![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
137 Cards in this Set
- Front
- Back
|
What is the functional unit of the ovary? |
Follicle (oocyte surrounded by granulosa and theca cells)
|
|
|
LH binds to what cells? What happens?
|
Theca cells.
They produce androgens which diffuse into granulosa cells (which under FSH influence) and gets converted into estradiol. Estradiol bathes the egg. |
|
|
FSH binds to what cells?
|
Granulosa cells. Allows granulosa cells to convert androgens to estrogens (estradiol)
|
|
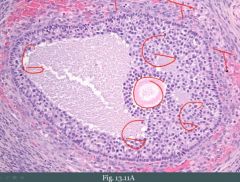
What is this?
|
Follicle
|
|
|
After ovulation, the residual follicle becomes _____________.
|
corpus luteum
|
|
|
What can happen to the corpus luteum?
|
Hemorrhage into it causing a hemorrhagic luteal cyst.
|
|

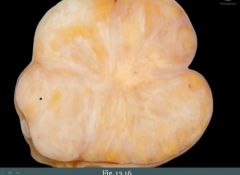
What is this? Why is it yellow?
|
Corpus luteum.
Yellow because it produces hormones (steroid hormone; progesterone) |
|
|
Degeneration of follicle results in ___________. What disorder results in multiple cysts?
|
follicular cyst
Polycystic ovarian disease |
|
|
What is PCOD? (brief) It is characterized by what?
|
Multiple follicular cysts in ovary due to hormone imbalance. Characterized by increased LH and low FSH (LH:FSH > 2)
|
|
|
What is hirsutism?
|
Excess hair in a male distribution.
|
|
|
Features of PCOD?
|
(1) Hirsutism (heavy facial hair e.g.)
(2) Obese woman (3) Infertility (4) Oligomenorrhea (5) Androgen --> Estrone will shut down FSH. - Granulosa cells are unable to perform their job and follicle degenerates and become cystic. |
|
|
Some patients with PCOD have ________________.
|
insulin resistance
|
|
|
Patients with PCOD have increased risk for what?
|
Endometrial carcinoma
|
|
|
An easy way of remember what ovarian tumors we can get.
|

|
|
|
The ovary is composed of what three cell types?
|
(1) Surface epithelium
(2) Germ cells (3) Sex-cord stroma Tumors can arise from any of these cell types or metastasis. |
|
|
What is the MC type of ovarian tumor?
|
Surface epithelial tumor
|
|
|
Surface epithelial tumors are derived from what? What is special about it?
|
From the coelomic epithelium that lines the ovary. It has the ability to produce multiple different cell types, therefore we see multiple different subtypes of potential tumors.
|
|
|
What are the two most common surface epithelial tumors? These are both usually _________.
|
(1) Serous
(2) Mucinous Both are usually cystic. |
|
|
The two most common types of surface epithelial tumors in the ovaries are classically named based on what?
|
The fluid they produce.
Full of water when you cut it open = Serous Full of mucus when you cut it open = Mucinous |
|
|
How can you categorize surface epithelial tumors?
|
Based on how they behave, e.g. benign or malignant or tumors in between (borderline tumors).
|
|
|
Benign tumors of surface epithelium of ovary are called ________. They are composed of?
|
Cystadenoma. Composed of single cyst with simple, flat lining.
|
|
|
Cystadenomas most commonly arises in?
|
Premenopausal women (30-40 yo)
|
|
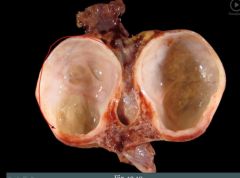
What is this?
|
Benign tumor of surface epithelium (cystadenoma)
|
|
|
What is the malignant variant of the benign tumor that arises from surface epithelium of the ovary called?
|
Cystadenocarcinoma.
Can be serous or mucinous. |
|
|
Cystadenocarcinomas are composed of what? It arises in?
|
Composed of complex cysts with thick, shaggy (almost like a carpet) lining. MC arises in postmenopausal women (60-70 yo).
|
|
|
What is the defining histologic feature of cystadenocarcinoma?
|
That cells invade into the connective tissue of the cyst wall.
|
|
|
Borderline tumors have what features?
|
Features that are in between benign and malignant.
|
|
|
Borderline tumors have better prognosis than frankly _______________ tumors, but [...]
|
malignant
but they still carry metastatic potential |
|
|
What type of ovarian carcinoma can you get with BRCA1 mutations?
|
Increases the risk for serous carcinoma of the ovary and fallopian tube.
|
|
|
Patients who have mutation in this gene have increased risk for breast cancer and ovarian cancer. What is the affected gene? What additional cancer are they at risk for?
|
BRCA1
Remember ovarian carcinoma is serous (from surface epithelium). They are at risk for fallopian cancer. |
|
|
A patient has a BRCA1 mutation. What could organ(s) could she elect to get surgically removed?
|
Breasts, ovaries, fallopian tubes
|
|
|
What types of surface epitheliai tumors of the ovary do you know?
|
(1) Serous
(2) Mucinous (3) Endometrioid (4) Brenner |
|
|
What histology does endometrioid tumor of the ovary have?
|
Endometrial-like.
|
|
|
An endometrioid tumor of the ovary is usually ___________ (benign/malignant).
|
malignant
|
|
|
What tumor may be associated with endometriosis?
|
Endometrioid carcinoma of the ovary
|
|
|
Average time of diagnosis of endometriosis is ____ to ____ yo.
|
25;29
|
|
|
A 26 year old woman comes in with complaints of pain during menstruation. During intercourse she also has pain. She has been trying to conceive but with no results. An adnexal mass is felt and confirmed to be endometrioid type of ovarian carcinoma. What should be your next concern?
|
Patients with endometrioid, in 10-15% of cases, will have a separate endometrioid tumor in the endometrium as well.
|
|
|
A biopsy of a suspected ovarian carcinoma contain cells that resemble urothelium. What might this be? Is this tumor benign or malignant?
|
Brenner's tumor.
Usually benign. |
|
|
When do surface-epithelial tumors present?
|
They present late (poor prognosis).
|
|
|
How do patients with a surface epithelial tumor of the ovary present?
|
They present late:
(1) Vague abdominal symptoms (pain, fullness) (2) Signs of compression (urinary frequency) |
|
|
You palpate the ovaries in a postmenopausal woman. Should you be able to do this?
|
Palpable ovaries in postmenopausal women is cancer until proved otherwise.
|
|
|
Epithelial tumors tend to spread _________, and especially to the _________.
|
locally; peritoneum
|
|
|
A surface-epithelial tumor of the ovaries may release this marker into the blood, what is it and what is it useful for?
|
CA-125.
It is useful for monitoring treatment response and recurrence. |
|
|
What is the second most common ovarian tumor that can arise?
|
Germ cell tumors (15% of causes)
|
|
|
Germ cell tumors usually arise in?
|
Women of reproductive age.
|
|
|
What type of tumor would you consider if a 15-30 year old presented with a tumor of the ovary? How about 35-40? 60-70?
|
15-30: Germ cell tumor
35-40: Benign surface epithelial tumor 60-70: Malignant surface epithelial tumor (top of your DDx) |
|
|
How could you easily remember what type of germ cell ovarian tumors there are?
|
Germ cells give rise to fetal tissues.
(1) One tumor that can resemble fetal tissues is called a cystic teratoma (different embryological layers) (2) You can also get fetal type tissues that's very primitive. This is embryonal carcinoma. (3) Germ cells can make the yolk sac --> Yolk sac tumor. (4) Germ cells can make additional germ cells. When we get a mass of germ cells we get a dysgerminoma. (5) Oocyte/egg has to make placenta --> choriocarcinoma. |
|
|
What is a cystic teratoma?
|
Cystic tumor composed of fetal tissue derived from two or three embryologic layers (germ cell tumor).
|
|
|
This is the MC germ cell tumor in females.
|
Cystic teratoma.
|
|
|
True or false: Cystic teratomas are always unilateral.
|
False, they are bilateral in 10% of cases.
|
|
What could this be?
|
Cystic teratoma (benign).
|
|
|
Cystic teratomas are _________ (benign/malignant)
|
Benign
|
|
|
What do we have to exclude when we have a cystic teratoma?
|
(1) Immature tissue, it has malignant potential.
(2) The tissue itself can contain a malignancy (somatic malignancy) - E.g., carcinoma in the skin |
|
|
What's the MC type of tissue that's immature in an immature teratoma?
|
Neuroectoderm
|
|
|
What is the MC somatic malignancy that arises in a teratoma?
|
Squamous cell carcinoma of the skin of the teratoma.
|
|
|
This is a special type of teratoma, what's the name and what's so special about it?
|
Struma ovarii: Cystic teratoma composed primarily of thyroid tissue.
|
|
|
What is a dysgerminoma composed of?
|
This is a germ cell tumor. Composed of large cells with clear cytoplasm and central nuclei (resembles oocyte).
|
|
|
What is the MC malignant germ cell tumor?
|
Dysgerminoma (most common benign is cystic teratoma).
|
|
|
The testicular counterpart of a dysgerminoma is a?
|
Seminoma
|
|
|
What is the prognosis of a dysgerminoma?
|
Good. Responds to radiotherapy.
|
|
|
What tumor marker may be elevated with a dysgerminoma?
|
LDH
|
|
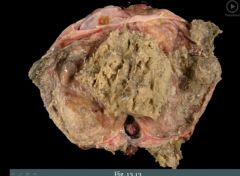
What is this?
|
Dysgerminoma.
|
|
|
What is an endodermal sinus tumor?
|
Germ cell tumor. Malignant tumor that mimics the yolk sac.
("Sinus = Yolk sac") |
|
|
What is the MC germ cell tumor in children?
|
Endodermal sinus tumor.
|
|
|
A five year old girl has an ovarian mass. What serum tumor marker may be elevated?
|
This is most likely an endodermal sinus tumor and AFP may be increased.
|
|
|
What do we see on histology of an endodermal sinus tumor?
|
Schiller-Duval bodies (glomeruloid structures)
|
|
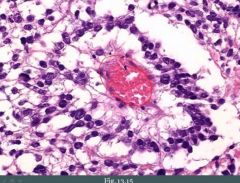
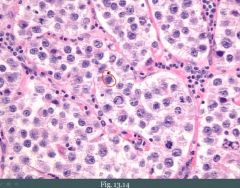
This biopsy was taken from a young girl. What could it be?
|
Schiller-Duval body, could be taken from an endodermal sinus tumor.
|
|
|
What is a choriocarcinoma? What is it composed of?
|
Germ cell tumor, a malignant proliferation of placental-like tissue. Composed of trophoblasts and syncytiotrophoblasts (villi are absent).
|
|
|
What key cell surrounds the villi in the placenta?
|
Trophoblasts
|
|
|
Choriocarcinoma: How does it classically look? Does it spread?
|
(1) Small, hemorrhagic tumor
(2) Early hematogenous spread - It's genetically programmed to invade blood vessels from the very beginning (trophoblasts are designed to invade and find blood vessels). |
|
|
What serum marker may we see with choriocarcinoma?
|
Syncytiotrophoblasts may produce beta-hCG
|
|
|
True or false: Patients with a choriocarcinoma have a poor response to chemotherapy.
|
True
|
|
|
What is an embryonal carcinoma? What is it composed of?
|
Germ cell tumor. Composed of large primitive cells.
|
|
|
An embryonal carcinoma is ________________ (only locally destructive/aggressive with early metastasis).
|
Aggressive with early metastasis.
("Embryonal indicates something very immature and less differentiated and therefore more aggressive. Primitive cells also have the ability to move and spread naturally, that's what they do") |
|
|
Sex-cord stromal tumors are tumors that resemble ___________.
|
the normal sex-cord stroma tissues of ovary
|
|
|
What is a granulosa-theca cell tumor? (brief)
|
A sex-cord stromal tumor. It is a neoplasm of granulosa and theca cells.
|
|
|
A granulosa-theca cell tumor often produces __________.
|
estrogen
|
|
|
How does a granulosa-theca cell tumor present?
|
Presents with signs of estrogen excess (symptoms vary with age). Can present at any age.
|
|
|
What is a sertoli-Leydig cell tumor?
|
Tumor that mimics the sex-cord stromal elements of the testicle. Ovaries and testicles have same embryological origin.
|
|
|
How would a sertoli-leydig cell tumor look like histologically?
|
(1) Sertoli cells form tubules
(2) Leydig cells contain characteristic Reinke crystals |
|
|
How could a woman with a sertoli-leydig cell tumor present?
|
May produce androgen; associated with hirsutism (hair in a male distribution) or virilization.
|
|
|
What is a fibroma?
|
Sex-cord stromal tissue. Benign tumor of fibroblasts.
|
|
|
Fibroma is associated with a strange syndrome. Describe.
|
Meig's syndrome in a subset of patients with a fibroma. Shows up as pleural effusion and ascites.
Photo shows fibroma, note the white bands. |
|
|
What is a Kruckenberg tumor?
|
A mucinous carcinoma from some other site that has metastasized to both ovaries. The primary site for such a tumor classically would be from a gastric carcinoma (diffuse subtype). A tumor from breast could cause this as well, e.g. a breast cancer with signet cells such as lobular carcinoma. Another example would be colon cancer.
|
|
|
How could we tell whether a tumor that is mucinous is a metastatic mucinous tumor to the ovary or a primary tumor?
|
If it involves one or both of the ovaries.
|
|
|
Abundant amount of mucin in the peritoneal cavity is called _____________. What tumor usually can cause this?
|
Pseudomyxoma peritonei ("Gelly belly").
A tumor within the appendix; a mucinous carcinoma of the appendix. Often it will also have metastasized to the ovary. |
|
|
What is ectopic pregnancy?
|
Implantation of a fertilized ovum at a site other than the uterine wall.
|
|
|
MC site of ectopic pregnancy?
|
Fallopian tube (lumen)
|
|
|
What is a key risk factor for ectopic pregnancy?
|
Scarring
(1) PID (2) Endometriosis |
|

What is this?
|
Ectopic pregnancy (ruptured)
|
|
|
Classic presentation of ectopic pregnancy?
|
(1) Lower quadrant pain weeks after missed period
It's a surgical emergency. |
|
|
What should you consider doing when a woman (pregnancy range of age) with severe lower abdominal pain comes in?
|
Pregnancy test (initial test)
|
|
|
What is a spontaneous abortion? (brief)
|
Miscarriage of a fetus (foster), usually occurs < 20 weeks of gestation
|
|
|
Spontaneous abortion is relatively ________ (rare/common).
|
common
|
|
|
How frequently does spontaneous abortions occur?
|
Recognizable in up to 1/4 of all pregnancies
|
|
|
How do women with spontaneous abortion present?
|
(1) Vaginal bleeding
(2) Cramp-like pain (3) Passage of fetal tissue |
|
|
Spontaneous abortion is most often due to what?
|
Chromosomal anomalies.
|
|
|
Aside from chromosomal anomalies, what are some causes of spontaneous abortion?
|
(1) Hypercoagulable states (e.g., lupus anticoagulant)
(2) Congenital infection (3) Exposure to teratogens |
|
|
When you have exposure to a teratogen within the first two weeks of embryogenesis that can result in __________.
|
spontaneous abortion
|
|
|
If exposure to a teratogen occurs between weeks 3 to weeks 8 there is a risk of ______________. After that, any time from months 3 to months 9 there is a risk of __________.
|
organ malformation; organ hypoplasia
|
|
|
Alcohol as a teratogen is the MC cause of ___________.
|
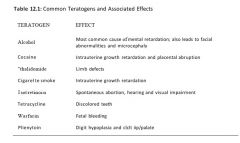
mental retardation
|
|
|
Cocaine as a teratogen can lead to ___________ and __________.
|
Intrauterine growth retardation, placental abruption (constriction)
|
|
|
Thalidomide was withdrawn form the market. It was initially helpful for morning sickness in pregnant women. What did it cause?
|
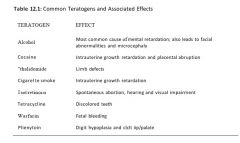
Limb defects
|
|
|
What is the significance of cigarette smoke as a teratogen?
|
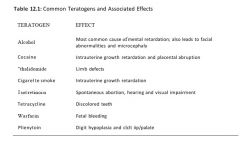
Intrauterine growth retardation, increases risk for sudden death after birth
|
|
|
What is the significance of isotretinoin as a teratogen?
|
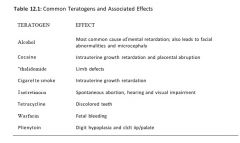
Spontaneous abortion, hearing and visual impairment
|
|
|
What is the significance of tetracycline as a teratogen?
|
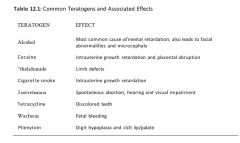
Discolored teeth
|
|
|
What is the significance of warfarin as a teratogen?
|
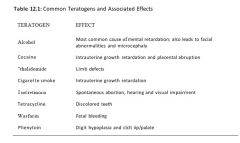
Fetal bleeding
|
|
|
What is the significance of phenytoin as a teratogen?
|
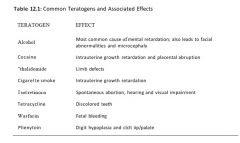
Digit hypoplasia, cleft lip and palate
|
|
|
What is placenta previa? How does it present?
|
Implantation of previa in the lower uterine segment. Placenta overlies the cervical os. It presents as third trimester bleeding.
("You're getting a _preview_ [previa] of the placenta") |
|
|
Placenta previa often requires what action to be taken? And why?
|
Delivery of fetus by C-section.
Baby can compress the placenta and therefore its blood supply. |
|
|
What is placental abruption? This is a common cause of _________.
|
Placenta abruptly begins to separate from the uterine wall (decidua).
It's a common cause of still birth. |
|
|
Placental abruption presents with [...]?
|
Third trimester bleeding and fetal insufficiency.
|
|
What is this?
|
Placental abruption. Note the blood and blood clots on the surface.
|
|
|
What is placenta accreta?
|
Improper implantation of placenta into myometrium with little or no intervening decidua.
|
|
|
How does placenta previa present?
|
Presents with difficulty delivery of the placenta and post-partum bleeding.
|
|
|
Placenta accretia often requires _____________.
|
hysterectomy (placenta can't be removed and the mother loses a lot of blood)
|
|
|
What is preeclampsia? When does it arise?
|
Pregnancy-induced HTN and proteinuria (with edema). It's a problem with the maternal-fetal vascular interface (kontaktflate) in placenta.
Arises in the third trimester. |
|
|
Preeclampsia is seen in about ____ % of pregnancies.
|
5%
|
|
|
How severe is the HTN in preeclampsia? Based on this, what would you expect to see in the vessels of the placenta?
|
Can be severe (almost malignant HTN) where patients get headaches and visual abnormalities.
Fibrinoid necrosis. |
|
|
What is eclampsia?
|
Preeclampsia with seizures
|
|
|
Eclampsia mandates what action to be taken?
|
Removal of placenta.
|
|
|
Preeclampsia can be part of what syndrome? Describe it.
|
HELLP
H - Hemolysis EL - Elevated liver enzymes LP - Low platelets This is an example of a thrombotic microangiopathy involving the liver. |
|
|
What is sudden infant death syndrome?
|
Death of healthy infant (1 month to 1 year) without cause. Usually during sleep.
|
|
|
Risk factors for sudden infant death syndrome?
|
(1) Sleeping on stomach
(2) Smoking in household (3) Prematurity |
|
|
What is hydatidiform mole?
|
Instead of growing a baby you grow abnormal placental tissue. The villi are swollen and edematous with proliferation of trophoblasts.
|
|

A pregnant woman is in your office for a checkup early first trimester. On ultrasound you notice that her uterus is abnormally large and you notice a "snowy" appearance on the screen. No fetal heart sounds are heard. Her beta-hCG is higher than expected. What could it be?
|
Hydatidiform mole
|
|

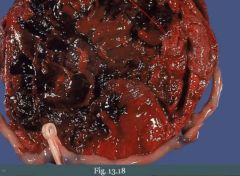
What is this?
|
Grapelike mass (edematous villi) that a woman with hydatidiform mole can begin to pass, especially is she hasn't received any prenatal care.
|
|
|
Hydatidiform mole usually presents when?
|
In early second trimester.
|
|
|
After you determine that a woman has a molar pregnancy, what do you have to do?
|

Classify it, they are either complete or partial.
|
|
|
What type of hydatidiform mole has the highest risk for progression to cancer? What type of cancer is it?
|
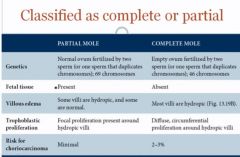
Complete (2-3%); choriocarcinoma
("A complete mole has the 'complete' risk of choriocarcinoma") |
|
|
How does hydatidiform mole occur and how could you remember properties that classify a mole as partial or complete?
|

"It's dads' fault!"
(1) Two sperm enter an empty ovum. All genetic material is from dad (completely from dad). This is a complete mole (46 chrom). There is no fetal tissue in this case. (Complete mole, no baby tissue). All villi are edematous ("Completely edematous"). Trophoblasts proliferate all around the circumference of a villus (completely). Beta-hCG is higher than partial. |
|
|
How does partial hydatidiform mole arise?
|
Two sperm from dad enters an ovum with moms genetic material. Gives 69 chromosomes.
|
|
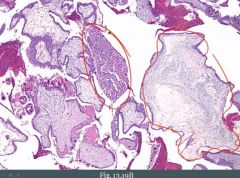
What is this?
|
Hydatidiform mole.
Encircled (left): Proliferation of trophoblasts Encircled (right): Massively dilated villi |
|
|
Treatment of molar pregnancy? Consequence of procedure?
|
Dilatation and curettage. Beta-hCG is monitored to ensure adequate mole removal and to screen for development of choriocarcinoma.
Asherman syndrome. |
|
|
When does a choriocarcinoma classically develop in context of complete mole?
|
Usually within the first year of removal.
|
|
|
Choriocarcinoma comes in two "flavors". Elaborate.
|
(1) Gestational pathway
- Could arise as complication of spontaneous abortion - Normal pregnancy - Hydatidiform mole (2) Spontaneous (germ cell pathway) |
|
|
A choriocarcinoma can arise via two pathways. How do the cancers from their respective pathways respond to chemotherapy?
|
(1) Spontaneous one does NOT respond well to treatment
(2) Gestation pathway-cancer responds well to chemotherapy (methotrexate) - Excellent response, they "melt" away. |

