![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
|
What do we call an accumulation of mature myeloid cells? |
Myeloproliferative disorder
|
|
|
If RBCs are overproduced, what do we call that?
|
Polycythemia vera
|
|
|
If granulocytes are overproduced what do we call that?
|
CML
|
|
|
Of megakaryocytes or platelets are overproduced, what do we call that?
|
Essenetial thrombocytemia
|
|
|
True or false: In myeloproliferative disorders, you get a proliferation of one cell lineage at a time.
|
False. Actually, it involves every single lineage. However, we name it based on the predominant cell type.
|
|
|
What age group do we see myeloproliferative disorders in?
|
it is a disease of late adulthood
|
|
|
What do we see in marrow and on count in myeloproliferative disorders?
|
Results in high WBC count (granulocytes) and hypercellular marrow
|
|
|
Complications that are common in myeloproliferative disorders include?
|
(1) Increased risk for hyperuricemia and gout (lets say you overproduce RBCs, the marrow spits out all the nuclei and those nuclei has to be degraded)
(2) Progression to marrow fibrosis |
|
|
Progression to marrow fibrosis is called the?
|
Spent phase
|
|
|
Many myeloproliferative disorders can progress to what?
|
Acute leukemia (accumulating mutations)
|
|
|
CML is proliferation of what?
|
Neoplastic proliferation of mature myeloid cells, especially granulocytes
|
|
|
What cell type is characteristically increased in CML?
|
Basophilia
CML is also the only leukemia with thrombocytosis. |
|

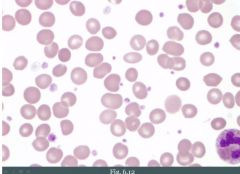
This might be?
|
Chronic myeloid leukemia, look at all the neutrophils, a myeloid precursor cell in the bottom and basophil.
|
|
|
CML is driven by what?
|
t(9;22), a BCR-ABL fusion gene
|
|
|
First line treatment of CML is what?
|
Imatinib, which blocks tyrosine kinase activity.
|
|
|
In CML, _____________ is common. What phase does this correspond to?
|
Splenomegaly.
Chronic phase. |
|
|
You can divide CML into three phases, what are they?
|
(1) Chronic phase
(2) Accelerated phase (3) Transformation phase (acute leukemia) |
|
|
A man with CML has had stable splenomegaly for some time. All of a sudden it enlarges. What phase does this correspond to?
|
Accelerated phase
|
|
|
When does transformation in CML occur?
|
Usually shortly after accelerated phase
|
|
|
Transformation, when it occurs in CML can result in either ________ or _________.
|
AML (2/3) or ALL (1/3)
|
|
|
What cell proliferates in CML?
|
Because CML can transform into either ALL or AML, it must be at the level of the HSC.
|
|
|
What is a leukemoid reaction?
|
Physiologic response to stress or infection
|
|
|
On a smear, you observe a bunch of granulocytes and early percursors. What is your differential diagnosis?
|
(1) Acute infection
(2) CML |
|
|
How can you make the distinction between a leukemoid reaction and CML?
|
(1) CML granulocytes are LAP negative (secondary granules)
- Cells of CML have no intention of fighting an infection, they are basically having a party. That's why LAP is negative. (2) CML is associated with increased basophils. (3) CML granulocytes exhibit t(9;22) |
|
|
What is polycythemia vera?
|
Myeloproliferative disorder with neoplastic proliferation of mature myeloid cells, especially RBCs.
|
|
|
What cells are increased in polycythemia vera?
|
RBCs especially, but also granulocytes and platelets.
|
|
|
Polycythemia vera is associated with a ________ mutation.
|
JAK2 kinase mutation
|
|
|
Clinically, patients with PV are going to get symptoms of what?
|
Symptoms of hyperviscosity.
(1) Blurry vision, headache (2) Increased risk of venous thrombosis (hepatic v.; budd chiari) (3) Flushed face due to congestion (4) Itching after bathing (they also have extra mast cells) |
|
|
Treatment of PV?
|
Phlebotomy.
Second-line is hydroxyurea. |
|
|
In PV, without treatment, death will usually occur within __________.
|
one year
|
|
|
PV must be distinguished from what?
|
Reactive polycythemia
|
|
|
List the oxygen saturation and EPO findings in PV, lung disease and ectopic EPO production.
|
PV: SaO2 normal, EPO is decreased (negative feedback)
Lung disease: SaO2 decreased, EPO increased Ectopic EPO: SaO2 is normal, EPO is high |
|
|
A tumor that typically produces EPO?
|
Renal cell carcinoma
|
|
|
What cells are increased in essential thrombocythemia?
|
Especially PLTs. RBCs and granulocytes are also increased.
|
|
|
Essential thrombocythemia is associated with what mutation?
|
JAK2 kinase mutation
|
|
|
What should you think about when you see tons of platelets in a blood smear?
|
Essential thrombocythemia
Iron deficiency anemia (reactive phenomenon) |
|
|
What are the symptoms of essential thrombocythemia?
|
Increased risk of bleeding (underfunctioning PLTs) and/or thrombosis (overfunctioning)
|
|
|
Most myeloproliferative disorders have the ability to ___________, however ET rarely progresses to ___________ or _________.
|
burn out; marrow fibrosis; acute leukemia
|
|
|
In what myeloproliferative disorder is there NOT an increased risk for hyperuricemia and gout?
|
ET. No nucleus in PLTs.
|
|
|
What is myelofibrosis? What mutation is it associated with?
|
A myeloproliferative disorder. Neoplastic proliferation of mature myeloid cells, especially megakaryocytes.
Associated with a JAK2 kinase mutation. |
|
|
Why is it called myeloFIBROSIS?
|

Because megakaryocytes produce excess PDGF and this results in marrow fibrosis.
We see way too much fibrosis on the picture. Should be fat and bone marrow elements. |
|
|
Clinical features of myelofibrosis include? Explain each feature.
|
(1) Splenomegaly due to extramedullary hematopoiesis (fibrosis --> no hematopoiesis in marrow --> hematopoiesis in spleen)
(2) Leukoerythroblastic smear (WBC and RBC immature cells in blood because spleen does not have a reticulin gate preventing their departure from the marrow) (3) Increased risk for infection, thrombosis, bleeding (marrow is gone; spleen is tiny compared to bone marrow, it cannot produce sufficient amounts. |
|
|
What prohibits cell from exciting the marrow when they are too immature?
|
reticulin "gates"
|
|
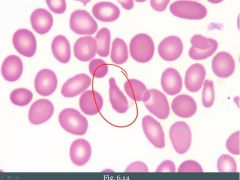
In what myeloproliferative disease do we see these cells?
|
Myelofibrosis.
Think of it like this: Some hematopoiesis still occurs in marrow, but it is highly fibrosed and cells get stretched as they try to leave the bone marrow. |

