![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
107 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Bilateral renal agenesis
|
oligohydramnios, flat face with low set ears, developmental defects of extremities. Incompatible with life
|
|
|
|
Dysplastic Kidney genetics and overview
|
NOT INHERITED. Congenital malformation of the renal parenchyma characterized by cysts and abnormal tissue. Usually unilateral, but can be bilateral.
NOTE THE ABNORMAL TISSUE(like cartilage) that can help distinguish against polycystic kidney disease. |
|
|
|
Polycystic Kidney Disease genetics
|
INHERITED leading to BILATERAL enlarged kidneys with cysts in renal cortex and medulla.
recessive and dominant form |
|
|
|
baby with signs of portal hypertension
|
autosomal recessive polycystic kidney disease
|
|
|
|
Juvenile PKD clinical presentation
|
recessive(juvenile) -- worsening renal failure and hypertension. Can present with Potter Sequence.
|
|
|
|
Adult PKD Clinical presentation
|
dominant(adult) -- presents in young adults as hypertension(increased renin), hematuria, and worsening renal failure.
|
|
|
|
Juvenile PKD a/w
|
Recessive form a/w congenital hepatic fibrosis(portal hypertension) and hepatic cysts.
|
|
|
|
Adult PKD a/w
|
A/w berry aneurysm, hepatic cysts and mitral valve prolapse.
BERRY ANEURYSM associated with mortality in Adult PKD |
|
|
|
family history of renal disease with death due to cerebral hemorrhage
|
cysts in the liver cysts in the brain cysts in the kidney
think of Adult PKD |
|
|
|
Medullary Cystic Kidney Disease
|
Autosomal Dominant defect leading to cysts in the MEDULLARY collecting ducts. Notably these kidneys are SHRUNKEN, as opposed to enlarged in PKD.
|
|
|
|
Azotemia
|
increase in BUN/Creatinine in blood
|
|
|
|
Prerenal Azotemia common cause?
|
commonly due to decreased blood flow to kidneys(e.g. cardiac failure)
decreased blood flow results in decreased GFR, azotemia and oliguria. |
|
|
|
Prerenal Azotemia leads to what lab finding?(BUN:Cr), etc.
|
Reabsorption of fluid and BUN ensues in response to release of Aldosterone causing serum BUN:Cr ratio to be >15.
Fractional Excretion of sodium [FENa]<1%(normal) and urine osmolality is >500(normal, meaning you can still concentrate urine). |
|
|
|
Postrenal Azotemia
|
Obstruction of ureters causing backpressure in glomerulus which decreases GFR.(decrease GFR means azotemia and oliguria)
|
|
|
|
Postrenal Azotemia leads to what lab finding in short term? in long term?(BUN:Cr), etc.
|
Acute
The backpressure pushes BUN out of the tubule increasing the BUN:Cr ratio to >15. Fractional Excretion of sodium [FENa]<1%(normal) and urine osmolality is >500(normal, meaning you can still concentrate urine). Long-term Decreased resorbtion of BUN because resorbtion requires epithelium to be intact. Damage to the epithelium causes reduction in the BUN:Cr ratio. Due to that damage, you also cause the FENa to elevate(>2%) and are unable to properly concentrate urine(<500 mOsm/kg) |
|
|
|
Acute Tubular Necrosis
|
injury and necrosis of tubular epithelial cells
necrotic cells plug tubules, decreasing GFR. These brown, granular casts are seen in the urine. labs are similar to long term postrenal azotemia. |
|
|
|
Which parts of kidney most susceptible to ischemic damage? nephrotoxic damage?
|
ischemic - Proximal tubule and medullary segment of the thick ascending limb
nephrotoxic - proximal tubule |
|
|
|
What can prerenal azotemia progress to?
|
Acute Tubular Necrosis of the ischemic kind
|
|
|
|
Most common cause of nephrotoxic acute tubular necrosis?
|
Aminoglycosides.
Also caused by myoglobinuria, ethylene glycol, heavy metals(lead), radiocontrast dye, and urate(tumor lysis syndrome) |
|
|
|
What is drinking ethylene glycol associated with?
|
oxalate crystals in urine
|
|
|
|
Tumor Lysis Syndrome
|
Chemotherapy can cause massive destruction of cells leading the creation of uric acid which can be toxic to the kidneys leading to Acute Tubular Necrosis.
You can try to prevent this with hydration and allopurinol. |
|
|
|
Clinical features of Acute Tubular Necrosis
|
1.) Brown casts in urine.
2.) Elevated BUN/Creatinine 3.) Hyperkalemia and metabolic acidosis(inability to excrete K+ and organic acids) |
|
|
|
Commons causes of Acute Interstitial Nephritis
|
NSAIDS, penicillin and diuretics
Drug-induced Hypersensitivity reaction of the interstitium. |
|
|
|
Classic findings in Acute Interstitial Nephritis
|
oliguria, fever and rash days to weeks after starting drug
NOTABLY, eosinophils found in urine |
|
|
|
Causes of Renal papillary necrosis
|
Chronic analgesic abuse
Diabetes mellitus Sickle cell trait/disease Severe Acute Pyelonephritis |
|
|
|
Nephrotic Syndrome characterized by...
|
Hypoalbuminemia -- pitting edema
Hypogammaglobulinemia -- increased risk of infection Hypercoagualable state -- preferential loss of Anti-Thrombin III Hyperlipidemia and Hypercholesterolemia -- liver reacts to loss of protein in blood by throwing **** in it to thicken it up. May result in fatty casts in urine. |
|
|
|
Minimal Change Disease a/w
|
Hodgkin's Lymphoma -- massive overproduction of cytokines by Reid-Sternberg cells
EXCELLENT response to steroid therapy. This is because effacement of foot processes is caused by production of cytokines. |
|
|
|
Minimal Change demographic
|
most common nephrotic syndrome in children
|
|
|
|
Minimal Change Disease hallmark?
|
Loss of podocyte(foot processes) on EM. Other than that, you see normal glomeruli on H&E and negative immunofluorescence(MC not driven by immune complex deposition).
|
|
|
|
Minimal Change disease clinical signs?
|
Selective proteinuria(loss of albumin, but not Ig)
|
|
|
|
Focal Segmental Glomerulosclerosis demographic
|
Hispanics and African Americans.
Also a/w HIV, heroin use and sickle cell disease |
|
|
|
Focal Segmental Glomerulosclerosis clinical stuff?
|
effacement of the foot processes on EM. Exact same as Minimal Change. Nothing on H&E, Nothing on IF.
Someone with Minimal Change who doesn't respond to steroids basically progresses to FSGS. |
|
|
|
Membranous Nephropathy demographic
|
Caucasian adults
a/w Hepatitis B or C, solid tumors, SLE, or drugs. Most common kidney disease in SLE? |
Diffuse Proliferative Glomerulonephritis.(kind of both nephritic and nephrotic...)
BUT if its a nephrotic syndrome, THEN they will have Membranous Nephropathy |
|
|
Most common cause of death in lupus is?
|
Renal disease. BUT most common renal disease is nephritic syndrome(diffuse proliferative membranous nephritis). However, if they develop a nephrotic syndrome, then they get Membranous Nephropathy
|
|
|
|
Membranous Nephropathy
|
Thick glomerular basement membrane on H&E, due to immune complex deposition.
Immune complexes deposit SUBEPITHELIALLY. They have a granular immunofluorescence and a ________ appearance on EM. This is because epithelial cells lay down basement membrane when they get pushed off by immune complexes. |
'spike and dome'
|
|
|
Membranoproliferative Glomerulonephritis Type 1
|
Subendothelial and a/w?
|
Hep B and C
|
|
|
"tram-track" appearance
|
membranoproliferative glomerulonephritis
|
|
|
|
Membranoproliferative Glomerulonephritis Type 2
|
intramembranous; a/w C3 nephritic facotr(autoantibody that stabilizes C3 convertase, leading to overactivation of complement, inflammation and low levels of circulatin C3)
|
|
|
|
membranoproliferative glomerulonephritis
|
Thick glomerular basement membrane on H&E due to immune complex deposition
|
|
|
|
Key problem is effacement of foot processes
|
Minimal Change Disease
Focal Segmental Glomerulosclerosis |
|
|
|
Key problem is immune deposition
|
Membranous Nephropathy
Membranoproliferative Glomerulonephritis |
|
|
|
Diabetes Mellitus effect on kidneys
|
Non-enzymatic Glycosylation of vascular basement membrane causing leakiness letting protein leak into the wall and causing hyaline arteriolosclerosis which causes thickening of the vessel wall(decreasing lumen caliber). This happens preferentially at the efferent arteriole causing increased pressure at the glomerulus leading to sclerosis of the mesangium of the glomerulus. ACE inhibits can slow this by dilating the efferent arteriole a bit.
|
|
|
|
First change that occurs in kidney in a diabetic
|
Non enzymatic glycosylation of vascular basement membrane
|
|
|
|
microalbuminuria
|
sclerosis of the mesangium resulting from hyperfiltration. Will cause Kimmelstiel-Wilson nodules(pathognomonic for diabetes)
|
|
|
|
Kimmelstiel-Wilson nodule, pathognomonic for diabetes
|
|
|
|
Systemic Amyloidosis
|
Kidney is the most commonly involved organ in amyloidosis.
|
|
|
|
Where does amyloid deposit in Amyloidosis?
|
Mesangium, resulting in ?
|
nephrotic syndrome
|
|
|
What stains amyloid? How does it stain?
|
Apple green birefringence under polarized light after staining with Congo Red
|
|
|
|
Nephritic Syndrome
|
Hallmark is glomerular inflammation and bleeding
1.) LIMITED proteinuria 2.) Oliguria and Azotemia 3.) Salt retention -- periorbital edema and hypertension(salt/fluid retention) 4.) RBC casts and dysmorphic RBCs in urine -- Immune Complex deposition activated Complement; C5a attracts neutrophils which mediate the damage |
|
|
|
Post Streptococcal Glomerulonephritis etiology
|
Nephritic Syndrome that arises after a Group A strep infection.(M protein virulence causes **** to go down)
|
|
|
|
Clinical symptoms of PSGN
|
hematuria(cola colored urine), oliguria, HTN, and periorbital edema
|
|
|
|
Hallmark of PSGN
|
subepithelial hump on EM.
Immune complexes start sub-endothelially, but they move up into the subepithelial space. Will eventually pop off and dissipate. |
|
|
|
Rapidly Progressive Glomerulonephritis
|
Nephritic syndrome that progresses to renal failure in weeks to months.
|
|
|
|
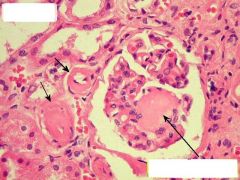
Crescent's in Bowman's space
|
Presents in Rapidly Progressing Glomerulonephritis
Crescent is composed of Fibrin and macrophages. |
|
|
|
Antibody against collagen in glomerular and alveolar basement membranes
|
Goodpasture Syndrome
linear immunofluorescence; presents as hematuria and hemoptysis, classically in young adult males |
|
|
|
Most common renal disease in SLE. Where do the immune complexes deposit?
|
Diffuse proliferative Glomerulonephritis. Subendothelial deposition.
|
|
|
|
What pattern of immunofluorescence does PSGN present with?
|
Granular
|
|
|
|
Negative IF(pauci-immune) diseases
|
Wegener Granulomatosis, Microscopic Polyangiitis, and Churg-Strauss Syndrome
Wegeners - c-ANCA, nasopharyngeal involvement, lungs and kidney Microscopic Polyangiitis & Churg-strauss both p-ANCA, but Churg-Strauss will have granulomatous inflammation, eosinophilia and asthma. |
|
|
|
Most common nephropathy?
|
IgA nephropathy, IgA deposition in mesangium. Follow mucosal infection.
|
|
|
|
Alport Syndrome
|
X-linked defect in Type IV collagen.
Results in thinning/splitting of basement membrane. Clinical symptoms are: Isolated hematuria, sensory hearing loss and ocular disturbances. |
|
|
|
What symptoms present with cystitis?
|
Dysuria, increased frequency of urination, urgency, suprapubic pain with systemic signs being absent.
|
|
|
|
Lab findings with cystitis?
|
Greater than 100,000 colony forming units
Positive leukocyte esterase and nitrites(bacteria convert nitrates to nitrites) Cloudy urine with >10 WBCs/hpf |
|
|
|
Alkaline urine with ammonia scent
|
Proteus mirabalis
|
|
|
|
What would make you suspect Neisseria or chlamydia for a UTI?
|
Sterile pyuria. Negative urine culture with pyuria.
|
|
|
|
What is usually the cause of pyelonephritis?
|
Ascending infection.
A/w vesicoureteral reflux. |
|
|
|
flank pain. other presentations?
|
pyelonephritis
will also have WBC casts and fever. This contrasts the RBC casts with nephritic syndrome. |
|
|
|
Most common pathogens for pyelonephritis?
|
E. Coli
Klebsiella Enterococcus faecalis |
|
|
|
What causes chronic pyelonephritis?
|
In children, vesiculoureteral reflux or obstruction due to BPH or cancer in adults.
|
|
|
|
Gross exam with chronic pyelonephritis in children?
|
vesiculoureteral reflux will frequently scar the upper and lower portions of the kidney
|
|
|
|
'thyroidization' of the kidney
|
chronic pyelonephritis
|
|
|
|
Most common type of stone? Most common cause? A/w?
|
Calcium oxalate and/or calcium phosphate. Must exclude hypercalcemia, but most common cause is idiopathic hypercalciuria.
A/w what disease? |
Crohn's Disease -- this is because the increased absorption of oxalate binds calcium
|
|
|
What would you treat calcium oxalate/phosphate stone with?
|
Hydrochlorothiazide. Ca+2 sparing diuretic reduces the calcium in urine
|
|
|
|
"staghorn calculi" in adult
|
Usually Ammonium Magnesium Phosphate,
in kid? |
but can also be Cysteine(especially if its a kid).
|
|
|
Most common organisms causing Ammonium magnesium phosphate stones
|
Proteus or Klebsiella. Alkalize urine predisposing stone formation
|
|
|
|
Radiolucent stone? Risk factors?
|
Uric acid
hot, arid climates, low urine volume and acidic pH. Most common stone seen in patients with Gout. hyperuricemia(leukemia or myeloproliferative disorder, lots of cell turnover) |
|
|
|
A stone commonly seen in children? a/w?
|
Cysteine stone
Genetic Cysteinuria due to decrease resorption |
|
|
|
Most common causes of Chronic Renal Failure
|
Diabetes Mellitus, Hypertension and Glomerular Disease
|
|
|
|
Where is EPO secreted from in kidneys?
|
Renal peritubular Interstitial cells
|
|
|
|
shrunken kidney's with cysts
|
dialysis of a chronic renal failure patient
increases risk for? |
renal cell carcinoma
|
|
|
Angiomyolipoma a/w
|
Tuberous Sclerosis
|
|
|
|
Triad of Renal Cell Carcinoma
|
hematuria, palpable mass and flank pain
|
|
|
|
Renal Cell Carcinoma symptoms
|
MULTIPLE paraneoplastic syndromes(EPO, renin, PTHrP, ACTH, etc.)
Left sided varicocoele due to anatomy of left testicular vein draining into left renal vein |
|
|
|
"clear cytoplasm"
|
Renal Cell Carcinoma subtype or "clear cell carcinoma"
|
|
|
|
Genetics of Renal Cell carcinoma
|
loss of VHL tumor supressor which leads to increased IGF-1(promotes growth) and increased HIF(increased VEGF and PDGF)
2 pathways, sporadic and hereditary -- both involve same mutation |
|
|
|
Sporadic Renal Cell Carcinoma presents where usually? demographic, and risk factor?
|
adult males over 60 as a single tumor in the upper pole of the kidney.
A/w Cigarette Smoke |
|
|
|
Hereditary Renal Cell Carcinoma
|
generally in younger patients with multiple and bilateral tumors.
A/w Von-Hippel-Lindau disease. These patients are also at risk for hemangioblastoma of the cerebellum. |
|
|
|
Von-Hippel-Lindau
|
Hemangioblastoma of the cerebellum and hereditary renal cell carcinoma
|
|
|
|
Most common tumor in the kidney arising in children
|
Wilm's Tumor comprised of blastema(immature kidney mesenchyme).
|
|
|
|
Presentation of Wilm Tumor?
|
Large unilteral flank mass with hematuria and HTN(renin secretion)
|
|
|
|
Genetics of Wilm's Tumor. Symptoms?
|
WT1 mutation
WAGR Wilm's Tumor Aniridia Genetial Abnormalities Mental/motor retardation |
|
|
|
Beckwith-Wiedemann syndrome
|
Wilm's tumor AND neonatal hypoglycemia, muscular hemihypertrophy and organomegaly(including tongue)
|
|
|
|
#1 risk factor for urothelial carcinoma
|
Polycyclic aromatic hydrocarbons from cigarette smoke
|
|
|
|
Painless hematuria
|
urothelial carcinoma
|
|
|
|
urothelial carcinoma pathways
|
flat pathway -- goes straight from high grade to invasive and is associated with an early p53 mutation
papillary pathway -- goes from low to high grade and then to invasive cancer and is not associated with early p53 mutation |
|
|
|
Microbe associated with Squamous Cell Carcinoma
|
Schistosoma Hematobium
|
|
|
|
Squamous Cell Carcinoma in lower urinary tract demographic
|
Middle Eastern male -- Schistosoma causes chronic inflamation
Squamous cell must be from metaplasia-->dysplasia-->carcinoma pathway. |
|
|
|
Adenocarcinoma a/w?
|
Adenocarcinoma that develops from a urachal remnant will develop at the dome of the bladder
Bladder Exstrophy |
|
|
|
What do newborns with PKD present with?
|
Potter sequence
a/w? |
Congenital hepatic fibrosis, hepatic cysts
|
|
|
baby with signs/symptoms of portal HTN
|
AR PKD
|
|
|
|
Mitral valve prolapse is a/w?
|
Marfan's, Ehler-Danlos, but ALSO ADPKD
|
|
|
|
shrunken kidneys with worsening renal failure
|
Medullary Cystic Kidney Disease -- cysts in medullary collecting ducts
What is the inheritanc? |
Autosomal Dominant
|
|
|
Beta 1 receptors are where other than the heart?
|
JG cells of the kidney. Stimulation causes renin secretion
|
|
|
|
Explain the diagnostic finding in prerenal azotemia
|
BUN:Creatinine > 15
BUN is filtered freely and then reabsorbed. Creatinine is NOT reabsorbed. In prerenal azotemia, RPF decreases which stimulates Renin secretion causing volume retention. Volume retention drags BUN along with it causing an increase in the BUN: Creatinine ratio. |
|
|
|
brown granular casts in urine
|
Acute Tubular Necrosis(the brown casts are necrosed cells)
What is significant about ATN? |
Most common cause of Acute Renal Failure
|
|
|
Describe BUN:Creatinine in Postrenal Azotemia
|
The hallmark in the beginning is simply blockage. The blockage "pushes" BUN back out into serum.
In the late stages, you get necrosis of tubular cells that result in a loss of BUN reabsorption effectively decreasing the BUN:Creatinine ratio. In addition, the necrosed cells cause a blockage in the tubule. What other lab findings will be present? |
FENa > 2% (should be less than 1% in normal)
Inability to concentrate urine(Urine Osm < 500) |
|
|
What agents are used to prevent ATN prior to chemotherapy?
|
Allopurinol and Hydration
(Tumor lysis syndrome increases uric acid) |
|
|
|
What kind of crystals form following ethylene glycol exposure?
|
Oxalate Acid Crystals
|
|

