![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
36 Cards in this Set
- Front
- Back
|
What percent of Pf cases are severe and what is the mortality rate?
|
~10% of falciparum malaria cases → severe disease
mortality rate of 10-50% complications can develop rapidly several complications can occur simultaneously |
|
|
What are the complications of Pf malaria?
|
*cerebral malaria
*severe anemia *respiratory distress (pulmonary edema) hyperpyrexia hypoglycemia acidosis/hyperlactemia GI and liver syndromes (jaundice) renal failure (black water fever) circulatory collapse (shock) *most common The high parasitemia and sequestration can result in various complications and severe malaria encompasses a complex syndrome affecting many organs and resulting in biochemical and hematological abnormalities |
|
|
Regarding Pf malaria respiratory distress, why is it so important and what causes it?
|
respiratory distress due to metabolic acidosis
characterized by difficult and rapid breathing can progress to respiratory failure best predictor of death |
|
Identify the major complications of Pf malaria and describe the % mortality (numbers)
|
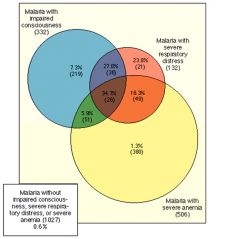
severe anemia>impared consciousness>severe respiratory distress
|
|
|
Why does Pf malaria have such high parasitemias?
|
all erythrocytes invaded
- Pv/Po = reticulocytes - Pm = senescent RBC up to 36 merozoites sequestration of infected erythrocytes - trophozoite and schizont stages - primarily in brain, heart, lungs, and gut - immune evasion (spleen avoidance) |
|
|
Why does Pf malaria have such severe anemia?
|
The severe anemia is due in part to the destruction of erythrocytes during
parasite maturation and merozoite release. In addition, noninfected erythrocytes are destroyed at higher rates in infected persons as a result of complement-mediated lysis and phagocytosis. This increase in complement activation and phagocytosis may be due to the high levels of antibodies observed during infection and the deposition of antibody complexes on the uninfected erythrocytes. Accordingly, severe anemia is more common in children from highly endemic areas because of repeated or chronic infections. Furthermore, there is a decreased production of erythrocytes during infection. This decrease in erythropoiesis may be due to the higher levels of cytokines and other mediators of inflammation which are known to affect the maturation of erythroid cells. |
|
|
What is a better predictor of death in Pf malaria, cerebral edema, severe anemia or respiratory distress? Why?
|
More recently it has been recognized that metabolic acidosis (i.e., low blood pH) as manifested by respiratory distress has emerged as a central
feature of severe malaria and is a better predictor of death than cerebral malaria or severe anemia. The first signs of lung injury are rapid and difficult breathing and are indicative of pulmonary edema (i.e., fluid in the lungs). This pulmonary edema can progress to an acute respiratory distress syndrome and even respiratory failure. |
|
|
Describe Pf malaria induced cerebral malaria and what causes it.
|
Cerebral malaria is characterized by an impaired consciousness and other neurological symptoms.
Patients typically present with fever for several days followed by a loss of consciousness. The onset of cerebral malaria can be gradual or rapid. The presenting symptoms are usually severe headache followed by drowsiness, confusion, and ultimately an unrousable coma. Convulsions, vomiting, and respiratory distress are also frequently associated with cerebral malaria, especially in children. neurological manifestations are believed to be due to the sequestration of the infected erythrocytes in the cerebral microvasculature. |
|
|
Pathology of all species of malaria is related to what?
|
Pathology associated with all malarial species is related to the rupture of
infected erythrocytes and the release of parasite material and metabolites, hemozoin (i.e., malaria pigment), and cellular debris. In addition, there is an increased activity of the reticuloendothelial system as evidenced by macrophages containing ingested infected and normal erythrocytes and hemozoin. Furthermore, the liver and spleen are often enlarged during malaria. |
|
|
What pathologic features contribute to severe Pf malaria?
|
Cytoadherence and sequestration are also believed to contribute to the
pathology of severe falciparum malaria. Sequestration refers to the cytoadherence of trophozoite- and schizont-infected erythrocytes to endothelial cells of deep vascular beds in vital organs, especially brain, lung, gut, heart, and placenta. As discussed above, this sequestration provides several advantages for the parasite and contributes to the high parasitemias. In addition, this cytoadherence and sequestration can have pathological effects on the specific organs, most notably the brain. |
|
|
What are "knobs"?
|
The parasite ligands are focused in electron-dense protuberances,
or “knobs,” on the surface of the infected erythrocyte. Receptor–ligand interactions between protein ligands expressed on the surface of trophozoite and schizont-infected erythrocytes and various receptors found on endothelial cells mediate cytoadherence knobs are restricted to P. falciparum and this suggests that the knobs play a role in cytoadherence. In addition, there is also a good correlation between animal Plasmodium species which express knobs and exhibit sequestration. |
|
How does Pf contribute to severe malaria? name labeled areas
|
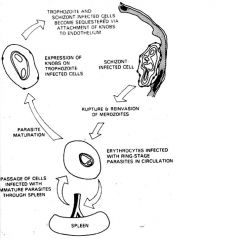
avoidance of spleen
low oxygen tensions better invasion complications sequestration in the tissues minimizes removal of infected erythrocytes by the spleen and can be viewed as an avoidance of the immune system. In addition, the cytoadherence to the endothelial cells of the capillaries allows for a more efficient erythrocyte invasion because the blood flow is much slower. The low oxygen tension found in the deep tissues is also metabolically favorable for parasite growth. |
|

What are the parasite proteins associated with knobs?
|

KAHRP and PfEMP2 are believed to interact with the submembrane cytoskeleton of the host erythrocyte
reorganization of the membrane skeleton may result in knob formation PfEMP1 crosses the erythrocyte membrane and is exposed on the surface Parasite proteins are associated with the knobs found on the surface of infected erythrocytes. These proteins probably cause a reorganization of the submembrane cytoskeleton of the erythrocyte and are important in the cytoadherence of the infected erythrocyte to host endothelial cells. |
|
|
What parasite proteins do are not exposed on the outer surface of the outer surface of an erythrocye?
|
Two proteins which probably participate in
knob formation are the knob-associated histidine rich protein (KAHRP) and erythrocyte membrane protein-2 (PfEMP2). Neither KAHRP nor PfEMP2 are exposed on the outer surface of the erythrocyte, but are localized to the cytoplasmic face of the host membrane |
|
|
What parasite protein is exposed to the outer surface of the erythrocyte membrane?
|
A polymorphic protein, called PfEMP1, has also been localized to the knobs and is exposed on the host erythrocyte
surface and probably functions as a ligand which binds to receptors on host endothelial cells. |
|
|
PfEMP1 is related to what gene family?
|
PfEMP1 corresponds to members of the var gene family.
family of ~60 var genes |
|
|
What are the three main structures in PfEMP1?
|
PfEMP1 has a large extracellular N-terminal domain,
transmembrane region C-terminal intracellular domain. |
|
|
What does the C-terminal region do?
|
conserved intracellular C-terminus
- acidic terminal segment (ATS) - binds cytoskeleton + KAHRP The C-terminal region is conserved between members of the var family and is believed to anchor PfEMP1 to the erythrocyte submembrane cytoskeleton. In particular, this acidic C-terminal domain may interact with the basic KAHRP of the knob as well as spectrin and actin of the submembrane cytoskeleton. |
|
|
What does the extra-cellular domain do?
|
variable extracellular domain composed of modules
- 2-7 copies of Duffy-binding like domains - - - 5 sequence types (a, b, g, d, e) - 1-2 cys-rich interdoma in regions - all have DBL1a + CIDR The extracellular domain is characterized by one to five copies of Duffy-binding-like (DBL) domains. These DBL domains are similar to the receptor-binding region of the ligands involved in merozoite invasion The DBL domains exhibit a conserved spacing of cysteine and hydrophobic residues, but otherwise show little homology. Phylogenetic analysis indicates that there are five distinct classes (designated as a, b, g, d, and e) of DBL domains. The first DBL is usually a DBLa type and this is followed by a cysteine-rich interdomain region (CIDR). A variable number and types of DBL domains in various orders make up the rest of the extracellular domain of PfEMP-1. |
|
|
How does Pf avoid the spleen?
|
Infected parasites (IRBC) can't filter through
|
|
|
What are the possible host receptors allowing PfEMP1 to bind to different domains?
|
CD36
Ig super-family - ICAM-1 - VCAM-1 - PECAM-1 E-selectin thrombospondin chondroitin sulfate A hyaluronic acid Rosetting Receptors Several possible endothelial receptors have been identified by testing the ability of infected erythrocytes to bind in static adherence assays.Detailed analysis of the binding activity of PfEMP1 to the receptors indicates that different domains of PfEMP1 are responsible for binding to different receptors. For example, CD36, an 88 kDa integral membrane protein found on monocytes, platelets, and endothelial cells binds to the CIDR domain. Similarly, the different classes of DBL domains bind to different endothelial cell receptors. |
|
|
What PfEMP1 domain does CD36 host receptor bind to?
What disease process is it known for? |
cysteine-rich
interdomain regions (CIDR) |
|
|
What PfEMP1 domain does Intracellular adhesion
molecule-1 (ICAM1) host receptor bind to? |
DBLb Implicated in cerebral malaria
ICAM1 is a member of the immunoglobulin superfamily and functions in cell–cell adhesion. As discussed above, binding of infected erythrocytes to ICAM1 is speculated to play a role in the development of cerebral malaria. |
|
|
What PfEMP1 domain does Complement receptor-1host receptor bind to?
This is part of what special receptor? |
Duffy-binding-like
(DBL) domain - DBLa Rosetting receptor |
|
|
What PfEMP1 domain does Chondroitin sulfate A host receptor bind to?
Where in the host is this receptor found? |
DBLy
Receptor in the placenta |
|
|
What are the Ig super-family host receptors?
|
ICAM-1
VCAM-1 PECAM-1 Of importance, ICAM1 is a member of the immunoglobulin superfamily and functions in cell–cell adhesion. As discussed above, binding of infected erythrocytes to ICAM1 is speculated to play a role in the development of cerebral malaria. |
|
|
What are the rosetting receptors in host receptors?
|
Complement receptor-1 (CR-1)
glycosaminoglycan blood group A |
|
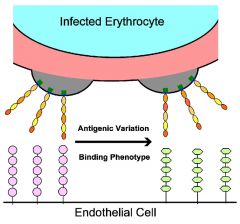
How does the parasite to avoid clearance by
the host immune system but maintain the cytoadherent phenotype? |
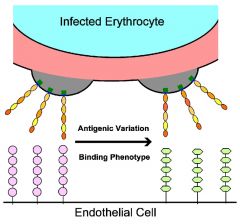
Antigenic variation.
Changes in the expression of PfEMP1 alleles will result in an infected erythrocyte with a different binding phenotype as well as a different antigenic type. the expression of antigens on the surface of the infected erythrocyte provides a target for the host immune system. The parasite counters the host immune response by expressing antigenically distinct PfEMP1 molecules on the erythrocyte surface, thus allowing the parasite to evade the immune system. Several studies have indicated that the expression of different PfEMP1 genes correlates with different receptor-binding phenotypes. Thus, the cytoadherence function is preserved through its ability to recognize multiple receptors This allows the parasite to avoid clearance by the host immune system but maintain the cytoadherent phenotype. |
|
|
What is the Sequestration Hypothesis?
|
cytoadherence --> cerebral ischemia --> hypoxia, metabolic effects --> coma --> death
cytoadherence would lead to a mechanical blockage (i.e., cerebral ischemia) and subsequently hypoxia. In addition, the parasite exhibits a high level of glycolysis which could cause localized metabolic effects such as hypoglycemia and lactic acidosis. The hypoxia and metabolic effects would then disrupt normal brain function and lead to coma and subsequent death. |
|
|
What are the problems with the Sequestration Hypothesis?
|
rapid reversibility
lack of ischemic damage low levels of permanent neurological damage sequestration occurs in non-cerebral malaria cases long-term neurological sequelae among survivors of cerebral malaria are lower than would be expected for ischemia and the coma associated with cerebral malaria is rapidly reversible upon treatment. |
|
|
What unexpected findings do you find with cerebral malaria survivors?
|
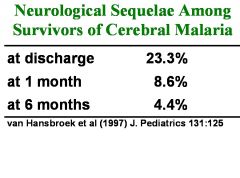
long-term neurological sequelae among survivors of cerebral
malaria are lower than would be expected for ischemia and the coma associated with cerebral malaria is rapidly reversible upon treatment. |
|
|
What is rosetting?
|
Rosetting is another adhesive phenomenon exhibited by P. falciparuminfected
erythrocytes which may play a role in pathogenesis. Some infected erythrocytes bind to multiple uninfected erythrocytes resulting in a large clump of erythrocytes, or a rosette. Some studies have shown an association between the rosetting phenotype and severe malaria. These clumps could restrict microvascular flow in a similar fashion as cytoadherence to endothelial cells and thus contribute to the pathology. |
|
|
What is the cytokine theory?
|
cytokines, such as
TNF-a, or short-lived intermediates, such as nitric oxide, are speculated to be responsible for the pathology. In this cytokine theory, malarial antigens stimulate the production of TNF-a and other cytokines which could then induce nitric oxide or have other pathological effects. Nitric oxide is known to affect neuronal function and it could also lead to intracranial hypertension through its vasodilator activity. |
|
|
What are the problems with the cytokine theory?
|
minimal lymphocyte infiltration or inflammation
A capillary is filled with infected erythrocytes which are adhered to the brain endothelial cells with relatively little inflammation. It is unlikely, though, that the systemic release of cytokines would cause coma and there is minimal lymphocyte infiltration or inflammation associated with the blocked capillaries |
|
|
Pathological events that contribute to severe Pf Malaria
|
potentially high parasitemias
sequestration complex (and not fully understood) host-parasite interactions differential var gene expression? |
|
Are there differences in expression of var alleles in different organs?
|
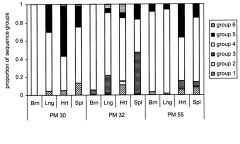
Frequency of PfEMP1 types
in organs of malaria patients. The organs of patients dying from severe malaria were analyzed for transcripts of var genes. The various types of PfEMP1 were grouped according to their sequences at positions of limited variability. Different types of PfEMP1 predominated in the various organs. Brain and lung have high amounts of group 4; heart group 5 |

