![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
|
The right coronary artery, how often does it give rise to
a. The posterior interventricular artery, and what is it called when it does b. SA node c. AV node |
a. 90%, dominant artery.
b. 60% c. 90% (Damjanov) |
|
|
The heart
a. Oxygen saturation in the right heart b. Oxygen saturation in the left heart c. Pressure in right atrium d. Pressure in right ventricle e. Pressure in Pulmonary artery f. Pressure in left atrium g. Pressure in left ventricle |
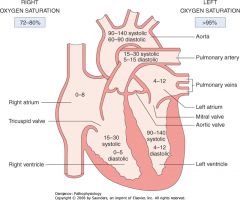
a. 75% (72-80%)
b. > 95% c. 0-8 mmHg d. 15-30 \ 0-5 mmHg e. 15-30 \ 5-15 mmHg f. 4-12 mmHg g. 120 \ 4-12 mmHg (Damjanov) |
|
|
Mechanism of conduction-contraction coupling in the cardiac myocytes
|
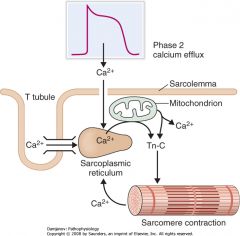
1. Entry from Ca from outside the cell during phase 2 acts as a trigger for discharge of large amounts of Ca stored inside SR and mitochondria
2. When the Ca concentration rise 10-fold contraction is initiated due to I. Ca binds to troponin C -> II. Inactivate troponin I -> III. Induce conformational change in troponin T and tropomyosin -> IV. Tropomyosin deblocks actin (Damjanov) |
|
|
Decreased contractility\inotropism
a. Causes b. Consequence c. What is the law that describe the relationship between cardiac output and preload |
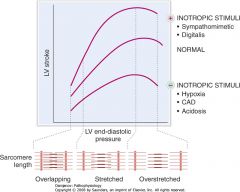
a. CAD, hypoxia, acidosis
b. The heart cannot increase CO in response to increased end-diastolic pressure\preload c. Frank-Starling law of the heart. (Damjanov) |
|
|
Conduction and contraction
a. Resting membrane potential of cardiac myocytes b. The five phases of the cardiac myocyte's action potential - Their name and the ionic flow |
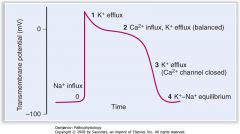
a. -90 mV
b. Phases of cardiac myocyte's action potential 1. Phase 0\Fast upstroke I. Opening of fast Na channels II. End when these are inactivated 2. Phase 1\Partial repolarization I. Inactivation of fast Na channels II. Rapid opening and closure of K channels 3. Phase 2\Plateau I. Opening of voltage-sensitive Ca channels II. Counterbalanced by slow K efflux 4. Phase 3\Repolarization I. Closure of Ca channels II. Efflux of K 5. Phase 4\Forward current I. Mild gradual depolarization due to Na influx accompanied by K efflux (Damjanov) |
|
|
Heart sounds
a. When can S3 be heard b. When can S4 be heard |
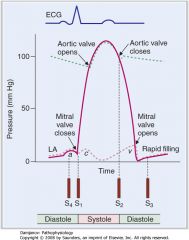
a. S3 - During the period of rapid ventricular filling.
b. S4 - Atrial contraction (Damjanov) |
|
|
Ischemia
a. What part of the heart receives oxygen and nutrients from the blood last b. When does this type of infarct usually develop c. Are the coronary arteries considered to be terminal arteries d. Paradoxical infarcts - What, mechanism |
a. Subendocardial myocardium.
(Subendocardial infarcts\non-Q wave infarcts) b. In shock and other hypoperfusion states. c. Yes (Are < 40 um anastomoses between them, these are only sufficient for collateral flow with chronic\slow-progressing stenosis) d. Paradoxical infarcts I. Infarcts that develop in the LCA supply zone due to a thrombus in the RCA and vice versa II. Consequence of stop of anastomoses due to gradual narrowing of the coronary artery that normally provides the blood to the infarcted area. (Damjanov) |
|
|
Risk factors for heart disease - Give specific disease and the risk factor association
a. Hereditary factors b. Social\Nutritional factors c. Aging d. Infections e. Medical and surgical procedures f. Drugs\toxins g. External mechanical factors (trauma) |
a. Hereditary factors
1. Hyperlipidemia -> Coronary heart disease 2. Familial hypertrophic cardiomyopathy 3. Hemochromoatosis -> Cardiomyopathy 4. Familial history of hypertension -> Hypertensive heart disease b. Social\Nutritional factors 1. Smoking -> Coronary heart disease 2. Drug abuse -> Endocarditis 3. Alcoholism -> Cardiomyopathy c. Aging 1. Atherosclerosis -> Coronary heart disease d. Infections 1. "Strep throat" -> Rheumatic fever 2. Systemic viral infection -> Myocarditis, Pericarditis e. Medical and surgical procedures 1. Sepsis -> Endocarditis f. Drugs\toxins 1. Adriamycin -> Cardiomyopathy 2. Alcohol abuse -> Cardiomyopathy g. External mechanical factors 1. Car accident -> Rupture of the aorta 2. Stabbing wound of the heart -> Hematopericardium (Damjanov) |
|
|
Signs and symptoms of heart disease
|
Signs and symptoms of heart disease
1. Chest discomfort and pain 2. Palpitations (Feel heart beats fast <- atrial fibrillation (rapid and irregular), supraventricular or ventricular tachycardia (rapid and regular), "skipping beats" <- premature atrial and ventricular contractions) 3. Dyspnea (From increased respiratory effort aimed at compensating for hypoxia) 4. Edema 5. Cyanosis 6. Syncope 7. Cardiac murmurs 8. Abnormal pulse 9. Jugular venous pulse 10. Hypertension (Damjanov) |
|
|
Major causes of chest discomfort and pain
|
Major causes of chest discomfort and pain
1. Cardiac pain I. Angina pectoris II. MI (Ischemic pain - normally has an epicenter over the sternum (retrosternal pain) radiating to the left arm (C8,T1 dermatome), neck, and lower jaw. Less commonly it occurs bilaterally or radiates to the back along the left scapula, often described as haeviness\pressure\squeezing behind the sternum) III. Aortic stenosis IV. Pericarditis (Typically most intense behind the sternum or at the apex of the heart, stabbing\burning\piercing, unrelated to exercise, aggregated by lying down, coughing\deep inspiration and movement, relieved (partially) by leaning forward or preventing chest movements) 2. Chest wall syndromes I. Herpes zoster II. Myalgias 3. GI pain I. Esophageal disorder II. Peptic ulcer disease III. Gallstones and cholecystitis 4. Pulmonary pain I. Pneumonia II. Pleuritis III. Pulmonary embolism 5. Vascular pain I. Aortic aneurysm II. Aortic dissection (Damjanov) |
|
|
Dyspnea
a. Which noncardiac causes should be ruled out b. Classification of cardiac dyspneas c. Symptoms associated with dyspnea |
a. Noncardiac dyspneas
1. Pulmonary - COPD, asthma, pneumonia 2. Drug-induced 3. Systemic 4. Neuromuscular diseases b. Cardiac dyspneas 1. High cardiac output I. Anemia II. Hyperthyroidism 2. Normal cardiac output I. Obesity 3. Low cardiac output I. CHF II. MI III. Valvular diseases IV. Pericarditis c. Symptoms associated with dyspnea 1. Orthopnea I. Breathing discomfort experienced while the patient is lying down that is relieved by sitting up or using several pillows 2. Paroxysmal nocturnal dyspnea I. Wakes the patient, which have a feeling of suffocation (May be associated with wheezing or coughing -> 'cardiac asthma') (Damjanov) |
|
|
Risk factors for heart disease - Give specific disease and the risk factor association
a. Hereditary factors b. Social\Nutritional factors c. Aging d. Infections e. Medical and surgical procedures f. Drugs\toxins g. External mechanical factors (trauma) |
a. Hereditary factors
1. Hyperlipidemia -> Coronary heart disease 2. Familial hypertrophic cardiomyopathy 3. Hemochromoatosis -> Cardiomyopathy 4. Familial history of hypertension -> Hypertensive heart disease b. Social\Nutritional factors 1. Smoking -> Coronary heart disease 2. Drug abuse -> Endocarditis 3. Alcoholism -> Cardiomyopathy c. Aging 1. Atherosclerosis -> Coronary heart disease d. Infections 1. "Strep throat" -> Rheumatic fever 2. Systemic viral infection -> Myocarditis, Pericarditis e. Medical and surgical procedures 1. Sepsis -> Endocarditis f. Drugs\toxins 1. Adriamycin -> Cardiomyopathy 2. Alcohol abuse -> Cardiomyopathy g. External mechanical factors 1. Car accident -> Rupture of the aorta 2. Stabbing wound of the heart -> Hematopericardium (Damjanov) |
|
|
Signs and symptoms of heart disease
|
Signs and symptoms of heart disease
1. Chest discomfort and pain 2. Palpitations (Feel heart beats fast <- atrial fibrillation (rapid and irregular), supraventricular or ventricular tachycardia (rapid and regular), "skipping beats" <- premature atrial and ventricular contractions) 3. Dyspnea (From increased respiratory effort aimed at compensating for hypoxia) 4. Edema 5. Cyanosis 6. Syncope 7. Cardiac murmurs 8. Abnormal pulse 9. Jugular venous pulse 10. Hypertension (Damjanov) |
|
|
Major causes of chest discomfort and pain
|
Major causes of chest discomfort and pain
1. Cardiac pain I. Angina pectoris II. MI (Ischemic pain - normally has an epicenter over the sternum (retrosternal pain) radiating to the left arm (C8,T1 dermatome), neck, and lower jaw. Less commonly it occurs bilaterally or radiates to the back along the left scapula, often described as haeviness\pressure\squeezing behind the sternum) III. Aortic stenosis IV. Pericarditis (Typically most intense behind the sternum or at the apex of the heart, stabbing\burning\piercing, unrelated to exercise, aggregated by lying down, coughing\deep inspiration and movement, relieved (partially) by leaning forward or preventing chest movements) 2. Chest wall syndromes I. Herpes zoster II. Myalgias 3. GI pain I. Esophageal disorder II. Peptic ulcer disease III. Gallstones and cholecystitis 4. Pulmonary pain I. Pneumonia II. Pleuritis III. Pulmonary embolism 5. Vascular pain I. Aortic aneurysm II. Aortic dissection (Damjanov) |
|
|
Dyspnea
a. Which noncardiac causes should be ruled out b. Classification of cardiac dyspneas c. Symptoms associated with dyspnea |
a. Noncardiac dyspneas
1. Pulmonary - COPD, asthma, pneumonia 2. Drug-induced 3. Systemic 4. Neuromuscular diseases b. Cardiac dyspneas 1. High cardiac output I. Anemia II. Hyperthyroidism 2. Normal cardiac output I. Obesity 3. Low cardiac output I. CHF II. MI III. Valvular diseases IV. Pericarditis c. Symptoms associated with dyspnea 1. Orthopnea I. Breathing discomfort experienced while the patient is lying down that is relieved by sitting up or using several pillows 2. Paroxysmal nocturnal dyspnea I. Wakes the patient, which have a feeling of suffocation (May be associated with wheezing or coughing -> 'cardiac asthma') (Damjanov) |
|
|
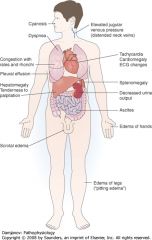
Heart failure
a. Consequences of left heart failure b. Consequences of right heart failure |
a. Left heart failure
1. Backlow pressure into the pulmonary system -> 2. Pulmonary edema -> (This hydrostatic edema may be of acute onset, as in MI, or chronic, as in CHF, pulmonary rales, chronic is associated with hydrothorax (water in pleural cavity)) 3. Increased pulmonary artery pressure -> 4. Cor pulmonale (Left heart failure is the most common cause of right heart failure) b. Right heart failure 1. Right ventricular dilatation and hypertrophy -> 2. Increased JVP and central venous pressure -> 3. Several I. Congestive hepatomegaly and splenomegaly (-> Pain in liver or spleen, epigastric fullness) II. Ascites (-> Bulging abdomen, changes in bowel habits) III. Pedal edema ("Pitting leg edema") IV. Anasarca (Generalized edema, fluid retention is an essential element) (Damjanov) |
|
|
Cyanosis
a. Cyanosis - What, caused by b. Types and causes |
a. Cyanosis
I. Bluish discoloration of skin or mucosa II. Caused by increased concentration of deoxygenated hemoglobin in the blood - > 5g\dL (Practically with saturation < 85%) b. Cyanosis 1. Central cyanosis I. Discoloration of lips and trunks I. <- Pulmonary diseases (most common in adults), congenital heart diseases with right-to-left shunts (most common in children), hemoglobin abnormalities, high altitude 2. Peripheral cyanosis I. Bluish discoloration of finger and toes II. <- Cold, Raynaud's disease, Buerger's disease, thrombi (venous or arterial), decreased cardiac output (Children -> most often by congenital heart disease with right-to-left shunt) (Buerger disease\Thromboangiitis obliterans - Inflammation of the entire wall and connective tissue surrounding medium-sized arteries and veins, especially of the legs of young and middle-aged men, associated with thrombotic occlusion and commonly result in gangrene) (Damjanov) |
|
|
Syncope - The four categories of causes
|
Syncope
1. Orthostatic hypotension I. Hyperadrenegic (<- Volume depletion) II. Hypoadrenergic (<- Autonomic dysregulation as in DM, familial dysautonomia, drugs affecting ANS - centrally acting hypotensive drugs (methyldopa), adrenergic neuron-blocking agents (guanethidine), tranquilizers, antidepressants..) (Can cause postprandial syncope in the elderly (syncope after meals)) 2. Reflex neurocardiogenic syncope - Situational (<- Reflex-induced vasodilation or bradycardia <- carotid-sinus reflex or vasovagal reflex (can be triggered by coughing, straining, micturition and defecation, or exercise) 3. TIA\Seizure\Epilepsy\Migraines - Neurologic disorders 4. Heart conditions I. MI - Pump failure II. Valvular disease - Obstruction of flow III. Conduction disorders (Bradycardia, arrhythmia) IV. Drugs - Nitroglycerin 4. Other causes I. Metabolic diseases - Hypoglycemia II. Hyperventilation from excitement, hysteria, and other psychiatric disorders (Idiopathic in 30% of cases) (Mnemonic - the first five letters of orthostatic - ORTHO) (Damjanov) |
|
|
Principal mechanisms by which chemical messengers in the ECF bring about changes in cell function, include examples
|
Principal mechanisms by which chemical messengers in the ECF bring about changes in cell function
1. Open or close ion channels in the cell membrane I. Acetylcholine on nicotinic cholinergic receptors II. Norepinephrine on K channels in the heart 2. Act via cytoplasmic or nuclear receptors to increase transcription of selected mRNAs I. Thyroid hormones II. Retinoic acid III. Steroid hormones 3. Activate PLC with intracellular production of DAG and IP3 I. ATII II. Norepinephrine via alpha-1 adrenergic receptor III. Vasopressin via V1 receptor 4. Activate or inhibit adenylyl cyclase, causing increased or decreased intracellular production of cAMP I. Norepinephrine via beta-1 adrenergic receptor (stimulate) II. Norepinephrine via alpha-2 adrenergic receptor (inhibit) 5. Increase cGMP in cell I. ANP II. NO (Via EDRF - endothelium-derived relaxing factor) 6. Increase tyrosine kinase activity of cytoplasmic portions of transmembrane receptors I. Insulin II. Epidermal growth factor (EGF) III. PDGF IV. Macrophage colony-stimulating factor (M-CSF) 7. Increase serine or threonine kinase activity I. TGF-beta II. MAPKs (Ganong) |
|
|
Cardiac murmurs - Causes of
a. Mid-systolic\Crescendo-decrescendo murmurs b. Pansystolic murmurs c. late-systolic murmurs |
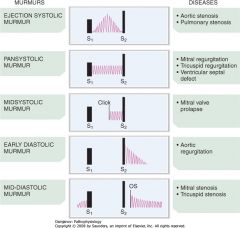
a. Mid-systolic\Crescendo-decrescendo murmurs
1. Aortic stenosis 2. Pulmonary stenosis 3. Hypertrophic cardiomyopathy b. Pansystolic murmurs 1. Mitral regurgitation 2. Tricuspid regurgitation 3. VSD c. Late-systolic 1. Mitral valve prolapse (Damjanov) |
|
|
Cardiac murmurs - Causes of
a. Early diastolic murmurs b. Mid-diastolic murmurs c. Continuous stenosis |
a. Early diastolic murmurs
1. Aortic regurgitation 2. Pulmonary regurgitation b. Mid-diastolic murmurs 1. Mitral stenosis 2. Tricuspid stenosis c. Continuous murmurs 1. Patent ductus arteriosus (Damjanov) |
|
|
Pulse - Shape of
a. Normal pulse b. Anacrotic pulse\Pulsus parvus et tardus c. Pulsus bisferiens\Pulsus celer d. Pulsus paradoxus |

a. Normal pulse - dicrotic
I. A normal pulse has two peaks separated by a dicrotic notch (Dicrotic notch - the acute drop followed by a rise in arterial pressure pulse curves following the systolic peak) b. Anacrotic pulse\Pulsus parvus et tardus I. The initial upstroke is slow and the peak is lower than normal (Typical of aortic stenosis) c. Pulsus bisferiens\Pulsus celer I. Two systolic peaks (Typically occurs in aortic regurgitation, the volume of such a pulse is larger than normal) d. Pulsus paradoxus I. Decline in pulse during inspiration of > 10 mmHg (<- Cardiac tamponade or constrictive pericarditis) (Damjanov) |
|
|
Hypertension
a. Primary - What, % of cases b. Secondary - What, causes |
a. Primary hypertension
I. Unknown cause II. 95% of cases b. Secondary hypertension I. Produced by a known cause II. Causes 1. Renal (Glomerulonephritis (acute, chronic), diabetic neuropathy, renal artery stenosis) 2. Endocrine (Hyperfunction of tumors of pituitary, thyroid, parathyroid, adrenal cortex, pheochromocytoma, carcinoid tumors, exogenous hormones (ie steroids)) 3. Neurogenic (Increased ICP (CNS tumors, infection), Guillain-Barre syndrome, sleep apnea) 4. Arterial (Atherosclerosis, coarctation of aorta, aortitis) 5. Labile or laboratory abnormalities (White coat hypertension\labile hypertension, psychogenic nervousness, postoperative, hypoglycemia, sickle cell anemia, drugs (cocaine, NSAIDs), pregnancy) (Mnemonic: RENAL) (Damjanov) |
|
|
Radiologic techniques - Which parameters does standard AP and lateral radiographs provide information about
|
Routine chest radiography
1. Shape of the heart (Boot-shaped in tetralogy of Fallot) 2. Size of the heart (Hypertension, various cardiomyopathies) 3. Size of cardiac chambers 4. Pulmonary circulation (Pulmonary congestion and edema that occur in left heart failure are easily recognized) 5. Pulmonary disease (COPD that may cause cor pulmonale is easily recognized) 6. Aortic pathology (Atherosclerosis, aneurysmal dilatations) (Radionucleotide imaging is widely used for assessing the thickness of the ventricles and evaluating cardiac functioning) (Damjanov) |
|
|
ECG - Which electrodes detect changes in
a. (Left) Anterolateral part of the heart b. Inferolateral part c. Right ventricle d. Septum e. Anterior and lateral wall of the left ventricle |
a. Anterolateral part
I. aVL (Left arm-indifferent electrode (right arm + right leg. -30) II. I (Left arm-right arm. 0) b. Inferolateral changes I. II (left leg-right arm, 60) II. III (right leg-left arm, 120) c. Right ventricle I. V1 (Right sternal margin, 4th intercostal space) II. V2 (Left sternal margin, 4th intercostal space) d. Septum I. V3 (Halfway between V2 and V4) II. V4 (5th intercostal space in the left midclavicular line) e. Anterior and lateral walls of left ventricle I. V5 (5th intercostal space in the anterior axillary line) II. V6 (5th intercostal space in the midaxillary line) (Damjanov) |
|
|
ECG
a. ST segment b. Hypokalemia - Effect on ECG c. Hyperkalemia - Effect on ECG d. Hypocalcemia - Effect on ECG e. Hypercalcemia - Effect on ECG f. Digitalis - Effect on ECG g. Quinidine - Effect on ECG |
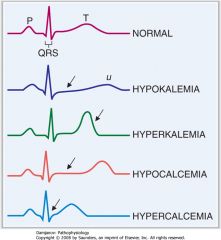
a. ST segment
I. Isoelectric segment following the QRS complex (Of equal electrical potential) II. Very little electrical activity in the heart during this period (-> Give clue about 'basal electrical state' of heart) b. Hypokalemia I. ST segment depression II. T wave depression c. Hyperkalemia I. T-wave peakening d. Hypocalcemia I. Prolong the QT interval (From beginning of Q to end of T, normally 0.35-0.45 sec) f. Digitalis I. ST depression II. T depression\flattening (Like hypokalemia g. Quinidine I. Prolong the T wave I. Depress\flat or invert the T wave (Damjanov) |
|
|
Laboratory testing for diagnosis of MI - Myoglobin
a. When is it released from damaged myocytes b. When does it peak c. When does it return to normal levels d. Pros and cons |
a. Within 2 hours after cell injury
b. 6-9 hours c. 24-36 hours (Its small molecular weight (17.8 kDa) is responsible for it being cleared mostly by the kidneys and this explains the short half-life) d. Pros I. Fast release after cell death (Fastest of all the tests) Cons I. Low specificity because myoglobin from skeletal and cardiac muscle are alike (Specificity is increased if there are no signs of skeletal muscle injury) (Damjanov) |
|
|
Creatine kinase
a. Types and their distribution b. When is the relevant CK released after injury to the myocytes c. When does it peak d. When does it return to normal levels |
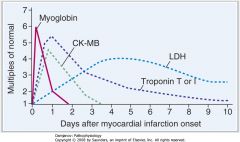
a. Creatine kinase
I. Dimer of M and B -> MM, BB, MB II. MB is found predominantly in the heart (20% is CK-MB, 80% is CK-MM) II. CK-MM predominate in skeletal muscle b. 4-8 hours c. 24 hours d. 72 hours (Damjanov) |
|
|
Troponins
a. Types b. Which are used as markers for myocyte damage c. Time of release after myocyte injury d. Peak d. Return to normal levels |
a. Troponins
I. Troponin T - Links the troponin compelx to tropomyosin II. Troponin I - Inhibitor of acomyosin ATPase III. Troponin C - Calcium-binding protein that regulate actin contraction b. Troponin T and I (Most specific markers for myocardial injury) c. 3-4 hours d. On the second day e. 5-6 days (Damjanov) |
|
|
Lactate dehydrogenase
a. Types and their distribution b. Which is measured c. Time of release after myocyte injury d. When does its levels peak e. When does it return to normal levels |
a. Lactate dehydrogenases - 5 isoenzymes
I. LDH1 - Cardiac primarily 2. LDH2 - Erythrocytes 3. LDH3 - Unspecific for many organs 4. LDH4 and 5 - Mostly from liver and skeletal muscle b. Total serum LDH is measured, sometimes ratios are measured as well (Ratio of LDH1\LDH2 > 1 is typical of MI) c. Rise slowly d. 4-5 days e. 9-10 days (Relatively nonspecific marker) (Damjanov) |
|
|
Ischemic heart disease
a. Synonym b. Principal cause c. Risk factors - Modifiable and unmodifiable |
a. Ischemic heart disease\Coroanry artery disease (CAD)\Atherosclerotic coronary heart disease
b. Principal cause - Atherosclerosis c. Risk factors Unmodifiable\Fixed 1. Age (Its prevalence decrease dramatically after age 60) 2. Sex (More common in men, almost similar prevalence after menopause in women) (Damjanov) 3. Genetic and hereditary factors Modifiable\Preventable 1. Cigarette smoking 2. Hypertension 3. Hyperlipidemia 4. Diabetes mellitus |
|
|
Secondary hyperlipidemias - The most common and their predominant lipoproteins in the blood
|
Secondary hyperlipidemias
1. Diabetes mellitus I. TG II. VLDL, IDL 2. Hypothyroidism I. Cholesterol II. LDL 3. Nephrotic syndrome I. Cholesterol II. LDL 4. Alcohol abuse I. TG II. VLDL 5. Chronic renal failure I. TG II. VLDL 6. Drugs - ie thiazides I. TG II. VLDL (Classification by WHO and Fredrickson) |
|
|
Classification of primary hyperlipoproteinemias - Pathogenetic classification, lipids in blood, electrophoresis (dominant band)
a. Type I b. Type IIa c. Type IIb d. Type III e. Type IV f. Type V |
a. Type I - Lipoprotein lipase deficiency
I. Elevated cholesterol and triglycerides II. Chylomicron as dominant band b. Type IIa - LDL-receptor deficiency I. Cholesterol II. LDL c. Type IIb - Single-gene defects I. Cholesterol, triglycerides II. VLDL, LDL d. Type III - Apo E2 homozygosity I. Cholesterol, triglycerides II. VLDL remnants e. Type IV - Familial combined hyperlipidemia I. Triglycerides (Some cholesterol) II. VLDL f. Type V - Familial hypertriglyceridemia I. Triglycerides (some cholesterol) II. VLDL (Damjanov) |
|
|
Atherosclerosis - Pathogenesis
|
Atherosclerosis - Pathogenesis
1. Risk factors (hyperlipidemia, hypertension, smoking) cause endothelial damage and dysfunction 2. Endothelial injury facilitate insudation of LDL in the vessel wall 3. Monocytes migrate from the blood into the subendothelial intima and transform into macrophages. Phagocytose oxidized LDL by scavenger receptors and become foam cells (Foam cells form the lipid core of the atherosclerotic plaque) 4. Production of inflammatory mediators and cytokines -> Proliferation of smooth muscle cells of the vascular intima and fibroblasts, deposition of extracellular matrix molecules such as elastin and collagen -> Plaque expansion, fibrous cap 5. The fibrous cap can weaken and rupture and cause emboli-formation or thrombotic occlusion (medscape.com) |
|
|
Atheromas of the coronary arteries
a. Types and their characteristics, which disease are they associated with |
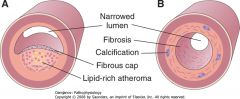
a. Atheromas of the coronary arteries
1. Soft atheroma\Vulnerable atheromas\Atheromas at risk I. Primarily composed of semiliquid lipid-rich material II. Covered on the luminal side by a thin fibrous cap which is prone to rupturing, this cause instantaneous thrombus formation and complete occlusion of the artery and MI 2. Hard atheroma\Stable atheroma I. Primarily fibrotic and calcified tissue (Oxidized lipids stimulate proliferation and calcification) II. Associated with chronic ischemic heart disease manifested as angina pectoris (The overlying endothelium lose its normal function and cannot secrete NO or other vasodilatory substances. The fibrous tissue, which is rich in collagen and calcifications, replaces the smooth muscle cells and impairs the capacity of the coronaries to dilate) (Damjanov) |
|
|
Angina pectoris
a. Definition b. Etiology c. Pain - Characteristics d. Pain - Location e. Triggered by |
a. Angina pectoris ('Pain of chest')
I. Chest pain caused by cardiac ischemia b. Etiology 1. Prinzmetal's angina (Spastic contractions of the coronary arteries, ST-elevation, not precipitated by cardiac work, longer duration, usually more severe) 2. Fixed hard atheromas I. Atheromas that cause more than a 70% reduction of the lumen can be sufficient for blood supply during rest but cause ischemia when the demand for oxygen is increased II. The endothelium of the atherosclerotic arteries is dysfunctional and can not secrete vasodilatory substancs such as NO II. Calcification, fibrosis, and loss of smooth muscle cells further impair the vessels capacity for dilatation d. Pain - Characteristics I. Precordial pressure - 'Heaviness' II. Vague, gnawing, burning sensation III. Can be crushing in severe cases IV. Progressive, last less than 15 minutes V. Relieved by nitroglycerin d. Pain - Location I. Retrosternal II. Radiate to left shoulder and arm (Less often to jaw and right arm) e. Triggered by - Ie 1. Climbing stairs 2. Exercise 3. Strong excitement 4. Eating a meal (Damjanov) |
|
|
Angina pectoris
a. Stable angina - Characteristics, associated pathological findings b. Unstable angina - --||-- c. Prinzmetal's angina - --||-- |

a. Stable angina
I. Pain that recurs predictably under identical conditions II. Hard atheromas that have narrowed the lumen of the coronary artery more than 70% b. Unstable angina\Preinfarctional angina I. The quality and intensity of the pain tend to vary and progress, ie to rest angina II. Can become unresponsive to nitroglycerin and progress to MI III. Pathological findings - Soft atheroma that narrow the lumen but are also prone to rupture, causing short-lived intraluminal thrombosis (Transient ischemic changes may be detected as ST-segment inversion) c. Prinzmetal's\Variant angina I. Typically pain at rest that may recur in a circadian manner II. Caused by spasm, often of coronary arteries that contain hard atheromas (Associated with ST-segment elevation) (Damjanov) |
|
|
Angina pectoris - diagnostic procedures
|
Angina pectoris - Diagnostic procedures
1. ECG I. Resting ECG is normal in 50% of cases II. Many patients show signs of myocardial ischemia such as down-sloping of the ST-segment and T wave inversion III. Stress ECG has a sensitivity of > 70% and specificity of 90% 2. Stress scintigraphy with thalium-201 I. Even higher sensitivity and specificity 3. Coronary angiography (Damjanov) |
|
|
Comparison of subendocardial (S) and transmural (T) myocardial infarctions
a. Cause b. Location c. ECG d. Pericarditis e. Rupture of ventricle f. Aneurysm of ventricle |
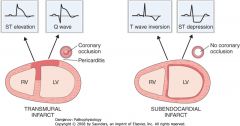
a. Cause
S: Hypotension T: Coronary thrombosis (Usually by rupture of soft atheroma, less often by thromboemboli originating from endocarditis vegetations on valves or mural thrombi in AF. Cocaine abuse can cause coronary spasm -> MI) b. Location S: Multiple foci, may be circumferential T: Single anatomic area corresponding to a specific coronary c. ECG S: 2 findings 1. T wave inversion 2. ST depression (-> Not Q wave deepening -> Non q wave infarction) T: 4 findings 1. QRS changes (width, depth) 2. Progressively deepening Q wave 3. STEMI 4. T wave inversion (ECG changes in only 85% of patients, the rest are nonspecific or nonexistent. d. Pericardiits S: No T: Yes e. Rupture of ventricle -> Hematopericardium S: No T. Yes f. Aneurysm of ventricle S: No T: Yes (Damjanov) |
|
|
Myocardial infarctions
a. At what time a day does MI most often occur b. S&S |
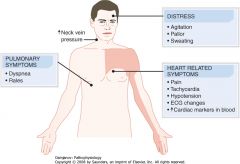
a. Morning hours
(Surge of catecholamines in the blood upon awakening?) b. S&S 1. Distress and agitation 2. Apprehensive 3. Pallor and sweating 4. Tachycardia (Compensatory reaction to acute heart failure) 5. Crushing chest pain lasting > 30 minutes and not relieved by nitroglycerin 6. Same radiation pattern as angina pectoris - Left shoulder and arm, neck, jaw 7. Hypotension (Pump failure) 8. Pulmonary rales and dyspnea (Left heart failure) 9. Elevation of JVP (Right heart failure or left heart failure -> right heart failure) (Damjanov) |
|
|
Complications of MI
|
Complications of MI
1. Arrhythmia and conduction abnormalities I. 50% II. Can cause sudden death in the early postinfarction period and is the main reason for admitting to cardiac ICU (Inferior (posterior) MI of occlusion of RCA often cause sinus bradycardia or an AV nodal block (85% of the cases the SA node and AV node is supplied by RCA), anterior MI of LAD often give bundle branch blocks) 2. Pump failure I. Proportional to the number of necrotic cardiac myocytes II. Early pump failure is a result of necrotic cardiac myocytes and cardiac stunning (Cardiac stunning - Ischemic cardiac myocytes lose ATP within minutes and this functional change make them inoperative even if they don't die immediately. These can be salvaged by reperfusion) III. Statistics Grade I - 30%, don't have heart failure, 5% mortality Grade II - 40%, mild failure, 15% mortality Grade III - 10%, pulmonary edema, 40% mortality rate Grade IV - 20%, cardiogenic shock, 50-80% mortality rate (If > 40% of the cardiac myocytes are damaged, systolic BP < 90 mmHg and urinary output < 20 mL\hour) 3. Mitral regurgitation I. From dilatation of mitral valve due to pooling of blood from heart failure II. From rupture of papillary muscles following infarction 4. Myocardial rupture I. Rupture of free wall -> hematopericardium and cardiac tamponade II. Rupture of interventricular septum -> L-R shunting -> Pulmonary hypertension -> Cor pulmonale III. rupture of papillary muscle -> Mitral valve insufficiency -> Acute pulmonary edema (Necrotic myocardium becomes infiltrated by neutrophils after 1-3 days. The neutrophils digest the necrotic myocytes and form a softening of the myocardium) 5. Ventricular aneurysm I. Noncontractile bulging scar (MI -> fibrous scarring) II. -> Weakens the pumping strength, pose obstacle to spread of electric impulses -> electrophysiologic disturbances, turbulent blood flow inside it -> thrombosis 6. Mural thrombosis I. AF II. On endocardial surface of the infarcted ventricular wall (Contain many thrombogenic substances) 7. Pericarditis I. Sterile pericarditis (Inflammation caused by the inflammatory cells (neutrphils -> macrophages -> fibroblasts), pericardial friction rub (fibrin exudation, roughening of surface) I. Immunologic pericarditis (Release of intracellular proteins -> antibodies against epicardial cells. Dressler's syndrome clinically - precordial pericarditic pain, pericardial friction rub, pericardial effusion. Responds to steroid treatment) 8. Chronic heart failure (Significant if > 25% of myocytes are injured) 9. Sudden death (Death that occurs without any preexisting or premonitory symptoms, or within 1 hour of onset of symptoms suggestive of CAD, complication of coronary atherosclerosis in > 85% of cases) (Damjanov) |
|
Clinical signs of chronic congestive heart failure
|
(Damjanov)
|
|
|
Paroxysmal atrial tachycardia
a. What b. Cause c. Treatment |
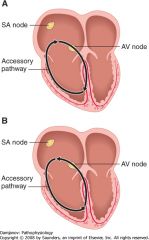
a. Sudden onset of tachycardia with a heart rate of 150-200 bpm
b. Most often secondary to reentry of electric currents around the AV node (Ie WPW syndrome, orthrodromic (image A) and antidromic (image B)) c. Treatment 1. Maneuvers that increase vagal tone I. Massage of carotid sinus II. Valsalva maneuver III. Immersion of head in cold water 2. Drugs I. Ca-channel blockers II. Digitalis (Damjanov) |
|
|
Infective endocarditis
a. Most affected areas b. Pathogens |
a. Most affected areas
1. Cardiac valves - Most common 2. Mural endocardium 3. Surface of cardiac defects in congenital heart disease 4. Artificial valvular prostheses b. Pathogens - Mostly bacterial 1. Streptococci - >60% of cases I. S. Viridans - Most common, upper aerodigstive tract II. S. Fecalis - Bowel III. S. Milleri - Urinary tract 2. Staphylococcal I. S. Areus - 20% (<- Skin, vascular access sites, IV drug abuse) II. Coagulase negative S. Albus (Most common cause of prosthetic valve infection) (Less often fungal) (Damjanov) |
|
|
Infective endocarditis
a. Is the valves of the left or the right heart most often affected, why b. Which valve is most often affected by IV drug abuse c. Characteristics of valves making them more susceptible d. Effects e. Causes of noninfectious endocarditis |
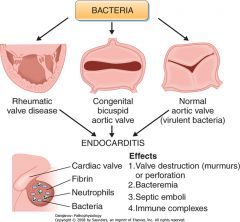
a. Left heart
I. High blood pressure -> more easily damage the valves? b. The tricuspid valve c. Characteristics of valves making them more susceptible 1. Previously damaged valves - Rheumatic valve disease 2. Congenitally abnormal valves - Bicuspid aortic valve (2%) (Highly virulent bacteria can infect normal intact valves) d. Effects 1. Valve destruction (-> murmurs) 2. Perforations 3. Septic emboli (Endocarditis -> fibrin-rich vegetatiosn containing bacteria and neutrophils) 4. Immune complexes e. Noninfectious endocarditis 1. Nonbacterial thrombotic endocarditis (NBTE) (In terminal stages of many chronic infectious and wasting disorders) 2. Libman-Sacks endocarditis of SLE 3. Acute rheumatic endocarditis (Can cause vegetations and murmurs) (Damjanov) |
|
|
Infectious endocarditis - S&S
a. General b. Heart c. Lung d. CNS e. Spleen f. Kidney g. Blood h. Hands and skin |
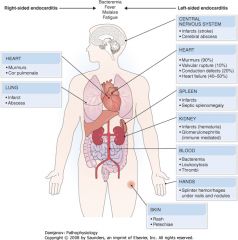
Infective endocarditis - S&S
a. General 1. Bacteremia 2. Fever 3. Malaise - Fatgiue, weakness 4. Night sweats 5. Anorexia and weight loss b. Heart 1. Murmurs (>80%) (Vegetations, rupture of chordae tendinae) 2. Conduction defects (20%) 3. Valvular rupture (10%) 4. Heart failure (>40%) c. Lung 1. Infarct 2. Abscess d. CNS 1. Infarcts (Stroke) 2. Abscesses (cerebral) e. Spleen 1. Infarcts 2. Septic splenomgaly f. Kidney 1. Infarcts (->hematuria) 2. Glomerulonephritis (Immune-mediated) g. Blood 1. Bacteremia 2. Leukoctosis 3. Thrombi 4. Vasculitis (Immune-mediated) h. Hands and skin 1. Splinter hemorrhage under nails and 2. Swelling and small nodularity of the fingers (Osler's nodes) 3. Clubbing of fingers 4. Rash 5. Petechiae - Skin and mucosal (1,2,5 by peripheral embolisms) (Damjanov) |
|
|
Mitral stenosis
a. Auscultatory findings b. Other findings c. Diagnostic methods |
a. Auscultatory findings
1. Loud S1 2. Mid-diastolic murmur 3. Opening snap b. Other findings 1. AF (Dilatation and hypertrophy of left atrium) 2. Fatigue (Diminished CO) 3. Dyspnea (Pulmonary venous congestion -> pulmonary edema, worse when lying down) 4. Leg edema, hepatosplenomegaly, ascites (<- Cor pulmonale) 5. Peripheral signs of infarction - Brain, extremities, kidneys (Arterial thromboemboli from vegetations on abnormal valves) c. Diagnostic methods 1. Echocardiography - Thickening of valves, narrowing of the orifice, reduced diastolic filling 2. Radiography - Enlargement of left atrium and right ventricle, pulmonary congestion and edema 3. Pulmonary pressure 4. ECG (Damjanov) |
|
|
Mitral regurgitation
a. Causes a. Auscultatory findings c. Other findings |
a. Cause
1. Chronic I. Rheumatic carditis (40%) (mitral regurgitaiton and stenosis) II. Degeneration of congenitally floppy valve III. Myocardial changes that lead to dilatation of the mitral valve ring (MI, myocarditis, dilated cardiomyopathy) 2. Acute I. Rupture of papillary muscle in MI II. Rupture of chordae tendinae in infectious endocarditis b. Auscultatory findings - Pansystolic murmur c. Other findings 1. Left ventricular hypertrophy -> Heart failure 2. Pulmonary hypertension -> cor pulmonale 3. Leg edema, hepatosplenomegaly, ascites (Diagnose - echo, color Doppler, cardiac catheterization) (Damjanov) |
|
|
Aortic stenosis
a. Causes b. Auscultatory findings c. Other findings d. Diagnosis |
a. Cause
1. Congenital valvular abnormalities - Young persons 2. Calcifications of congenital bicuspid valves 3. Rheumatic carditis 4. Idiopathic calcification - Elderly (Narrowing and calcification) b. Auscultatory findings 1. Pansystolic murmur 2. Ejection click c. Other findings 1. Left ventricular hypertrophy 2. Forward and backward heart failure 3. Angina and exertional syncope (Inadequate filling of coronary arteries, which originate from the sinus of Valsalva behind the calcified cusps) d. Diagnosis 1. ECG - Left ventricular hypertrophy 2. Echocardiography - Calcifications of the cusps 3. Doppler cardiography - Gradient across the aortic orifice (Damjanov) |
|
|
Aortic regurgitation
a. Causes b. Auscultatory findings c. Other findings |
a. Causes
1. Congenital valvular defects 2. Valvular defects of rheumatic or infective endocarditis 3. Dilatation of the aortic ring by atherosclerosis or syphilitic aortic aneurysm 4. Marfan's syndrome b. Auscultatory findings 1. Decrescendo diastolic murmur (Reflux) 2. Ejection systolic murmur (Related to increased stroke volume, best heard when on expiration when patient is leaning forward) c. Other findings 1. Hyperdynamic heart action I. Thrusting apex II. Pulsations can be seen in nailbed (Pulsating nodding sign of head is known as de Musset's sign) III. Angina 2. Forward heart failure 3. Backward heart failure (Damjanov) |
|
|
Chronic endocarditis
a. Causes b. Effects |
a. Chronic endocarditis
1. Rheumatic fever 2. Healed bacterial endocarditis 3. Carcinoid syndrome b. Effects - Stenosis and incompetence\insufficiency, most often of left side 1. Mitral stenosis 2. Aortic stenosis 3. Mitral regurgitation 4. Aortic regurgitation (Damjanov) |
|
|
Cardiomyopathy
a. Cardiomyopathy b. 3 groups and their characteristics c. Clinical diagnosis of the group as an entity |
a. Cardiomyopathy
I. Diverse group of heart diseases caused by pathological changes in the myocardium II. Can only be treated by cardiac transplantation b. Classification 1. Dilated cardiomyopathies I. Dilation of both ventricles and systolic dysfunction 2. Hypertrophic cardiomyopathies I. Ventricular hypertrophy, diastolic dysfunction 3. Restrictive cardiomyopathies I. Stiff myocardium that cannot dilate properly c. Clinical diagnosis I. Based on exclusion II. After coronary, valvular, hypertensive, or congenital heart diseases have been ruled out (Damjanov) |
|
|
Dilated cardiomyopathy
a. Causes b. Characteristics |

a. Causes
1. Idiopathic\Primary Secondary 2. Genetic causes 3. Infection I. Viral - Coxsackievirus A and B II. Parasitic - Trypanosoma cruzi (Endemic in South America) 4. Drugs and toxins I. Alcohol II. Anthracyclines (Anticancer agents - Doxorubicin, daunorubicin, daunomycin) III. Cobalt 5. Endocrine\Metabolic I. Thyroid disorders - hyper or hypo II. Peripartum or postpartum cardiomyopathy III. Hemochromatosis 6. Nutritional I. Starvation II. Beri-beri\Thiamine deficiency 7. Immune I. Sarcoidosis (Idiopathic, granulomatous, composed of epithelioid and multinucleated giant cells) II. Scleroderma III. Polymyositis b. Characteristics 1. Extensive dilatation of the ventricles causing systolic dysfunction (The left ventricular ejection fraction is usually < 45%. Its normally 50-65%) 2. Congestive heart failure - Backward and forward signs 3. Mural thrombi formation 4. Myocyte stretching -> Arrhythmias, seen on ECG as QRS widening and distortion (Damjanov) |
|
|
Hypertrophic cardiomyopathy
a. Causes b. Characteristics c. Diagnostic findings d. S&S e. Factors causing sudden death |
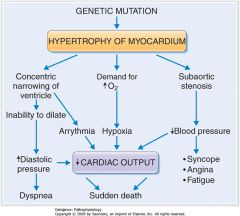
a. Causes
1. Genetical - Mutations of genes encoding cardiac proteins (beta-myosin heavy chain, troponin, alpha-tropomyosin) b. Characteristics 1. Increased total cardiac mass without a corresponding increase in the size of the cavities c. Diagnostic findings 1. The left ventricular ejection fraction are either high normal or increased (>65%) 2. End-diastolic ventricular pressure is increased 3. Maneuvers that reduce cardiac filling may cause fainting (Valsalva, nitroglycerin, standing upright) 4. Thickening of ventricle on echocardiogarphy 5. Increased RQS voltage on ECG d. S&S 1. Dyspnea (↑Diastolic pressure) 2. Syncope 3. Angina 4. Fatigue (2-4 is among other things caused by prominent asymmetrical hypertrophy of ventricular septum causing subaortic stenosis) 5. Sudden death (History of sudden deaths in family is common) e. Factors causing sudden death 1. Hypertrophy of myocardium -> Subaortic stenosis -> ↓CO 2. Hypertrophy of myocardium -> ↑Oxygen demand -> Hypoxia -> ↓CO 3. Hypertrophy of myocardium -> Distort conduction system -> Arrhythmia -> ↓CO 4. Hypertrophy of myocardium -> ↓Diastolic compliance -> ↑Diastolic pressure -> ↓CO (Beta-blockers and calcium channel blockers are used to slow down the heart rate and prolong diastole, and thus allow better diastolic filling of the ventricles) (Damjanov) |
|
|
Hypertensive heart disease
a. General effects b. Effect on Aorta c. Effect on cerebral vessels and eye vessels d. Effect on renal vessels e. Effect on heart |

a. General effects
I. Accelerate atherosclerosis II. Cause mechanical injury to arteries III. Cause ventricular hypertrophy b. Effect on aorta I. Dissection II. Aneurysm c. Effect on cerebral vessels and eye vessels I. TIA (Microaneurysms and microhemorrhages) II. Stroke III. Microinfarct dementia IV. Retinopathy d. Effect on renal vessels I. Hypereninemia II. Nephrosclerosis -> renal failure e. Effect on the heart I. Atherosclerosis of coronary arteries -> MI II. Left ventricular hypertrophy -> Right ventricular hypertrophy -> Congestive heart failure |

