![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
100 Cards in this Set
- Front
- Back
|
What is duodenal atresia?
|
Congenital failure of small bowel to canalize.
|
|
|
Duodenal atresia is associated with what?
|
Down syndrome
|
|
|
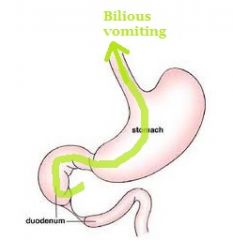
Clinical features of duodenal atresia?
|

(1) Polyhydramnios (can't digest amniotic fluid)
(2) Distension of stomach and blind loop duodenum of duodenum ('double-bubble' sign) (3) Bilious vomiting |
|
|
What is a Meckels diverticulum?
|

Outpouching of all three layers of bowel wall. Arises due to failure of vitelline duct to involute.
|
|
|
Meckel diverticulum is a __________ (true/false) diverticulum.
|
true
|
|
|
Early in embryologic life, the midgut receives it's nutrients from the _____________, and the way by which it receives this is through the ___________.
|
yolk sac; vitelline duct
"The vitelline duct is 'vital' for receiving nutrients early in life" |
|
|
The vitelline duct normally forms around the _______ week and involutes around the _______ week.
|
4th; 7th
|
|
|
What complication may arise in an vitelline duct that hasn't involuted at all.
|
Passing of meconium through umbilicus
|
|
|
On physical exam how would Meckels diverticulum present?
|
Something hard but soft (stool) in umbilical area.
|
|
|
Rule of 2's with Meckels diverticulum.
|
(1) Seen in 2% of population.
(2) 2 inches long (3) located in bowel within 2 feet of the ileocecal valve (4) presents during first 2 years of life |
|
|
What is the MC congenital anomaly of the GI tract?
|
Meckels diverticulum
|
|
|
Clinical presentation of Meckels diverticulum?
|
(1) Bleeding, volvulus, intussusception, or obstruction during first 2 years of life.
Most cases are however asymptomatic. |
|
|
Why can we see bleeding inside a Meckels diverticulum?
|
Heterotopic gastric mucosa may be present (choristoma)
|
|
|
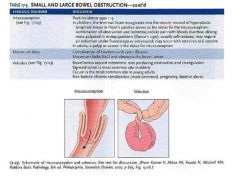
What is volvulus?
|
Twisting of bowel along its mesentery. Results in obstruction and disruption of blood supply (infarction).
|
|
|
Most common locations for a volvulus to occur?
|
(1) Sigmoid colon (elderly)
(2) Cecum (young adults) |
|
|
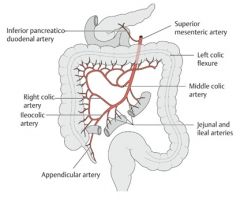
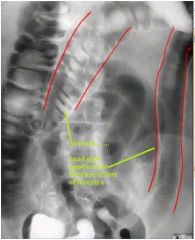
What could this be? What type of infarction is it?
|

Volvulus. Hemorrhagic.
|
|
|
What is intussusception?
|
Telescoping of a proximal segment of bowel into a more distal segment of bowel.
|
|
|
Patients with intussusception often present with?
|
When the segment telescopes, blood supply is compressed. Presents with obstruction or with infarction. Infarction often presents itself with something called current gelly stools.
|
|
|
Intussusception is associated with _____________.
|
a leading edge; it needs something to "hook on" to create a leading edge
|
|
|
What may create a leading edge for intussusception to occur?
|
(1) In children, the MCC is lymphoid hyperplasia (TI to cecum)
- Infection causes hyperplasia and terminal ileum gets dragged. (2) In adults, MCC is tumor. |
|
|
The small bowel is __________ (not/mildly/highly/ susceptible to ischemic injury.
|
highly. It needs tons of ATP (it performs a lot of digestion and absorption). Mucosal infarction can occur with marked hypotension.
|
|
|
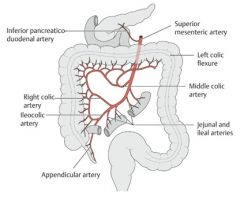
What could occur when you get ischemia of the small bowel? Describe the etiologies for each scenario.
|
(1) Transmural infarction may occur. Occurs with thrombosis or embolism of SMA or thrombosis of mesenteric vein.
(2) Mucosal infarction. Occurs with marked hypotension. |
|
|
An elderly man appears apathetic. He appears to have lower than normal muscle strength. He is also known to have heart problems and he has a goiter. Lately, whenver he eats he experiences a stabbing pain in his abdomen. What could be the cause?
|
Graves' disease in the elderly (apathetic hyperthyroidism) tend to have atrial fibrillation and congestive heart failure. A-fib can cause clot formation which could embolize, lodge in SMA and cause bowel infarction.
|
|
|
A middle-aged man has had recent episodes of bloody diarrhea. He has a long history of skin ulcers and pain in his testicles. His history is significant for hepatitis B infection. What could have caused this diarrhea?
|
Vasculitis of SMA with thrombosis and infarction of bowel.
|
|
|
A man with a constantly ruddy face now has migraine attacks and blurred vision. He tells you this followed his recent episode of melena.
(1) Why did he have melena? (2) What is a very common initial complaint in this disorder? (3) What other patient could have melena with the same etiology as in this disorder? |
(1) Thrombosis of IMV, he has polycythemia vera.
(2) Pruritus after bathing. (3) Lupus (lupus anticoagulant) |
|
|
Clinical features of small bowel infarction?
|
(1) Abdominal pain
(2) Bloody diarrhea (3) Decreased bowel sounds |
|
|
Upon consumption of milk products a man has abdominal distension and diarrhea. What is it?
|
Lactose intolerance (decreased function of lactase in brush border of enterocytes)
|
|
|
True or false: Lactose intolerance is always congenital.
|
False, it may be congenital or acquired (As you age or after GI infection)
|
|
|
Lactose is broken down into what?
|
Galactose and glucose
|
|
|
What is celiac disease?
|
Immune-mediated damage of small bowel villi due to gluten exposure.
|
|
|
Celiac disease is associated with what human leukocyte antigens?
|
(1) HLA DQ2
(2) HLA DQ8 |
|
|
Gluten is present in _________ and __________.
|
wheat (hvete); grain (korn)
|
|
|
This is the most pathogenic component of gluten. What happens inside the enterocyte?
|
Gliadin.
Gliadin is deamidated by tissue transglutaminase. Deamidated gliadin is presented by APCs via MHC II. Helper T cells help mediate the damage. |
|
|
Classical presentation of celiac disease in children and adults?
|
(1) Children: abdominal distension, diarrhea, failure to thrive
(2) Adults: chronic diarrhea, bloating |
|
|
One associated finding with celiac disease. Describe.
|

Dermatitis herpetiformis. Due to IgA deposition at tips of dermal papillae, disrupts connection between dermis and epidermis between those points. This results in a blister or vesicle that looks like the vesicles in herpes. Resolves with gluten free diet.
|
|
|
Laboratory findings in celiac disease?
|
(1) IgA antibodies against endomysium, tTG or gliadin.
|
|
|
A subset of patients with celiac disease can be IgA deficient. What laboratory tests can we employ to test for celiac disease in these patients?
|
IgG antibodies.
|
|
|
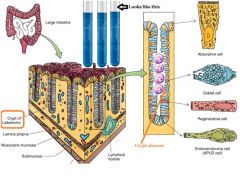
How do we make a diagnosis of celiac disease? What will it show?
|
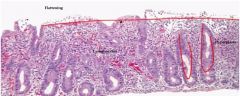
Duodenal biopsy.
Flattening of villi, hyperplasia of crypts, increased intraepithelial lymphocytes (normally we have villi that protrudes and tiny villi that dips down) |
|
|
What is the damage distribution in celiac disease?
|
Most prominent in the duodenum. Jejunum and ileum are less involved.
|
|
|
Most important diagnostic antibody in celiac disease?
|
Anti-tissue transglutaminase IgA
|
|
|
A woman with gluten-free diet for many years presents with celiac disease again. It is refractory to any dietary changes. What could have happened?
|
Small bowel carcinoma or T-cell lymphoma (Enteropathy associated T-cell lymphoma; EATL)
|
|
|
Tropical sprue is similar to celiac disease, however it is due to?
|
an unknown organism
|
|
|
Tropical sprue results in __________.
|
malabsorption and diarrhea
|
|
|
Tropical sprue is similar to celiac sprue, except [...]
|
(1) Tropical sprue occurs in tropical regions (e.g., caribbean)
(2) Arises after infectious diarrhea and responds to antibiotics (3) Damage is most prominent in jejunum and ileum; duodenum is less commonly involved |
|
|
What nutritional deficiencies could you theoretically get in tropical sprue?
|
Jejunum is affected --> Folic acid deficiency
Ileum is affected --> B12 deficiency |
|
|
What is Whipple's disease?
|
Systemic tissue damage characterized by macrophages loaded with Tropheryma whippelii organisms.
|
|
|
What stain would you use (1) and WHAT are you staining when looking for the etiology of Whipple's disease (2)?
|
(1) PAS
(2) Partially destroyed organisms are present in macrophage lysosomes (positive for PAS) |
|
|
What is the classic site of involvement in Whipple's disease? What is the result? Explain the pathology behind fat malabsorption.
|
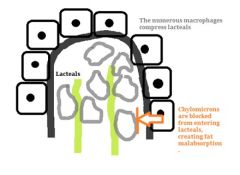
Small bowel lamina propria. Results in fat malabsorption and steatorrhea.
The macrophages are numerous and compress lacteals, preventing chylomicrons from properly diffusing from enterocytes into lacteals in lamina propria. |
|
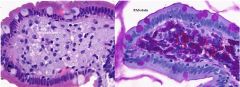
What is this?
|
Whipple's disease. PAS to the right.
|
|
|
The most common site affected in Whipple's disease is the lamina propria of the small bowel, however, what are some other common sites of involvement?
|
(1) Synovium of joints (arthritis)
(2) Cardiac valves (3) Lymph nodes (4) CNS |
|
|
What is abetalipoproteinemia? Describe it.
|
AR deficiency of apolipoprotein B-48 and B-100.
B-48 - Can't form chylomicrons (fat malabsorption) B-100 - Absent plasma VLDL and LDL |
|
|
What is a carcinoid tumor?
|
Malignant proliferation of neuroendocrine cells; low-grade malignancy (high grade would be small cell carcinoma).
|
|
|
Carcinoid tumor is positive for ____________.
|
chromogranin
|
|
|
Where does a carcinoid tumor arise?
|
Can arise anywhere along the gut (tarm). Small bowel is the MC site.
Remember it like this: Every site in the GI has a cancer associated with it, but not small bowel, so we gotta give it something. We give it this one. |
|

What is this?
|
Carcinoid tumor. Grows as submucosal polyp.
|
|
|
Carcinoid often secrete what substance and what is it metabolized to?
|
Serotonin; metabolized to 5-hydroxyindoleacetic acid (5-HIAA) by monoamine oxidase which is excreted in the urine.
|
|
|
This location is the MC location for a carcinoid tumor. It is usually _______ cm.
|
Vermiform appendix; < 2cm (which is too small for metastasis to liver)
|
|
|
From what location would a carcinoid tumor typically metastasize to the liver from and why?
|
Midgut carcinoid tumors (e.g., terminal ileum) tend to invade and ALSO metastasize. Potential for metastasis increases with size and depth of invasion. It needs to be more than 2 cm and size of invasion must be > 50%.
|
|
|
Carcinoid syndrome is characterized by what clinically? What organ can it particularly affect.
|
(1) Bronchospasms
(2) Diarrhea (3) Flushing of the skin Right side of the heart. Serotonin causes fibrosis of heart valves. |
|
|
Symptoms of carcinoid syndrome can be triggered by what?
|
(1) Drinking alcohol
(2) Emotional stress Causes release of serotonin from the tumor. |
|
|
Right sided carcinoid heart disease leads to what?
|
Right-sided valvular fibrosis.
Leads to tricuspid regurgitation and pulmonary valve stenosis. |
|
|
Why don't we get left-sided valvular disease?
|
Serotonin is broken down by MAO in the lung.
|
|
|
What is acute appendicitis?
|
Acute inflammation of appendix.
|
|
|
What is acute abdomen? (brief)
|
When a patient presents with a severe abdominal pain that is often a surgical emergency.
|
|
|
This is the MCC of acute abdomen.
|
Acute appendicitis.
|
|
|
What is acute appendicitis related to in children and adults?
|
(1) Related to obstruction of the appendix by lymphoid hyperplasia (children).
(2) In adults it is related to obstruction of appendix by fecalith. This is a general principle of pathology, you block a tube and you often get infection/inflammation. |
|
|
Pain in acute appendicitis is initially ____________ and then shifts to _______.
|
periumbilical; RLQ
|
|
|
What is a very important sign for identifying acute appendicitis in children with abdominal pain?
|
Fever
|
|
|
A man with acute appendicitis extends his leg and reports pain. What is this sign called?
|
Psoas sign
|
|
|
In acute appendicitis, pain shifts to right lower quadrant (RLQ) in ____ to ____ hours. This is due to what?
|
12;18
Irritation of different nerve fibers. Irritation of A-delta fibers on parietal peritoneum. This localizes pain to exact location. |
|
|
What is Blumberg's sign?
|
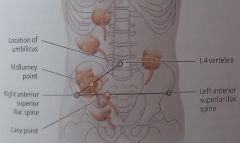
Rebound tenderness at McBurney's point.
|
|
|
What appears first in acute appendicitis; pain or nausea & vomiting?
|
Pain precedes nausea and vomiting.
|
|
|
Rupture of the appendix can result in what?
|
Rupture results in peritonitis that presents with guarding (so much pain that the patient tightens muscles to 'guard') and rebound tenderness.
|
|
|
Common complication of acute appendicitis?
|
Periappendiceal abscess.
|
|
|
What is IBD? What is its etiology?
|
Chronic relapsing inflammation of bowel. Possibly due to abnormal immune response to enteric flora.
|
|
|
Classic presentation of IBD?
|
Young women (teens to 30s) with recurrent bouts (omgang, anfall) of bloody diarrhea and abdominal pain.
|
|
|
IBD is more prevalent in the ________, particularly _________ and ____________.
|
West; Caucasians; Eastern European Jews
|
|
|
What type of diagnosis is IBD?
|
Diagnosis of exclusion because bloody diarrhea and abdominal pain mimic other causes of bowel inflammation.
|
|
|
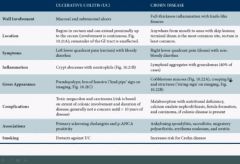
What does the word ulcerative colitis tell you about the disease itself?
|
Ulcerative tells us about the involvement of the wall; mucosal and submucosal ulcers
Colitis; involves colon |
|
|
Where does UC typically arise? How does it progress in terms of location?
|
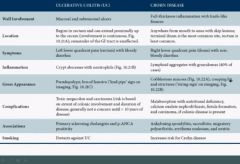
Begins in rectum and can extend proximally up to the cecum (involvement is continuous). Remainder of the GI remains unaffected. The most proximal it can go is the cecum.
|
|
|
What symptoms do we have in UC?
|
Recurrent LLQ crampy pain (rectum) with mucus and bloody diarrhea.
|
|
|
What is the key histologic hallmark of UC?
|
Crypt abscesses with neutrophils.
|
|
|
What is the gross appearance of a colon affected by UC?
|
(1) Pseudopolyps (a series of bumps that arise due to healing of the inflammatory process)
(2) Loss of haustra |
|

What is this?
|
A colon affected by ulcerative colitis.
|
|
|
Complications of ulcerative colitis.
|
(1) Toxic megacolon where patients start to appear toxic (febrile etc).
(2) Rupture (3) Carcinoma |
|
|
The risk of carcinoma in ulcerative colitis is based on what?
|
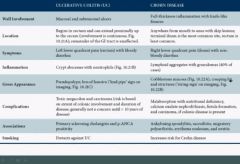
(1) Extent of colonic involvement
(2) Duration of disease |
|
|
When is carcinoma in a patient with ulcerative colitis a concern?
|
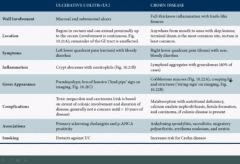
Generally not a concern until > 10 years of disease.
|
|
|
Ulcerative colitis has some associations, what are they?
|

(1) Primary sclerosing cholangitis
(2) p-ANCA positivity |
|
|
Smoking protects against _______ while it exacerbates ______.
|
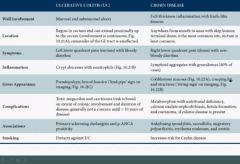
ulcerative colitis; Crohn's
|
|
|
p-ANCA should remind you of what?
|
(1) Microscopic polyangiitis
(2) Churg-Strauss (3) UC |
|
|
UC is a superficial ulceration while Crohn's disease is a __________.
|
full-thickness inflammation with knife-like fissures
|
|
|
What is the typical location of Crohn's disease?
|
MC site is terminal ileum. Can occur anywhere from mouth to anus with skip lesions. Rectum is least common site.
|
|
|
Presenting symptoms of Crohn's?
|
RLQ pain (ileum) with non-bloody diarrhea
|
|
|
What is the hallmark of Crohn's disease?
|
Lymphoid aggregates with granulomas (40% of cases).
|
|
|
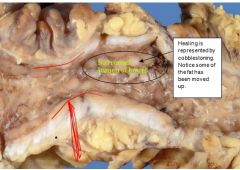
Gross appearance of the gut affected by Crohn's?
|
(1) Cobblestone appearance (rullestein/brostein)
(2) Creeping fat (comes closer to serosa due to fibrosis by healing) (3) Strictures |
|

What is this?
|
A classic 'string-sign' characteristic of Crohn's disease. Caused by strictures.
|
|
|
Complications of Crohn's disease?
|
(1) Malabsorption with nutritional deficiencies
(2) Calcium oxalate nephrolithiasis - Normally we have oxalate in gut, but we dont absorb much. Inflammation causes us to absorb more. (3) Fistula formation - Weakened wall with rupture that plugs into another tube or epithelial surface. |
|
|
There is a risk of carcinoma in Crohn's however [...]
|
Only if colonic involvement is present
|
|
|
Crohn's disease is associated with what?
|
(1) Ankylosing spondylitis
(2) Sacroiliitis (3) Migratory polyarthritis (4) Erythema nodosum (5) Uveitis |
|

What is this?
|
|

