![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
94 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
location of ischemia in angina. Exception? |
subendocardial ischemia
EXCEPT in Prinzmetal Angina, which occludes proximally due to vasospasm and causes TRANSmural ischemia |
|
|
|
nitroglycerin MOA
|
vasodilate arteries and veins
NO increases the level of cGMP within the cell. cGMP then activates myosin light chain phosphatase via a cGMP-dependent protein kinase. |
|
|
|
angina =
|
REVERSIBLE injury to myocytes
|
|
|
|
EKG finding in angina
|
ST segment depression -- representation of subendocardial ischemia
|
|
|
|
Prinzmetal angina
|
episodic chest pain unrelated to exertion
|
|
|
|
ST segment depression indicates
|
subendocardial ischemia
|
|
|
|
ST segment elevation indicates
|
transmural ischemia
|
|
|
|
Disease associated with vasospasm's in the coronary artery
|
prinzmetal angina
|
|
|
|
MOA of Kawasaki's causing MI
|
vasospasm causes inflammation or damage to endothelial tissue exposing sub-endothelial collagen and Tissue Factor and other pro-coagulants leading to formation of thrombus
|
|
|
|
chest pain radiating to left arm or jaw
|
MI
|
|
|
|
Nitroglycerin used for?
Not used for? |
used for angina. Not used for MI
|
|
|
|
List most common coronary arteries of infarction
|
Left Anterior Descending(LAD)
Right Coronary Artery(RCA) Left Circumflex Artery(LCX) |
|
|
|
Left Anterior Descending occlusion affects
|
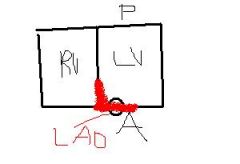
Anterior wall of left ventricle and septum
|
|
|
|
Right Coronary Artery affects
|
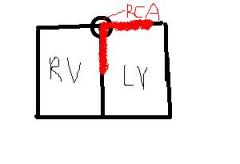
Posterior wall of left ventricle and septum
|
|
|
|
Left Circumflex Artery occlusion affects
|
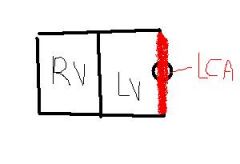
Lateral wall of left ventricle
|
|
|
|
MI spares which parts of heart?
|
Right Atria, Right Ventricle, Left Atria
|
|
|
|
What cardiac enzyme useful to test for reinfarction after an MI
|
CK-MB.
Troponin would be elevated due to prior MI, but CK-MB is transiently elevated after MI and should go down within 2 days. If a week later, you have ANOTHER infarction, it should obviously be elevated again. |
|
|
|
Key complication one day after MI
|
arrhythmia
|
|
|
|
Milestones Post-MI
|
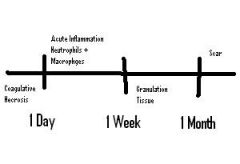
Within 1 Day, you get coagulation necrosis
Within 1 Week, you get acute inflammation with recruitment of neutrophils then macrophages Within 1 Month, you get the creation of granulation tissue After 1 Month, you get scar formation. |
|
|
|
Complication associated with neutrophil infiltration post MI
|
1-3 days
fibrinous pericarditis which presents with chest pain with friction rub due to inflammatory debris entering pericardium. Notably, this ONLY occurs with a TRANSmural infarction |
|
|
|
Complication associated with macrophage infiltration after an MI
|

4-7 days
RUPTURE Rupture of left ventricular wall --> cardiac tamponade Rupture of Interventricular septum --> left-to-right shunt Rupture of papillary muscle of the mitral valve --> mitral insufficiency(blood re-enters left atria during systole) |
|
|
|
Which artery feeds papillary muscle of mitral valve?
|
Right Coronary Artery
|
|
|
|
Dressler's Syndrome
|
Exposure of antigens in pericardium to immune systems which causes auto-immune pericarditis that happens 6-8 weeks post-infarction. Fibrinoid pericarditis.
|
|
|
|
Orthopnea
|
Dyspnea while laying flat over just a few minutes
|
|
|
|
Paroxysmal Nocturnal Dyspnea
|
Dyspnea while laying flat over few hours due to increased venous return while lying flat
|
|
|
|
Heart failure cells arise because?
|
capillaries that burst lead to intra-alveolar hemorrhage. Macrophages come in and eat all the RBC's which cause them to accumulate iron. These are called hemosiderin-laden macrophages or "heart failure" cells.
|
|
|
|
What happens in CHF?
|
Pulmonary congestion leads to pulmonary edema
Decreased Forward perfusion |
|
|
|
Complications of decreased forward perfusion?
|
Decreased forward perfusion causes the activation of the Renin-Angiotensin system. This causes eventual vasoconstriction, which increases afterload and blood volume increase. Both of which cause the heart to work harder ==> BAD.
|
|
|
|
Mainstay treatment of CHF?
|
ACE inhibitors
|
|
|
|
MCC of Right sided heart failure?
|
Left sided heart failure
|
|
|
|
MOA leading to Right heart failure due to Chronic Lung Disease
|
Lung blood vessels have a natural response to constrict when they are hypoxic as a mechanism to accomodate. However, if the entire lung does this, you raise pulmonary resistance and the right heart has to work harder which can lead to failure(cor pulmonale)
|
|
|
|
Cor pulmonale
|
Right heart dilation due to increased resistance in pulmonary vessels
|
|
|
|
Nutmeg liver
|
A result of congestive heart failure and backup of blood into the hepatic veins.
|
|
|
|
Clinical features of right heart failure
|
Jugular Venous Distention(since this feeds into right heart)
Painful hepatosplenomegaly along with possible "cardiac" cirrhosis of liver Dependent pitting edema due to increased hydrostatic pressure |
|
|
|
Most common congenital defect?
|
VSD
A/w? |
Fetal Alcohol Syndrome
|
|
|
Most common type of ASD? Less common ASD A/w?
|
Ostium Secundum
Ostium Primum A/w Down's Syndrome |
|
|
|
Paradoxical embolus A/w what cardiac defect?
|
ASD
|
|
|
|
Describe the splitting A/w ASD's
|
The extra volume due to the L-->R shunt causes the pulmonic valve to stay open longer. That is, the aortic valve closes and then the pulmonic valve follows.
|
|
|
|
PDA is A/w?
|
Congenital Rubella
|
|
|
|
PDA arises where in relation to the branches of the aorta?
|
After the major upper extremity branches. Therefore after birth, there is a L-->R shunt due to the PDA.
Can lead to Eisenmenger Syndrome due to eventual switch to the R-->L shunt. Will result in LOWER EXTREMITY CYANOSIS. |
|
|
|
What classic congenital defect causes lower extremity cyanosis?
|
PDA due to it causing a L-->R shunt AFTER the upper main branches of the aorta.
|
|
|
|
What keeps PDA open?
|
Prostoglandins KEEP the PDA open, while indomethacin, a PGE inhibitor closes it.
PGE KEEEEPS the PDA open |
|
|
|
Tetralogy of Falot
|
1.) Pulmonary Stenosis
2.) Right Ventricular Hypertrophy 3.) VSD 4.) Overriding Aorta |
|
|
|
Boot shaped heart on x-ray?
|
Right ventricular hypertrophy, associated with Tetralogy of Falot
|
|
|
|
What condition is associated with squatting after a cyanotic spell? Why does this help?
|
Tetralogy of Falot. It increases systemic resistance, decreasing the pressure differential between
|
|
|
|
Transposition of great vessels A/w
|
Maternal Diabetes
|
|
|
|
What clinical presentation occurs with persistent Truncus Arteriosus?
|
Early cyanosis
5 T's of early cyanosis? |
Truncus Arteriosus
Tetralogy of Falot Transposition of Great Vessels Tricuspid Atresia Total Anomalous Pulmonary Venous Return |
|
|
Infantile Coarctation of the Aorta A/w?
|
In infantile form, it is associated with a PDA and Turner's Syndrome.
Notably, this shunt will be R-->L since the narrowing creates a relative low pressure locally distal to coarctation. This contrasts a normal PDA which is a L-->R shunt. As such, infants will develop cyanosis of the lower extremities. |
|
|
|
Infant with cyanosis of lower extremities
|
Coarctation of the Aorta with associated PDA. PDA is distal to coarctation.
|
|
|
|
Adult Coarctation of the Aorta A/w what clincal sign?
|

"notching" of ribs on x-ray due to engorged arteries. Also associated with what cardiac abnormality?
In the adult form, it will present as hypertension of the upper extremities and hypotension/weak pulses of the lower extremities. |
bicuspid aortic valve.
|
|
|
Etiology of Acute Rheumatic Fever
|
Group A Strep(Strep Pyogenes)
A result of antigenic mimicry due to the virulence factor--M protein. Onset usually 2-3 weeks after strep throat infection |
|
|
|
Diagnosis of acute rheumatic fever?
|
JONES criteria
J -- Joints(migratory polyarthritis) O -- Pancarditis N -- Nodules(subcutaneous) E -- Erythema Marginatum S -- Sydenham's Chorea Main problem is the pancarditis as other symptoms are self-limited |
|
|
|
Swelling and pain in the wrist that resolves in two days. Then some pain in the ankle that resolves and moves to the knees.
|
Migratory polyarthritis A/w Acute rheumatic fever
|
|
|
|
Describe the pancarditis A/w acute rheumatic fever...
|
Endocarditis -- Generally involves vegetations on Mitral Valve. But can also involve Aortic valve. CAN CAUSE REGURGITATION.
Myocarditis -- Aschoff bodies containing Anitschkow cells(caterpillar nuclei in activated histiocytes). Pericarditis -- Leads to friction rub and chest pain |
|
|
|
Most common cause of death during acute phase of acute rheumatic fever
|
myocarditis --
characteristic histologic finding? |
Anitschkow cells in Aschoff bodies characteristic
|
|
|
"fish mouth" appearance of cardiac valve
|
due to stenosis. A/w chronic rheumatic heart disease as a result of repeat Group A strep infections.
|
|
|
|
How does the mitral valve respond in chronic rheumatic heart disease?
|
thickening of the chordae tendineae and cusps
|
|
|
|
How does the aortic valve respond in chronic rheumatic heart disease?
|
leads to fusion of the commissures
|
|
|
|
Aortic Stenosis etiology...
A/w? |
due to wear and tear on valves. As such, presents late in life(>60 years)
A/w bicuspid aortic valve(2 leaves doing the work of 3) |
|
|
|
How can you distinguish stenosis of valves via rheumatic fever vs wear and tear?
|
Rheumatic fever stenosis will always involve mitral valve. Therefore if only aortic valve involved, it must be "wear and tear" etiology.
Also, aortic valve in rheumatic fever will have FUSION of the commissures, whereas in wear and tear, they will just have fibrotic scarring on the surface of the valve. |
|
|
|
Describe clinical course of aortic stenosis...
|
Long asymptomatic period due to compensation period during which a systolic ejection click is followed by a crescendo-decrescendo murmur is heard.
---This leads to ventricular hypertrophy which can progress to cardiac failure. ---Angina and syncope due to the limited ability to increase blood flow across stenotic valve. ---Microangiopathic hemolytic anemia due to RBC's being damages while crossing the calcified valve. |
|
|
|
What causes aortic valve regurgitation?
|
Aortic root dilation, Syphilitic Aneurysm(tertiary syphilis) which pulls apart the valve leaflets
or infectious endocarditis, causing direct damage to the valve |
|
|
|
Clinical features of aortic regurg...
|
Early, blowing diastolic murmur
diastolic because regurg happens during diastole blowing because that's the sound that usually happens on blood flowing backwards. |
|
|
|
When does the pulse pressure widen? Why?
|
The pulse pressure widens because the regurgitating blood increases systolic BP by increasing stroke volume and decreasing diastolic BP by taking away blood from the systemic circulation.
|
|
|
|
head bobbing
|
aortic regurgitation
also a/w bounding pulses and pulsating nail bed. All this is called "hyperdynamic circulation" |
|
|
|
eccentric hypertrophy
|
refers to asymmetric hypertrophy of left ventricle generally due to volume overload.
seen in ? |
aortic regurgitation.
|
|
|
Mitral valve prolapse has a light association with...
|
Marfan syndrome and Ehler-Danlos syndrome
|
|
|
|
heart sound of mitral valve prolapse
|
incidental mid-systolic click followed by a regurgitation murmur.
mid-systolic click is due to the reverse ballooning of mitral valve during contraction of ventricle since the valve is so floppy.(it parachutes out...) |
|
|
|
Etiology of mitral valve regurg...
|
Mitral valve prolapse, left ventricular dilation, rheumatic heart disease and papillary muscle rupture after MI.
|
|
|
|
heart sound with mitral valve regurg...
|
holocystolic blowing murmur louder with squatting and expiration
expiration increases blood flow to atrium and ventricles and as such has more blood to regurg. |
|
|
|
Acute rheumatic fever influence on mitral valve
|
Mitral valve regurgitation
|
|
|
|
Chronic rheumatic fever influence on mitral valve
|
Mitral valve stenosis
|
|
|
|
heart sounds for mitral valve stenosis
|
opening snap followed by a diastolic rumble
|
|
|
|
Staph aureus in endocarditis
|
acute endocarditis
infects tricuspid valve due to high virulence. Common in IV drug abusers |
|
|
|
Strep viridens
|
subacute endocarditis
damaged endocardial surface develops thrombotic vegetations that can trap transient bacteria in blood stream |
|
|
|
endocarditis that is indicative of strep bovis. What do you look for?
|
colorectal carcinoma
|
|
|
|
What kind of organism is strep bovis?
|
Its a group D streptococci. Gram + gamma hemolytic. bile+salt culture?
|
It will NOT grow on it
the enterococci will. |
|
|
HACEK organisms and relevance
|
Haemophilus, Actinobacillus, Cardiobacterium, Eikenella, Kingella
Endocarditis with negative blood cultures. These organisms are particularly difficult to grow. |
|
|
|
Bacterial Endocarditis presenting symptoms...
|
FROM JANE
F - Fever R - Roth's Spots(round white spots on retina surrounded by hemorrhage) O - Osler's nodes(painful on finger/toe pads) M - Murmur(due to vegetative growths on valve) J - Janeway lesions(painless lesions on palms/soles) A - Anemia of Chronic Disease(microcytic) N - Nail-bed hemorrhage E - Emboli(Rt-PE, Lt-Stroke) |
|
|
|
Bacterial endocarditis will cause what specific acute phase reactant?
|
Liver releases Hepcidin, which traps iron in the storage sites which raises ferritin levels which reduces total iron binding capacity. Since no access to iron from storage sites, bone marrow will pull iron from blood, causing low serum iron and percent saturation of iron to decrease.
|
|
|
|
Libman-Sacks endocarditis
|

Lupus associated sterile vegetations that form on BOTH sides of mitral valve
|
|
|
|
Dilated Cardiomyopathy etiology
|
commonly idiopathic,
but can be a late complication related to? |
Coxsackie A or B virus
|
|
|
Hypertrophic Cardiomyopathy etiology
|
Usually due to genetic mutations in sarcomere proteins;
genetics? |
autosomal dominant
|
|
|
Dilated cardiomyopathy symptoms
|
Systolic dysfuntion(ventricle cannot pump) causing biventricular CHF. Mitral and Tricuspid Regurgitation due to stretching of the walls.
|
|
|
|
Symptoms of hypertroph cardiomyopathy
|
Decreased cardiac output - left ventricular hypertrophy is so massive that it cannot fill.
Syncope with exercise -- subaortic hypertrophy of the ventricular septum results in functional aortic stenosis |
|
|
|
Sudden death in young athletes
|
hypertrophic cardiomyopathy
|
|
|
|
Histologic appearance of hypertrophic cardiomyopathy
|
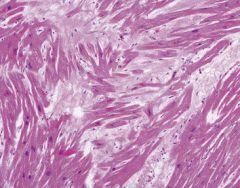
Myofiber disarray with hypertrophy. The muscle fibers are going every which way.
|
|
|
|
rare cause of restrictive cardiomyopathy in children
|
endocardial fibroelastosis
|
|
|
|
Classic finding for restrictive cardiomyopathy; ekg?
|
same as congestive heart failure for the most part.
low voltage EKG, dim qrs amplitudes |
Low voltage EKG with diminished QRS amplitude
|
|
|
Loeffler Syndrome
|
A restrictive cardiomyopathy caused by an endomyocardial fibrosis with an eosinophilic infiltrate and eosinophilia
|
|
|
|
Most common primary cardiac tumor in adults
|
Myxoma. Derives from?
|
MESENCHYME
|
|
|
Clinical presentation of myxoma
|
pedunculated mass in the left atrium that causes syncope due to obstruction of the mitral valve
|
|
|
|
Most common primary tumor in children? A/w?
|
Rhabdomyoma
A/w tuberous sclerosis usually arises in? |
in ventricle
|
|
|
anti-dnase B
|
same as ASO, Group A strep, Rheumatic Fever
|
|

