![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
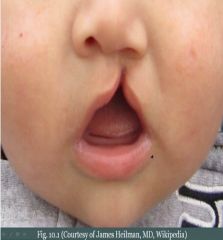
Full-thickness defect of lip &/or palate due to the failure of the facial prominences (5) to fuse.
|
Cleft lip and palate
|
|
|
Painful, superficial ulceration of the oral mucosa. Arises in relation to stress and resolves spontaneously, but often recurs. Characterized by a grayish base (represents granulation tissue) surrounded by erythema.
|
Apthous Ulcer
|
|
What
|
Cleft lip and Palate
|
|

What & Characterized by
|
Apthous Ulcer (Canker sore). Grayish base (represents granulation tissue) surrounded by erythema.
|
|
|
Recurrent apthous ulcers, genital ulcers, and uveitis. Due to immune complex vasculitis involving small vessels. Can be seen after viral infection, but etiology is unknown.
|
Behcet Syndrome
|
|
|
Vesicles involving oral mucosa that rupture, resulting in shallow painful, red ulcers. Usually due to HSV-1 (Can be HSV-2). Primary infection (Childhood)->Lesion heals->Virus remains dormant in ganglia of trigeminal nerve. Reactivation due to stress and sunlight leading to vesicles that often arise on the lips (Cold Sore).
|
Oral Herpes
|
|

What & Cause
|
Cold Sore; HSV-1 (Can be HSV-2)
|
|
|
Malignant neoplasm of squamous cells lining the oral mucosa. Tobacco and alcohol are major risk factors. Floor of the mouth is the most common location.
|
Squamous Cell Carcinoma of the oral mucosa
|
|
|
Leukoplakia: A white plaque that cannot be scraped away; Often represents SC dysplasia.
Erythroplakia: A red plaque representing vascularized (angiogenesis) leukoplakia and is highly suggestive of squamous cell dysplasia. |
Precursor lesions to SCC of the oral mucosa
|
|
|
Immunocompromised individuals (e.g. AIDS).
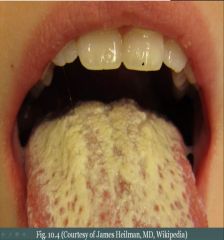
Oral candidiasis: A white deposit of the tongue that can be easily scraped away. Due to Candida albicans (alba = white). Hairy leukoplakia: A white, rough ('hair') patch that arises on the lateral tongue due to EBV-induced squamous cell hyperplasia. Not pre-malignant! |
Leukoplakia look alikes
|
|
What & Cause
|
Oral Candidiasis (Thrush); Candida albicans (alba = white) in immunocompromised.
|
|
|
Salivary Glands (What, Major (3), & Minor)
|
Exocrine glands that secrete saliva.
Major: Paroid, Submandibular, Sublingual. Minor: Microscopic glands distributed throughout the oral mucosa. |
|
|
Benign tumor gross characteristics (3)
|
1. Mobile: Hasn't invaded local tissue.
2. Painless: Hasn't invaded nerves. 3. Circumscribed: Is distinct from surrounding tissue. |
|
|
A paramyxovirus. Pacreatitis, Bilateral inflamed parotid glands (Parotitis), Orchitis, and aseptic Meningitis. Can cause sterility (especially after puberty). Serum amylase is increased (Salivary gland or Pancreatic involvement).
Mnemonic: ... makes your parotid glands and testes as big as POM-poms. |
Mumps Virus
|
|
|
Inflammation of the salivary gland most commonly due to sialolithiasis (an obstructing stone) leading to S aureus infection (Usually unilateral).
|
Sialadenitis
|
|
|
Benign tumor composed of stromal (e.g. cartilage) and epithelial tissue. Most common tumor of the salivary gland. Usually arises in parotid as a mobile, painless, circumscribed mass at the angle of the jaw. High recurrence rate due to incomplete resection (Extensions of small islands of tumor through the tumor capsule). Rarely transforms into carcinoma, which would present with signs of facial nerve damage/palsies (Facial nerve runs through parotid gland).
|
Pleomorphic Adenoma
|
|
|
Biphasic tumor (What & Example-think parotid)
|
Tumor that contains 2 types of tissue; Pleomorphic adenoma.
|
|
|
Benign cystic tumor with abundant lymphocytes and GCs (Lymph-node like stroma). 2nd most common type of salivary gland tumor that almost always arises in the parotid (Separates from adjacent stroma late in embryological development). Not uncommon to see LN associated with the parotid.
|
Warthin Tumor
|
|
|
Malignant tumor composed of mucinous and squamous cells. Most common malignant tumor of the salivary gland. Usually arises in the parotid and involves the facial nerve.
|
Mucoepidermoid Carcinoma
|
|
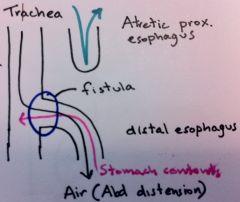
What
|
Tracheoesophageal Fistula
|
|
|
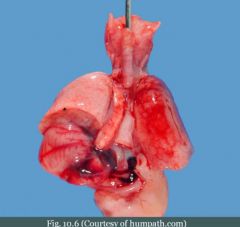
Congential defect resulting in a connection between the esophagus and trachea. Most common variant consists of proximal esophageal atresia with the distal esophagus arising from the trachea. Presents with vomiting, polyhydramnios, abdominal distension, and aspiration.
|
Tracheoesophageal Fistula
|
|
|
Determinants of the amount of amniotic fluid (2)
|
Production by babies kidney - Uptake by baby (Swallowing/Digestion).
|
|
|
Thin protrusions of esophageal mucosa, most often in upper esophagus. Can cause obstruction. Present w/ dysphagia for poorly chewed food. Increased risk for esophageal SCC.
|
Esophageal Web
|
|
|
Dysphagia due to esophageal webs, Atrophic glossitis (Beefy red tongue), and Anemia. All due to Fe deficiency. Increased risk for esophageal SCC.
|
Plummer-Vinson Syndrome
|
|

What (Top & Bottom)
|
Top: Esophageal Web; Bottom: Zenker Diverticulum
|
|
|
False Diverticulum (What & Example)
|
Does not involve all the layers of the wall of the GI tract (e.g. Zenker Diverticulum)
|
|
|
Outpouching of pharyngeal mucosa through an acquired defect in the muscular wall (False diverticulum) caused by abnormal pressure in the pharynx while swallowing (Usually due to disordered/impaired swallowing). Arises above the esophageal sphincter at the junction of the esophagus and pharynx. Patient presents with "something in the back of my throat", dysphagia, obstruction, and halitosis (bad breath). Dianosed by barium swallow.
|
Zenker Diverticulum
|
|
What
|
Tracheosophageal fistula
|
|
|
Dilated submucosal veins in the lower esophagus. Arises secondary to portal hypertension. Asymptomatic, but can rupture leading to painless hematemesis (Most common cause of death in cirrhosis). Compounded by coagulopathy since liver is not producing coagulation factors as well as a normal liver.
|
Esophageal Varices
|
|
|
Longitudinal laceration of mucosa at the GE junction caused by severe vomiting, usually due to alcoholism or bulimia. Presents w/ painful hematemesis. Risk of Boerhaave syndrome (Rupture of esophagus leading to air in the mediastinum and subcutaneous emphysema)
|
Mallory-Weiss Syndrome
|
|
What
|
Mallory-Weiss Syndrome
|
|
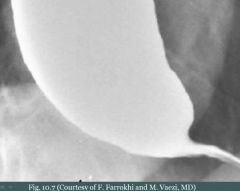
What & Disorder
|
'Bird-beak' sign; Achalasia
|
|
|
Reflux of acid from the stomach due to reduced LES tone. Risk factors HIATAL HERNIA, EtOH, tobacco, obesity, fat-rich diet, and caffeine. Characterized by heartburn (mimics cardiac chest pain), asthma (Adult-onset) and cough, damage to the enamel of the teeth. Late complications include ulceration w/ stricture and Barret esophagus are late complications.
|
Gastroesophageal Reflux Disease - GERD
|
|
|
Ulceration (What, Consequence)
|
Complete knockout of mucosa (contains stem cells), so it heals with fibrosis leading to a stricture.
|
|
|
Metaplasia of lower esophageal mucosa from stratified squamous epithelium to noncilitated columnar epithelium w/ goblet cells (Response of lower esophageal stem cells to acidic stress). Seen in 10% of patients w/ GERD. May progress to dysplasia and adenocarcinoma.
|
Barrett Esophagus
|
|
|
Esophageal Carcinoma (Sub-classifications (What, Cause, Prevalence), Presentation, LN Spread)
|
1. Adenocarcinoma: Malignant proliferation of glands that arises from pre-existing Barret esophagus and usually involves the lower 1/3 of esophagus. Most common type of esophageal cancer of the West.
2. SCC: Malignant proliferation of squamous cells due to irritation and usually arises in the upper 2/3 of the esophagus. Irritation includes EtOH and tobacco (most common causes), very hot tea, achalasia and esophageal web (rotting food), esophageal injury (e.g. lye ingestion). Presentation: Usually presents late (Poor prognosis), progressive dysphagia (solids to liquids), weight loss, pain, hematemesis. SCC may additionally present w/ hoarse voice (recurrent laryngeal nerve involvement) and cough (tracheal involvement). LN spread depends on location of cancer: Upper 1/3 - Cervical nodes, Middle 1/3 - Mediastinal or tracheobronchial nodes, Lower 1/3 - Celiac and gastric nodes. |
|
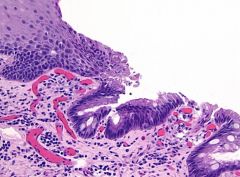
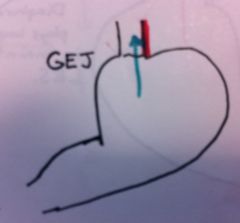
What & Histology
|
Barrett Esophagus; NKSSE to NCCE w/ goblet cells
|
|
|
Congenital malformation of the anterior abdominal wall leading to exposure of abdominal contents.
|
Gastroshisis
|
|
|
Persistent herniation of bowel into umbilical cord due to the failure of herniated intestines to return to the body cavity during development. Contents are covered by peritoneum and amnion of the umbilical cord.
|
Omphalocele
|
|
|
Congenital hypertrophy of pyloric smooth muscle. More common in males. Classically presents 2 weeks after birth as projectile nonbilious vomiting, visible peristalsis, Olive-like mass in abdomen (Can be felt on PE). Tx is myotomy.
|
Pyloric Stenosis
|
|

What
|
Gastroschisis
|
|

What
|
Omphalocele
|
|
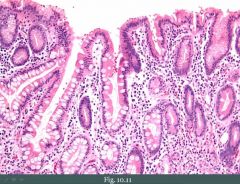
Biopsy of stomach (What, Changes, Type)
|
Chronic gastritis; Goblet cells indicating intestinal metaplasia.
|

