w/ this
|
|
|
Relate BUN to GFR?
|
As GFR decreases, BUN will increase
|
|
|
[ ] & dilution tests measure what?
|
Specific gravity
|
|
|
What is the [Na] test?
|
restrict Na in diet – urine should be free of Na. If loss more than ingest – problem.
|
|
|
What is the urine acidication test?
|
5 day test – control testing – challenge with NH4Cl check pH.
|
|
|
What is the most common abnormal microscopic examinations?
|
RBC >1-2/field, WBC 3-4/field, bacteria, & cast (these are muco protein matrix w/ cells & debris
|
|
|
What are the 5 types of casts?
|
Hyaline, RBC, WBC, fatty, broad or ganular
|
|
|
These casts are devoid of cells; they are clear cylinders of protein?
|
Hyaline
|
|
|
These casts come from leaking glomeruli
|
RBC casts
|
|
|
These casts come from infection & often seen in pylonephritis?
|
WBC casts
|
|
|
These casts are seen in nephrotic syndrome?
|
Fatty casts
|
|
|
These casts contain dead cells, they are formed in the collecting ducts & are typical of ESRF?
|
Broad or granular casts
|
|
|
What is IVP & what can it show?
|
Intravenous pyelogram w/c is a contrast media given IV & then x rays are taken. It can show cortex of kidney & can also establish size, shape & location of kidneys
|
|
|
What pathology can IVPs show?
|
Presence of cysts, lesions or obstruction & cortex thinness & thickness
|
|
|
If cortex is thin on IVP, what does it mean? If cortex has moth eaten appearance?
|
Thin: indicates glomerulonephritis. If moth eaten appearance: indicates pylonephritis or ischemia
|
|
|
What is a retrograde pyelogram?
|
A catheter is advanced up the ureter & a contrast media is injected into the renal pelvis
|
|
|
w/c radiologic test is useful for transplantations?
|
Renal angiography
|
|
|
What is the renal angiography?
|
A catheter is advanced via the femoral artery to the level of the renal artery
|
|
|
What pathology can a renal angiography detect?
|
Areterial stenosis, presence of neoplasms, & arrangement of arteries & veins
|
|
|
This is a way to Dx diffuse renal dz?
|
Renal biopsy
|
|
|
This can see problems w/ intrarenal bleeding?
|
Renal biopsy
|
|
|
This type of ARF usually reflect abnormal renal blood flow or myocardial dysfunction?
|
Pre-renal
|
|
|
This type of ARF is from a parenchymal injury?
|
Renal
|
|
|
This type of ARF is usually some type of tubular obstruction that interferes w/ elimination of urine from the kidney?
|
Post renal
|
|
|
What is the most common cases in ARF?
|
80-95% are pre-renal or renal in nature
|
|
|
ARF is usually manifested by a fall in urine output to < ________. The clinical syndrome is characterized by a sudden __________ in GFR.
|
400ml/day, decrease
|
|
|
Causes of ARF?
|
Ischemia & nephrotoxic injury
|
|
|
In order for the kidney to excrete the daily load of metabolic wastes three conditions must prevail?
|
1.The Kidney must be adequately perfused with blood. 2. The kidney must function normally. 3. Urine formed must be able to leave the body
|
|
|
Autoregulation can be overcome in conditions of ________ __________ ________if pressure to the kidney < ___mmHg.
|
severe volume depletion, <65mmHg
|
|
|
What are the causes of severe volume depletion?
|
Hemorrhage, GI or renal losses (loss of lytes), excessive diuretics, burns, & heat prostration, dehydration
|
|
|
What happens to the kidneys when there is volume loss?
|
kidney vessels vasoconstrict (NE, AngII, etc) and renal blood flow and GFR fall (whether CO falls or not) and this results in a “pre-renal” state.
|
|
|
Pre-renal azotemia is commonly caused by loss of what?
|
ECF; Fluid doesn’t actually have to be lost – this could occur due to a volume shift of fluid out of the extracellular spaces (decrease in vascular filling).
|
|
|
What happens to the kidneys w/ vasodilating drugs?
|
the volume of fluid is constant but the volume of distribution is expanded – less to kidney.
|
|
|
Give 3 examples of edematous states that can lead to ARF?
|
CHF, nephrotic syndrome, & cirrhosis
|
|
|
How does CHF contribute to ARF?
|
There will be a decrease in CO & therefore a decrease in GFR
|
|
|
How does cirrhosis contribute to ARF?
|
There is a drop in vascular volume & increase in interstitial volume
|
|
|
T/F:The drop in vasuclar volume in cirrhosis is d/t the hyperprotenemia?
|
False it’s hYPOprtenemia
|
|
|
What is the normal ratio of BUN: creatinine? What is the ratio in ARF?
|
Normal: 10:1 but w/ ARF it’s 20:1. Since GFR has decreased, more urea is not being excreted therefore it increases BUN
|
|
|
W/ pre-renal ARF, there is a marked decrease in GFR, what does this do to Na & water?
|
The kidney will conserve salt & water so there will be low excretion of sodium (<1%) so it can maintain BP.
|
|
|
T/F: w/ pre-renal ARF, u will find protein in the urine?
|
FALSE; since the kidneys are normal, there won’t be any protein in the urine
|
|
|
What 2 signs will be seen in pre-renal ARF?
|
1)rapid pulse, 2) low BP,
|
|
|
What meds should be avoided in ARF? Why?
|
NSAIDS b/c they inhibit PG synthesis. PG is a vasodilator & when u inhibit it w/ NSAIDS, ischemia is potentiated & PX worsened.
|
|
|
What is the best treatment for ARF?
|
Restore the adequate volume w/ whole blood or isotonic fluids
|
|
|
What is the Px for oliguria as a result of CHF or cirrhosis?
|
It implies a severe dz w/ poor px
|
|
|
How can u differentiate pre-renal azotemia from tubular necrosis? What is seen?
|
Urine osmolarity fractional excretion of Na. In pre-renal azotemia reabsorption capacity of tubules are maintained while necrosis this fxn is lost & therefore unable to [ ] urine
|
|
|
What are 4 potential causes of pre-renal conditions leading to ARF?
|
1) hypovolemia, 2) decreased vascular filling, 3) HF & cardiogenic shock, 4) decreased renal perfusion d/t vasoactive mediators, drugs or diagnostic agents
|
|
|
This is caused by an acute obstruction that affects the normal flow of urine out of both kidneys?
|
Postrenal ARF
|
|
|
The degree of renal failure corresponds to what?
|
Degree of obstruction
|
|
|
Postrenal ARF is seen most often in who?
|
Elderly men w/ enlarged prostate glands that obstruct the normal flow of urine
|
|
|
This is a condition in which the flow of urine is blocked, causing it to back up and injure one or both kidneys?
|
Obstructive uropathy
|
|
|
What is seen in obstructive uropathy?
|
Oliguria or anuria if both kidneys obstructed & polyuria if there is partial obstruction.
|
|
|
T/F: anuria is rarelly seen in pre-renal or renal parenchymal dz?
|
True
|
|
|
Post renally, obstruction can occur where?
|
Various levels like the bladder, the outlet, the level of the ureter, the prostate
|
|
|
Can obstruction of bladder cause ARF? Why or why not?
|
Rarely unless one of the kidneys is already destroyed or only have one kidney
|
|
|
This condition is more difficult to Dx & urinalysis may be of little to no help?
|
Post-renal ARF
|
|
|
This may be the only type of acute renal failure where urinalysis may be normal.
|
Post renal ARF
|
|
|
What is the Tx of post renal obstruction?
|
Relief of the obstruction
|
|
|
W/ relief of obstruction, there is profound diuresis, why is this?
|
Buildup of urea & other metabolites during the obstruction. Can have accumulation of excess salt & water & tubular defects caused by the obstruction.
|
|
|
After obstruction relief, how long can polyuria last?
|
A few hours to a few days
|
|
|
After obstruction, what is the urine osmolarity?
|
It’s isomolar w/ plasma; ½ of it is urea & the other ½ electrolytes
|
|
|
Caused by a variety of mechanisms that damage structures within the kidney (glomerular, tubular or interstitial?
|
Renal parenchymal dz
|
|
|
What are some causes of renal parenchymal dz?
|
Immunological, allergic, obstruction & subsequent necrosis, ischemic, & toxic substances
|
|
|
W/c renal parenchymal dz is common in hospital admits? Why?
|
Ischemic – common in hospital admits – kidney itself sustains no damage but if blood flow is blocked or reduced for over 40 min can result in acute tubular damage.
|
|
|
w/c renal parenchymal dz occurs following uric acid pp in hyperuricemia?
|
Obstruction & subsequent necrosis
|
|
|
80% of cases of renal fall in what category?
|
Acute tubular necrosis
|
|
|
The tubular epithelial cells are sensitive to ________?
|
Anoxia
|
|
|
What patho can happen w/ tubular damage?
|
Vasoconstriction to decrease GFR & damage itself can result in oliguria since tubular debris can block urinary outflow
|
|
|
What happens if person survives ATN?
|
will get regeneration of the epithelial cells – the recovery is nearly 100% if there is no basement membrane damage.
|
|
|
What are the 2 most damaging effects of urinary obstruction?
|
1) stasis of urine
2) & progressive dilation of the renal collecting ducts & renal tubular structures |
|
|
Why can stasis of urine have damaging effects
|
predisposes to infection & stone formation
|
|
|
Why can dilation of the tubules cause damaging effects?
|
b/c it causes destruction & atrophy of renal tissue
|
|
|
Of the 3 renal dz, pre, post & renal, w/c has the worst Px?
|
Renal b/c it’s intrinsic to the kidneys
|
|
|
ARF is a common threat to w/c group of people?
|
Seriously ill persons in ICU w/ mortality ranging from 40-75%
|
|
|
What is the most common indicator of ARF?
|
Azotemia
|
|
|
An accumulation of nitrogenous wastes in the blood & decrease in GFR?
|
azotemia
|
|
|
ATN is characterized by what?
|
destruction of tubular epithelial cells w/ acute suprression of renal function
|
|
|
WHat are the causes of ATN?
|
1) ischemia
2) sepsis 3) nephrotoxic effects of drugs 4) tubular obstruction 5) toxins from massive infection |
|
|
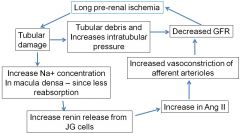
What happens w/ long pre-renal ischemia. Know the flow chart
|
|

