![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
111 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Body water |
60-80% Fluids move from high pressure to low pressure Consistent of intracellular fluid (icf)- fluid inside cells Extracellular fluid (ecf) fluid outside of cells |
|
|
|
Extracellular fluid |
Made up of: Interstitial fluid: in between cells Intravascular fluid- fluid in blood |
|
|
|
Normal flow of body water |
Water leaks out of blood capillaries into the tissue spaces (interstitial fluid) and is collected or reclaimed by the lymphatic capillaries and filtered and returned to circulation. Water can also move into and out of out cells depending on the concentration of ions. Water, sodium, and glucose move across the capillary membrane due to plasma proteins (albumin) |
|
|
|
Plasma proteins (albumin) |
In blood plasma. They stay in capillaries to help mantain blood volume because albumin attracts h2o. |
|
|
|
Concentrations similarities and differences |
The concentration of ions between the blood (intravascular) and interstitial fluids is very similar There is a big difference between ion concentration in the ICF and the ECF. |
|
|
|
Compare the levels of Na+ & K+ Ions |
Bonding between these 2 is plasma membrane of cell ICF- lower levels of Na+ higher than level of K+ ECF- Higher levels of NA+ and lower levels of K+ |
|
|
|
Passage of H20 across plasma membrane |
Water passes freely but passage of ions (electrolytes) is regulated by Na+ and K+ Atapase pumps A lump that pumps both Na+ and K+ but require ATP (energy) Polarized, drpolirized, repolarized=> movement of ions across the plasma membrane These pumps are what restore the resting membrane potential of our cross after repolarization |
|
|
|
Fluid movement between blood and interstitial fluid |
Movement of fluid between blood plasma (intravascular) and interstitial fluid is controlled by several pressures: Capillary Hydrostatic Pressure (CHP) Capillary Oncotic Pressure (COP) Interstitial Hydrostatic Pressure (IHP) Interstitial Oncotic Pressure (IOP) |
|
|
|
Capillary Hydrostatic Pressure (CHP) |
Pushing pressure or blood pressure. Pushes water out of the capillaries and into the interstitial compartment. |
|
|
|
Capillary Oncotic Pressure (COP) |
Pulling pressure pulling fluid into the capillary from interstitial fluid to capillary via plasma cell (albumin) it's concentration determines COP |
|
|
|
Interstitial Hydrostatic Pressure (IHP) |
Pushing pressure is what cause water to move from the interstitial space into the capillary. |
|
|
|
Interstitial Oncotic Pressure (IOP) |
Pulling force or pulling fluids out of capillaries and into the interstitial space |
|
|
|
Filtration |
When fluid moved out of the capillaries into interstitial fluid |
|
|
|
Reabsorption |
Fluids moved from interstitial space back into the capillaries "reclaim" |
|
|
|
Net pressure, fluid movement, & capillaries |
All four pressures working together determine which direction the fluid flows and the magnitude of the force (net pressure) that drives the fluid in that direction. |
|
|
|
Net pressure equation |
We want to know 2 things: 1. What direction is fluid flowing (into or out of) the capillary. 2. What is the net pressure such the magnitude of the force that is driving the fluid in that direction. First: add up the forces driving the water out of the capillary (all hydrostatic) Second: add up the forces pulling water in (all Oncotic unless negative than add that number positively into hydrostatic because force is reversed). Finally, subtract the pressures Forces pushing - forces pulling= fluid flow The sign wether positive or negative tells is the direction of the water (+ fluid flow out of capillary) (-fluid flow into the capillary) |
|
|
|
Practice problem pressure examples |

|
|
|
|
Control mechanisms for water balance in the body |
Thirst Hormones (ADH, Aldosterone, ANP) Normal mechanism in body that regulated blood volume/blood pressure (Renin angiotensin mechanism) |
|
|
|
Ten in Angiotensin Mechanism |
Mechanism is activated when blood volume or blood pressure is low Juxtaglomerular cells (in kidney;near glomeruli) detect a decrease in blood volume and blood pressure. Causes kidneys to release Rabin (an enzyme) that converts angiotensin to angiotensin 1. Angiotensin converting ezyme (ace) converts angiotensin 1 to angiotensin 2. This causes 3 things: 1. Vasoconstriction: increase in BP 2. Antidiuretic hormone release: reabsorprion of h20 increase blood volume and increase BP 3. Aldosterone release: reabsorprion of sodium first and than h20 follows which increase blood volume and BP. |
|
|
|
ACE inhibitor drugs |
Hypertension (increase in blood pressure). Angiotensin converting enzyme blocked keeping conversion I angiotensin 2 to not happen wich decrease blood volume and BP. |
|
|
|
Solutions |
Are described in terms of their solute cncentration Water want to dilute moving towards solute |
|
|
|
Tonicity |
The ability of a solution with a certain concentration of dilutes to affect the shape (tone) of a cell by causing water to move into or out of the cell. |
|
|
|
3 basic types of solutions |
Isotonic Hypertonic Hypotonic |
|
|
|
Isotonic |
Normal saline solution Same concentration of dilutes to ICF. No water movement. Equal or the same to intracellular cell fluid. Shape tone the same. |
|
|
|
Hypertonic |
Most dangerous part of ECF This solution has increased dilutes than the cells ICF. Water lives out of the cell into the solution. The cell shrinks and of too much water goes out of the cell the cell crenates and dies |
|
|
|
Hypotonic |
Help hydrate someone experiencing fluid deficit. Solution solutes below ICF. Water moves into the cell. Cell swells and bursts of too much. |
|
|
|
PH |
Power of hydrogen or Potential hydrogen Log based scale. Exponential increase from 7 to acid left or basic to right. Scale measures hydrogen ion [H+] concentration pH= log 1/[H+] explains relationship of [H+] and pH One pH unit is 10× |

|
|
|
Acid & bases |
Acids- have lots or increase of [H+] decreased ph Bases- have lots of OH- or hydroxide ions. (few hydrogen ions) increased ph Acids and bases have inverse relationship |
|
|
|
Normal range of blood ph |
7.35-7.45 Extreme range of ph 6.7-7.9 |
|
|
|
Acidosis |
Condition where there is excess [H+] in extracellular fluid |
|
|
|
Alkalosis |
Condition where there is a deficit [H+] in extracellular fluid. |
|
|
|
How we maintain acid base balance |
2 organs: 1. The kidneys: they can excrete or retain H+ if needed. 2. The respiratory system: in order to understand how respiratory system regulate acid base balance we have to look at the chemical reaction of CO2 and H20. CO2+H20<=> H2CO3<=> H+ + HCO3- |
|
|
|
Reactant concentrations equation explanation |
Carbon dioxide combines with water to provide carbonic acid (wich is very unstable quickly dissociated) intia H+ and a bicarbonate ion. Reaction is reversible depends on the reactant concentrations More reactant on left side will push the reaction to the right. More CO2 drives the reaction right wich increases H+. CO2 + H+ are directly related Increased CO2 (reactant) = increased H+ Decreased CO2= Decreased H+ |
|
|
|
Example disorder |
A person has a respiratory disorder (emphysema) where they can't exhale nomal amounts of CO2. What happens to CO2 in the blood? Increased levels of CO2 in blood Which way does reaction go? Goes right [H+] ? Increases Too many H+ ions= acidosis What compensates and how? Kidneys excrete urine with more H+. The body has ability to compensate for this (to a certain degree) |
|
|
|
Compensations for acidosis |
1. Kidneys: retaining I exceeding H+ 2. Respiratory system But of respiratory is the problem (diseased) in causing acidosis or alkaloids it can't compensate. Compensation comes from kidneys and not respiratory system. |
|
|
|
Metabolic acidosis or alkalosis |
Any acid base imbalance caused by anything other than respiratory system |
|
|
|
Acid base imbalance may be causes by |
Metabolic problem Person producing too much or not enough H+ A kidney problem-the person can't excrete excess H+ In both cases acidosis or alkalosis the body will try to compensate for the imbalance (try to bring ph back to normal) |
|
|
|
Compensation carries out by: |
Respiratory system Kidneys. If respiratory system can't than kidneys will compensate |
|
|
|
Buffer |
A way to keep H+ in balance by either releasing a H+ if something is too basic or binding to a hydrogen if something is too acidic. If excess H+ picked up by bicarbonate If not enough released by carbonic acid H+ is being shuffled back and forth by carbonic acid and bicarbonate to keep ph balance. |
|
|
|
Normal ph |
7.35-7.45 |
|
|
|
Reaction left or right? |
CO2+H20<=> H2CO3<=> H+ + HCO3 In bold buffer system of carbonate of the ECF Carbonic acid very unstable |
|
|
|
CO2 and Hydrogen reactions |
Increased CO2 levels= reaction to right=> increased H+ Decreased CO2 levels= reaction proceeds to the left-=> Decreased H+ |
|
|
|
Henderson Hasselbach equation |
Described pH in terms of the buffering system. The most important part of this rqustio. Is the ratio between bicarbonate and carbonic acid. The normal ratio of bicarbonate to carbonic acid is 20/1 |
|
|
|
Henderson Hasselbach eq. Cont. |
pH= K (6.1) + log (exponential) [HCO3-] ------------ [H2CO3] K is a constant related to how easily carbonic acid dissassociates into H+ and bicarbonate K is always 6.1. 6.1 + log 20/1 *log of 20 => 6.1 + 1.3 = 7.4 normal pH Bc carbonic acid is so unstable the only way to measure it is to use a new but similar equation pH= k+log [HCO3] --------- [CO2] All imbalances involve a shift in this ratio all compensations involve a sift in this ratio. |
|
|
|
Example condition |
A person is hyperventilating causing them to exhale too much CO2 What happens to CO2 levels in blood? Decrease Wich way does the reaction go? Left What happens to [H+]? Decreased or defficient Acidosis or alkalosis? Alkalosis Respiratory or metabolic? Respiratory Compensation by? Kidneys they retain H+ |
|
|
|
Example condition |
Untreated diabetic not getting enough glucose into cells so body breaks down days and proteins for energy instead Ketoacidosis What happens to H+ concentration? Increased H+ Respiratory or metabolic? Metabolic Compensation by? Respiratory system exhale to get rid of more CO2 to being decreased H+ |
|
|
|
Respiratory acidosis |
Acidosis is most common condition
Increase in CO2 blood levels therefore an increase in H+.
Acute problems: Pneumonia Airway obstructions (asthma or aspiration) Chest injury Opiate drugs (depressed respiratory control center) Chronic conditions: 1. COPD: emphysema; can't exhale appropriate amount of CO2 2. Decompensated respiratory acidosis: body unable to compensate. The buffer system is ineffective. Impairment is severe or an infection develop. The body is unable to compensate.
|
|
|
|
Causes of metabolic acidosis |
Associated with an decrease in bicarbonate 1. Excessive loss of bicarbonate from diarrhea. 2. Increased use of bicarbonates. The body is using too much bicarbonate. 3. Renal disease or renal failure. |
|
|
|
Generalized effect of acidosis |
Direct effects are on the nervous system. Nervous system overall is depressed. Headache Lethargy Weakness Confusion Eventually coma or death |
|
|
|
Compensation for acidosis |
Compensation by the respiratory system is deep, rapid breathing Compensation by kidneys is excretion of hydrogen in urine. |
|
|
|
Causes of alkalosis |
Respiratory alkalosis: too much CO2 is exhaled. Drop of CO2 levels: hyperventilation Metabolic alkalosis: Increase in bicarbonate HCO3. Loss of HCL from the stomach in the early stages of vomittin or with stomach drainage. Hypokalemia: decrease in potassium levels Excessive ingestion of antacids. |
|
|
|
Effects on alkalosis on body |
Stimulate the nervous system Increased irritability of the nervous system Restlessness Muscle twuitching Tingling and numbness of fingers Eventually tetany, seizures, coma and death |
|
|
|
Compensation for alkalosis |
Compensation by the respiratory system is shallow slow breathing compensation by the kidneys is retention of more H+ in the body. |
|
|
|
How do we compensate for fluid deficit |
Increased: thirst Heart rate Construction of cutaneous vessels of skin will be pale and cool Produce less urine and is more concentrated |
|
|
|
Sweating |
When sweating is the cause of the fluid deficit we not only lose water but also electrolytes. Electrolytes are important for regulating water balance between ICF and ecf both must be replaced. |
|
|
|
Causes of dehydration |
Vomitting and diarrhea Drainage or suction of any part of the digestive tract Excessive sweating Diabetic ketoacidosis--with loss of fluids, electrolytes and glucose in the urine. Insufficient water intake: more so in the elderly and unconscious persons *use of concentrations formula for infants to provide.more nutrition. |
|
|
|
Effects of dehydration (S & S) |
Dry mucous membranes Decreased skin turgor Lower blood pressure Hypovolemia (weak pulse and fatigue) Increased hematocrit (measure of rbc proportional to blood plasma membrane Mental function-confusion Loss of consciousness- brain cells are losing water and function (shrinking)
|
|
|
|
Fluid deficit |
Dehydration caused by reduced intake of fluids, excessive loss of fluids or a combination of both. Fluid loss is often measures by a change in body weight. Mild deficit- decrease in 2% in bw Moderate- decrease in 5% in be Severe- decrease in 8% bw |
|
|
|
Infants and FD |
More serious problem ininfants and elderly because they lack Fluid reserve. Infants lose more water through their proportionally larger body surface area and need more water because their metabolic rate is higher. Intravascular fluid space is also rapidly depleted in infants ( hypovolemia) |
|
|
|
Hypovolemia |
Can affect the heart brain and kidneys. FD in infants is usually indicated by decreased urine output increased lethargy and dry mucosal membranes. |
|
|
|
Effects manisfestations of edema (symptoms) |
Localized or systemic edema Pitting edema: severe, put or indentations left after pushing on area of edema (fluids move away from pressure but do not return when pressure is removed). Localized: Restriction in ROM, edema in the intestinal wall- may interfere with absorption of nutrients Around heart or lungs-restricts movements and functions of these organs Pain if edema puts pressure on nerves or edema is in an area where there is a closed cavity (cerebral edema) causing head aches. Sustained edema- hinders venous return and arterial circulation wich can impair O2 delivery to the tissues causing necrosis and ulcerations.
|
|
|
|
Edema in mouth |
Soreness can form on the gums that are slow to heal Dentures may not fit properly Adematous tissues in the skin is very suceptible to breakdown from pressure abrasion and external chemicals. |
|
|
|
What causes lots of plasma proteins |
Kidney disease (glomulas) synthesis Synthesis of plasma proteins is impaired (liver disease) or malnutrition. Burn patients who have extensive 3rd degree burns (proteins leak out) Obstruction of lymphatic vessels or removal of lymphatic vessels Normally the function of lymphatic capillaries is to collect leaked fluids from interstitial space and returns them to blood stream If a lymphatic vessel is blocked (a tumor) or has been removed fluid in the interstitial space in the area.will not be collected but instead remains in the interstitial compartment (edema) (lymph edema) Increased capillary permeability- fluids leak out of capilary into interstitial space (edema) caused by the inflammatory response Can be localized or systemic (anaphylaxis) |
|
|
|
Causes of edema |
Increase capillary hydrostatic pressure (increase chp) (blood pressure) This will prevent return of fluid from the interstitial space back into the blood (at the senile end of the capillary bed) Or It will force excess out of the blood land into interstitial space. |
|
|
|
What increases CHP |
Hypervolemia- increased blood volume Caused by kidney failure Pregnancy Congestive heart failure Adminiestration of excess fluid Loss of plasma proteins (albumin) Decrease capillary Oncotic Pressure due to loss of plasma proteins. Plasma proteins normally stays in blood stream so the presence of fewer proteins mean more fluid will leave the blood and move back into interstitial compartment. |
|
|
|
Edema-dehydration |
To maintain constant level, we must take in as much fluid as we lose. Fluid intake by ingesting foods and liquids. |
|
|
|
Control mechanism for fluid in the body |
Thirst mechanism in the hypothalamus Adh (anti diuretic hormone) -controls the amount of water leaving the body in urine. Aldosterone- determines the reabsorprion of sodium resulting in reabsorprion because water follows sodium. Anp- atrial natriuretic peptide hormone secreted by myocardial cells in the atria of the heart regulates fluid sodium and potassium levels. |
|
|
|
Fluid excess(edema) |
Have fluids collecting within the interstitial space of the extra cellular fluid outside of blood cells. Causes swelling and enlargement of tissue (more systemic) Can be visible (facial edema) or invisible (liver damage) Usually more severe in dependent area of the body areas where force of gravity is greatest (buttox feet and ankles) most dependent areas. If net pressure is negative-- direction of fluid flow is into the capillary Chp+ihp+iop-cop= 10+7+5-26= 22-26=-4mmhg flow into capillary bc capillary negative |
|
|
|
What does ph stand for |
Power of hydrogen |
|
|
|
Because the equationfor good based on a log scale a ph of 7 would be ------ times greater than a ph of 5 |
100 |
|
|
|
The end result of ram |

|
|
|
|
What conditio. Would ace inhibitor be used for? |
High blood pressure or hypertension |
|
|
|
If I put a cell in hypersonic solutio. What will happen to it and why? |
The environment outside of cell is higher than solutes than inside of cell. The fluid would mover out of the cell causing crenation. |
|
|
|
Equation buffer system |

|
|
|
|
Rest of quiz |

|
|
|
|
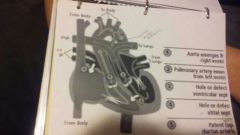
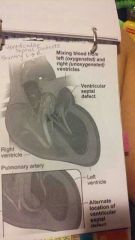
The pathway of blood through the adult heart |
Deoxygenated blood from body Superior and inferior vena cava Right atrium Tricuspid RT AV Valve Rt ventricle Semi lunar valve Pulmonary artery (oxygenated) Pulmonary veins Left atrium Bicuspid or mitral valve Left ventricle Aorta In adult heart pressure is highest in left side. |
|
|
|
Why is the fetal heart different? |
The fetal lungs are collapsed and non functioning. All exchange of O2, CO2, nutrients, wastes, hormones occur between mom and fetus at the placenta a huge bed of capillaries. Blood always wants to go through the path of least resistance. Blood doesn't need to go to the lungs (pulmonary circuit) so the fetal heart has several structures that allow pulmonary circuit to the lungs to be bypassed. |
|
|
|
Fetal heart pathway |

The firemen ovale (ovale is opening into interatrial septum) Ductus arteriosus-a duct that connects the pulmonary artery to the aorta. The pressure in the fetal heart is highest on the right side because of collapsed lungs and high resistance. Gets pushed to left side through firemen ovale. |
|
|
|
Babies birth |
Baby take a first breath- cries and lungs inflate. Umbilical cord gets clamped and cut (vascular connection between baby and placenta) Now the baby's heart must function like an adult heart (now pressure is on the left sode of the heart and exchange of O2 and CO2 is occurring in the lungs. This increase in pressure on the left sode will cause the flaps of firemen ovale to close and stick to the interstitial septum. This provides temporary closure of the firemen ovale. Permanent closure of the firemen ovale occurs at 6-8months and becomes fossa ovalis. Also the ductus arteriosus (smooth muscle in walls constricts and close the ducts. It occurs within a couple of days and closed duct becomes ligament structure called ligamentum arteriosum. |
|
|
|
Congenital heart defects |
.8% of love births have a congenital heart defect. Usually the defect causes one of two things to happen: 1. A shutting of blood flow through an abnormal connection between chambers or between pulmonary or systemic circuits. 2. Obstructive defect like stenosis wich causes increased pressure in chamber behind the obstruction. |
|
|
|
Causes of congenital heart defects |
Unknown but there are some contributing factors: 1. Environmental (vital infection during first 8 weeks of pregnancy, drug and alcohol use, or maternal lupus) 2. Hereditary factors- genetic or inherited. 3. Persistence of structures from fetal heart/circulation. |
|
|
|
Patent ductus arteriosus (PDA) |
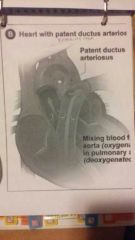
This is when the ductus arteriosus does not close properly after birth. It persists as a shunt (open) Blood follows the path of least resistance. The blood flow will travel back through the patent ductus arteriosus instead of going in through the body goes through aorta instead of pulmonary artery for oxygenation. This abnormal blood flow from aorta through patent ductus arteriosus into pulmonary artery will produce a heart murmur an abnormal heart sound. This is how PDA is usually detected. |
|
|
|
Possible results of PDA |
Increased blood volume and increased BP in pulmonary circulation Decreased cardiac output on the left side and manifestation of heart failure.
Degree of symptoms seen dependent on severity of shunt. |
|
|
|
Atrial septal defect (ASD) |
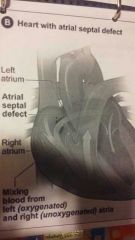
When the foramen ovale doesn't close. It persist as a left to right shunt (opening). Symptoms depend on the severity of the shunt. Many are asymptomatic. Symptoms include: Right ventricular hypertrophy Dyspnea or SOB Easily fatigued Can cause decreased growth.
Surgery may be delayed until school aged of shunt isn't severe foramen may close on it's own. |
|
|
|
Ventricular septal defect (VSD) |
The most common of all the congenital heart defects. An opening in the interventricular septum (between the right and left ventricles). The shunt will be from left to right. Because higher pressure on the left side.
If opening is very small it may be closed during systole (ventricular contraction) bc of contraction of septum. 1/3 of VSD close spontaneously on their own. If opening is large we will we overloading on right ventricle bcause of left to right shunt and Of pulmonary circulation the pressure of the right ventricle gradually increases. Eventually causing pressure of left and right ventricles to equal. |
|
|
|
Tetrology of fallot |
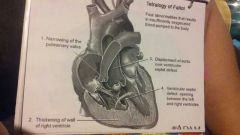
First described in 1888. 4 defects together at the same time: 1. Pulmonary artery stenosis. Narrowing at the base of the pulmonary artery 2. Ventricular septal defect 3. Dextraposed aorta (shifted opening in the wrong place) 4. Rt ventricular hypertrophy.
The pressure in rt ventricle is increased because vsd causing LT to RT due to shunt (opening) all pressure and blood on rt side. Larger opening means more blood enters. It's increased pressure that causes hypertrophy. The stenosis at base of pulmonary artery and left to RT shunt through vsd together this causes the pressure to be higher on rt side than the left. Blood is shunted from right to left through the vsd. Low O2 venous bloodis going through systemic circulation. There is also decreased blood flow to the lungs (because of stenosis) it chooses bigger opening or home this causes decreased oxygenation of the blood.
|
|
|
|
Blue baby |

Cyanosis from teratology of falloff. Children have tet spells because they aren't getting enough CO2 a squatting position but will put legs up increasing pressure in systemic circuit. This will help get blood to lungs and also decrease the right to left shunt thru the vsd. If 4 defects are severe they will not survive without surgery. |
|
|
|
Normal roles of great vessels |
Normally the aorta is exuti g the left ventricle and delivers O2 blood to body or systemic circuit. Normally the pulmonary artery is exiting the right ventricle and delivers Deoxygenated blood to lungs wich is the pulmonary circuit. |
|
|
|
Normally how the heart develops |
1. The heart starts out as a single tube that has a primitive (one) atrium and primitive (one) ventricle. During the development of heart there is one great vessel coming off this single tube. This vessel is called the "trunkus arteriosus" (4th week of gestation) 2. The single tube then doubles over on itself and forms two parallel pumping systems each with two chambers but still only one great vessel the trunkus arteriosus. 3. The reunjus arteriosus divides into two vessels: The aorta and pulmonary artery. The two vessels the rotate so that the aorta exits the left ventricle and pulmonary artery exits the right ventricle. |
|
|
|
Abnormal transposition of the great vessels. |
In transposition of the great vessels the rotation does not occur. They are exiting the wrong chambers. The aorta exits the right ventricle and pulmonary artery exits the left ventricle. Not a survivable defect. Must be corrected. Deoxygenated blood on right goes back to systemic circulation to body and oxygenated blood on left side goes back on left side to lungs back to heart and oxygen never gets back to the body. |
|
|
|
Abnormal transposition and conditions that alleviate defect |
ASD VSD PDA These openings will shunt blood back to body but it will still be mixed blood and condition is still non survivable. 2-3 times more common in boys than in girls Commonly seen in mothers with diabetes. |
|
|
|
Constriction or coarctation of the aorta |
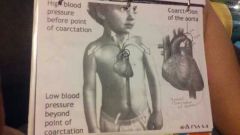
The effect on the body (symptoms) of this defect will depend on where the constrictii. Of the aorta occurs (in relation to ductus arteriosus) |
|
|
|
Preductal coarction |
The constriction of the aorta occurs above or before where the ductus arteriosus joins. Causes ductus arteriosus to remain openso we will see a shuntin of blood flow from pulmonary artery to aorta causing cyanosis of lower extremities. |
|
|
|
Postductal coarctation |
The constriction of the aorta occurs after or below whee the ductus arteriosus joins. The ductus arteriosus closes normally causes increase in blood pressure in the arms and decrease of blood pressure in the legs. |
|
|
|
Trunkus arteriosus |
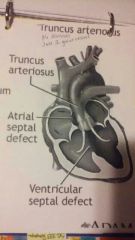
It never divides into coronary artery and aorta it just stays as one great vessel. Non survivable. No 2 separate systems. Mixed blood. |
|
|
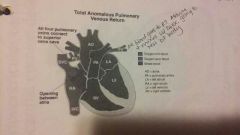
Anomalous pulmonary venous connection. |
In this defect the pulmonary veins empty into the right atrium instead of the left |
|
|
|
Endocardial cushion defect |
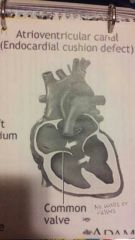
Normal function of endocarditis cushion is to form the septa and valves during development. In this defect the aorta and valves fail to form and we get a one chamber heart because no walls or valves to separate the heart. |
|
|
|
Normal valves |
Function to prevent backflow so that heart tranvels in one direction. Forward. |
|
|
|
4 valves in heart |
Tricuspid- btween right atrium and right ventricle Mitral or bicuspid- between left atrium and left ventricle Pulmonix valve (rt semilunar) base of pulmonary artery Aortic valve (left semilunar) base of the aorta Bicuspid and aortic valve are the most commonly defective because of high pressure on left side. |
|
|
|
2 basic valve defects |
Valve stenosis- narrowing of the valve. Interferes with valve opening. Valve can't open properly. Blood accumulates in chamber behind the valve. Chamber will hypertrophy as pressure increases Valve insufficiency- valve doesn't close properly. Blood regurgitated and flows backwards through the valve. Blood accumulates in chamber behind insufficient valve and pressure increases in valve causing hypertrophy of chamber. |
|
|
|
Causes of valve defects |
Valve dfects are more common on the left side because of higher pressure on the left. Causes: Congenital defects Trauma Ischemic damage Degenerative changes Inflammation (most common cause) due to a variety of different things but inflammation caused by rheumatic fever is the most common cause of all valve defects. |
|
|
|
Mitral valve stenosis |
When the mitral valve is stenotic (narrowed) and can't open properly. This will restrict the blood flow from the left atrium into the left ventricle. Blood backs up in the left atrium and ultimately backs up into pulmonary circulation. This will cause pulmonary edema. The left atrium becomes dilated and hypertrophic. Cardiac output is decreased on left side. Because cardiac output is so low the renin angiotensin mechanisms get stimulated wich makes the problem worse and will create further pulmonary edema. |
|
|
|
Steps to mitral valve stenosis |
Decreased cardiac output from mitral valve stenosis Causes decrease in glomerular filtration rate (GFR) in the kidneys. The kidneys detect low CO and blood volume and release renin. Remain initiates the renin angiotensin mechanism Outcomes are: Vasoconstriction- increase BP ADH- reabsorprion of water increase BP wich increase Blood volume Aldosterone release: cause reabsorprion of sodium and water wich increase Blood pressure and blood volume. In the case of mitral valve stenosis the I crease in blood pressure will cause pulmonary edema to be worse and manifestations of heart failure. |
|
|
|
Things we can do for valve defects: |
Percutaneous balloon valvuloplasty can be used to open a Stenotic valve or to replace a valve. Surgery |
|
|
|
Mitral valve insufficiency or regurgitation |
Mitral valve is not closing properly. The forward stroke volume of the left ventricle is going to decrease because blood regurgitated backwards into the left atrium. Pressure in the left atrium increases because of back flow. Increase pressure in pulmonary circuit causes pulmonary edema. Causes: ruptured chordae tendinae or papillary muscles. |
|
|
|
Mitral valve prolapse |
A type of insufficiency The leaflets of the mitral valve become enlarged and floppy. Causes: Specific to connective tissue disorder like marfan syndrom or osteogenesis imperfecta. Seen more freaquently in women than in men When leaflets become enlarged and floppy they balloon back into the left atrium. Most are asymptomatic. Any valve defect can cause or is detected by a heart murmur. |
|
|
|
If the person experiences symptoms of mitral valve prolapse: |
Chest pain (angina) Dyspnea (SOB) Fatigue Anxiety Palpitations Light headedness |
|
|
|
Aotic valve stenosis |
This is when the aortic valve is not opening up properly and blood backs up into left ventricle and left ventricle has to work harder to try and push out through the stenotic valve. Left side cardiac output will decrease causing left ventricular hypertrophy. Other symptoms: Angina Synscope (fainting) Heart failure |
|
|
|
Aortic valve insufficiency |
Aortic valve isn't closing properly and blood regurgitated back into the left ventricle so the left ventricle is constantly trying to increase it's stroke volume I the heart beats faster in order to try to compensate for increases stroke volume. Blood is backing up in the left atrium And pulmonary circuit causing pulmonary edema. |
|
|
|
Heart quiz part one |

|
|
|
|
Heart quiz part two |

|
|

