![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
61 Cards in this Set
- Front
- Back
|
What is the goal of secondary hemostasis? How does it occur? |
Stabilize the weak platelet plug. This occurs via the coagulation cascade.
|
|
|
The coagulation cascade generates thrombin. What happens next?
|
Thrombin converts fibrinogen in the PLT plug to fibrin. Fibrin is then cross-linked, yielding a stable platelet-fibrin thrombus.
|
|
|
Activation of coagulation factors requires [...]
|
(1) Exposure to an activating substance
(2) Phospholipid surface (3) Calcium |
|
|
In what granules are calcium contained in PLTs?
|
Dense core granules
|
|
|
Disorders due to secondary hemostasis is usually due to ______________.
|
factor abnormalities.
|
|
|
Clinical features of secondary hemostasis disorders include [...]
|
(1) Deep tissue bleeding into muscles and joints
(2) Rebleeding after surgical procedure (such as wisdom tooth extraction) |
|
|
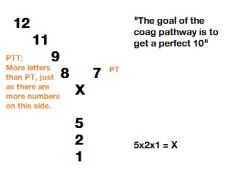
PT measures _________ and ____________.
|
extrinsic; common pathways
|
|
|
PTT measures __________ and ___________.
|
intrinsic; common
|
|
|
Draw a simple coagulation cascade.
|
|
|
|
What is an easy way of remembering that PTT is useful for monitoring heparin therapy?
|
PTT = HEP (three letters)
|
|
|
Hemophilia A is a genetic deficiency in factor ____.
|
FVIII (Hemophilia AAAIGHT/EEEEEIGHT)
|
|
|
What is the hereditary pattern of hemophilia A?
|
X-linked recessive; predominantly affects males
|
|
|
Hemophilia A can arise from a __________ without any family history.
|
new mutation... it can arise de novo in an offspring without any family history
|
|
|
Classical clinical features of a male with hemophilia A would include?
|
(1) Deep tissue bleeding
(2) Joint bleeding (3) Postsurgical bleeding Depends on degree of severity. |
|
|
What are laboratory findings in hemophilia A?
|
(1) Increased PTT, normal PT
(2) Decreased FVIII (3) Normal platelet count and bleeding time |
|
|
What is the treatment of Hemophilia A?
|
Recombinant FVIII
|
|
|
Hemophilia B is due to?
|
Genetic FIX deficiency. ("One more" than hemophilia A)
|
|
|
How does hemophilia B present clinically compared to hemophilia A?
|
Resembles hemophilia A, except FIX levels are decreased instead of FVIII.
|
|
|
What is a coagulation factor inhibitor?
|
Autoantibody against coagulation factors
|
|
|
The MC coagulation factor inhibitor is [...]
|
Anti-FVIII
|
|
|
How would you distinguish between coagulation factor inhibitor anti-FVIII in a patient with hemophilia A?
|
Mixing study. Mix plasma with normal plasma. If it correct, it is hemophilia (you replenish VIII), if it doesn't, it is due to coagulation factor inhibitor because the replenished VIII will just be bound.
|
|
|
This is the MC inherited coagulation disorder.
|
Von Willebrand Disease
|
|
|
True or false: Von Willebrand Disease is only one disease entity.
|
False. Multiple subtypes exist. Cause can be quantitative or qualitative.
|
|
|
The MC type of vWF disease is ______________________.
|
AD with decreased vWF levels
|
|
|
Patients with vWF disease will present with ________ and ___________ because low vWF impairs ____________.
|
mild mucosal bleeding; skin bleeding; platelet adhesion
|
|
|
What would the laboratory findings in vWF disease be?
|
(1) Increased bleeding time
(2) Increased PTT, normal PT (3) Abnormal ristocetin test |
|
|
What happens when you add ristocetin to a medium containing normal healthy platelets?
|
They aggregate in the presence of vWF. In its absence, they don't.
|
|
|
The treatment of vWF is ___________.
|
Desmopressin. It increases vWF release from Weibel-Palade bodies of endothelial cells.
|
|
|
Deficiency of vitamin K occurs in [...]
|
(1) Newborns.
- Lack bacterial colonization of the bowel. (2) Long-term antibiotic therapy. - Killing off the gut flora (3) Malabsorption - Fat soluble vitamin |
|
|
Breast milk contains __________ (adequate/very little) vitamin K.
|
very little
|
|
|
Failure of what organ can cause a secondary hemostatic disease, and by what pathomechanisms?
|
Liver.
(1) Decreased production of coagulation factors (2) Decreased activation of vitamin K by epoxide reductase. |
|
|
Measuring the effect of liver failure on coagulation is done using __________.
|
PT
|
|
|
What is large-volume transfusion?
|
You dilute coagulation factors, resulting in a relative deficiency.
|
|
|
Vitamin K levels normally decrease between days ___ and ____.
|
2;5
|
|
|
What is given to newborns after they are born?
|
Prophylactic shot of vitamin K.
|
|
|
What is a disease that may lead to malabsorption of vitamin K?
|
Celiac disease
|
|
|
Rat poison contains _________.
|
warfarin
|
|
|
A young child has been staying with his grandparents for a week. The grandparents brings the child your office after several bouts of epistaxis and easy bruising. The child is now hypotensive. What could you suspect?
|
Exposure to warfarin from elders
|
|
|
This is the MCC of thrombocytopenia in hospitalized patients.
|
Heparin-induced thrombocytopenia.
|
|
|
How can heparin cause thrombocytopenia?
|
Heparin can bind to platelet factor 4 on platelets, forming a complex. Autoantibodies can be formed against this complex, leading to destruction.
|
|
|
What is a feared complication of heparin-induced thrombocytopenia?
|
When it occurs, fragments of destroyed PLTs may activate remaining PLTs leading to thrombosis.
|
|
|
What anticoagulant do you NOT wanna give HIT-patients complicated with thrombosis?
|
Warfarin. In these patients there is an increased risk of coumadin skin necrosis.
|
|
|
What is the problem in DIC and what is the result?
|
Pathologic activation of the coagulation cascade. Widespread microthrombi result in ischemia and infarction. Consumption of PLTs and factors, bleeding results, especially from IV sites and mucosal surface (e.g. coughing up blood, hematuria, hematochezia).
|
|
|
DIC is almost always __________ (primary/secondary).
|
DIC is almost always secondary to another disease process.
|
|
|
List five disease processes that may lead to DIC.
|
(1) Obstetric complication
(2) Sepsis (3) AdenoCA (4) Acute promyelocytic leukemia (5) Rattlesnake bite |
|
|
Why can obstetric complications lead to DIC?
|
Amniotic fluid contains tissue factor which activates the coagulation cascade.
|
|
|
How can sepsis lead to DIC?
|
(1) Endotoxin can activate coagulation cascade
(2) Macrophages produce inflammatory mediators activating coagulation indirectly |
|
|
How can adenocarcinoma cause DIC?
|
Mucin from adenocarcinoma can activate the coagulation cascade, especially if it is metastatic.
|
|
|
How can acute promyelocytic leukemia cause DIC?
|
Cells are loaded with primary granules. They coalesce to form Auer rods. When they enter the circulation they can activate coagulation.
|
|
|
A rattlesnake bite can cause DIC by ______________.
|
injecting venom (cytohemoneurotoxin) that causes DIC. Seen with rattlesnakes, copperheads (nordamerikansk giftslange) and water moccasin (seen in southeastern US).
|
|
|
What are some laboratory findings in DIC?
|
(1) Low PLT
- We are consuming PLTs. (2) Increased PT/PTT - Everything is consumed (3) Decreased fibrinogen - It's used up (4) Microangiopathic hemolytic anemia - Microthrombi will "sheer" RBCs (5) Elevated fibrin split products (D-dimer) |
|
|
Treatment of DIC involves [...]
|
(1) Addressing the underlying cause
(2) Transfuse blood products (3) Cryoprecipitate |
|
|
What is fibrinolysis?
|
End-stage of coagulation. It's removal of a thrombus by lysing it.
|
|
|
Disorders of fibrinolysis occurs due to _____________.
|
plasmin overactivity resulting in excessive cleavage of fibrinogen
|
|
|
What is the action of plasmin after being activated by tissue plasminogen activator?
|
(1) Cleaves fibrin
(2) Cleaves serum fibrinogen (3) Destroys coagulation factors (4) Blocks PLT aggregation |
|
|
What molecule inactivates plasmin?
|
alpha2-antiplasmin
|
|
|
Provide two scenarios that may cause disorder of fibrinolysis.
|
Radical prostatectomy - In this setting, urokinase is released from the tissue causing activation of plasminogen and the release of plasmin.
Cirrhosis of liver - reduced production of alpha2-antiplasmin |
|
|
Patients with disorders of fibrinolysis present the same way as a patient with ___________.
|
DIC. They present with increased bleeding.
|
|
|
What are the laboratory findings in disorders of fibrinolysis?
|
Increased PT/PTT
- Action of plasmin on coagulation factors. Increased bleeding time (but normal PLT count) - Plasmin inhibits platelet aggregation Increased fibrinogen split products without D-dimer. |
|
|
Which one of these situations causes increase in D-dimer:
A. Plasmin cleaves a thrombus B. Plasmin cleaves fibrinogen |
A.
|
|
|
The treatment of disorders of fibrinolysis is? How does it work?
|
Aminocaproic acid. It blocks the activation of plasminogen.
|

