![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
67 Cards in this Set
- Front
- Back
|
Acute pancreatitis
|
Premature activation of trypsin activate other enzymes leading to autodigestion of pancreatic parenchyma.
Causes both liquefactive(pancreatic parenchyma) and fat necrosis(peripancreatic fat) |
|
|
Most common cause of pancreatitis
|
Alcohol and gallstones
Rupture of a posterior duodenal ulcer Mumps virus |
|
|
Lab findings for pancreatitis(acute)
|
lipase and amylase.
lipase more specific Hypocalcemia due to fat necrosis |
|
|
Complications of acute pancreatitis
|
Shock due to peripancreatic hemorrhage
Pancreatic PSEUDOcyst - just lined by fibrous tissue surrounding the liquefactive necrosis and enzymes.(Causes persistent elevation of amylase) DIC and ARDS(enzymes can activate coagulation, can also destroy lung tissue if they get into blood) |
|
|
Common cause of pancreatic abscess? presentation?
|
E. coli; presents with abdominal pain, fever and persistently elevated amylase(normally would reduce after bout of acute pancreatitis)
|
|
|
Common causes of chronic pancreatitis
|
Alcohol(adults) and cystic fibrosis(children). Can also be idiopathic.
CF - slows the ability of the pancreas to drain |
|
|
Clinical features of chronic pancreatitis
|
--Epigastric abdominal pain that radiates to the back.
--Pancreatic Insufficiency leading to fat malabsorption, steatorrhea, poor absorption of Vitamins DAKE --ABSENCE of amylase/lipase in chronic pancreatitis --dystrophic calcification of pancreas --damage to islets leading to secondary Diabetes Type II --Risk for pancreatic carcinoma |
|
|
Pancreatic Carcinoma demographic and risk factors
|
elderly(>70)
Smokers and chronic pancreatitis |
|

Clinical features of pancreatic cancer(head)
|
--Tumor in the head of pancreas blocks the flow of bile which allows whatevers in bile to leak into blood. As such, conjugated bilirubin leaks into blood(jaundice).
--Since bile can't get to GI tract, you get pale stool. --Since duct is blocked, bile swells up making it palpable. obstructive jaundice, pale stool, palpable bladder |
|
|
Clinical features of pancreatic cancer(tail)
|
Secondary diabetes if they knock out islet cells.
|
|
|
Serum tumor marker for pancreatic cancer?
|
CA 19-9
|
|
|
Classic sign for pancreatic cancer?
|
Trousseau sign -- presents as swelling erythema and tenderness in the extremities
|
|
|
Biliary obstruction within first 3 months of life?
|
Biliary atresia
|
|
|
Biliary atresia presentation
|
Presents within first 3 months, CONJUGATED bilirubin can leak into blood causing jaundice and can lead to cirrhosis due to back pressure to the liver
|
|
|
Cholelithiasis(Gallstones)
|
Precipitation of cholesterol or bilirubin in bile(both components of bile)
Can occur due to supersaturation OR decreased phospholipids/bile acids which help solubilize cholesterol. OR stasis which can lead to infection where bacteria can unconjuage bilirubin causing stones |
|
|
Cholestyramine
|
lipid lowering agent which binds bile acids which prevents ileum from recycling bile acids. Thus decreased bile acids increase risk of cholesterol stones
|
|
|
Cholesterol Stones description/risk factors
|
usually radioLUCENT, YELLOW stones
Age(40ish), estrogen-- which increase activity of HMG-CoA reductase which increases cholesterol and increase Lipoprotein receptors on hepatocytes increasing cholesterol uptake(female, obese) --clofibrate(lipid lowering agent increasing HMG-Coa reductase activity causing increased cholesterol and decreases conversion of cholesterol to bile acids which decreases solubility --Crohn's Disease(terminal ileum) which damages ability to reuptake bile salts/acids which is necessary for solubility in bile --Cirrhosis leads to decreased production of bile salts |
|
|
Bilirubin Stone description/risk factors
|
RadioOPAQUE, BLACK in color
Risk factors: --Extravascular Hemolysis(increases bilirubin in bile.) Hb --> Heme and Globin Heme --> Iron and Protoporphyrin Protophorphyrin --> Unconjugated Bilirubin This bilirubin is eventually put in gall bladder, so if theres a lot of extravascular hemolysis, there's a lot of conjugated bilirubin in the gall bladder when the liver eventually works through it. -- Biliary tract infection(bacteria can deconjugate increasing risk of precipitation) |
|
|
Complications associated with gallstones
|
Biliary colic, acute/chronic cholecystitis, ascending cholangitis, gallstone ileus and gallbladder cancer
|
|
|
Biliary colic presents where?
|
Right upper quadrant pane
Waxing and waning pain as gall bladder contracts against stone |
|
|
Acute Cholecystitis Etiology
|
A stone blocking duct will cause dilatation of gall bladder leading to pressure ischemia and bacterial overgrowth of E.Coli
|
|
|
Right upper quadrant pain radiating to the right scapula
|
Acute cholecystitis
|
|
|
Acute cholecystitis lab findings
|
increased serum alk phosp, increased WBC
|
|
|
What key sign is associated with Chronic Cholecystitis
|
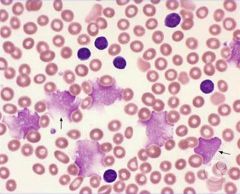
Rokitansky-Aschoff sinus -- herniation of gallbladder mucosa into the muscular wall(PICTURE)
|
|
|
Chronic Cholecystitis long term complication...
|
Porcelain gall bladder
Shrunk hard gallbladder due to chronic inflammation, fibrosis and dystrophic calcification |
|
|
Gallstone ileus etiology
|
fistula formed between gallbladder wall and small bowel allowing a huge ass stone to block GI tract
|
|
|
cholecystitis in an elderly woman(80 year old)
|
Gall bladder carcinoma
|
|
|
What binds unconjugated bilirubin to allow it to travel in blood?
|
Albumin
|
|
|
What enzyme conjugates bilirubin?
|
Uridine Glucuronyl Transferase(UGT) in hepatocytes.
|
|
|
Describe what happens to conjugated bilirubin?
|
It is released in the small bowel to aid in digestion. The intestinal flora then convert conjugated bilirubin into urobilinogen
|
|
|
Extravascular Hemolysis
|
Overpowers livers ability to conjugate, leads to an increase in unconjugated bilirubin in the blood.
EVENTUALLY, this will lead to high concentration bilirubin in bile that enters small bowel. Turns to urobilinogen in GI tract and turns urine and stool dark.(Urine dark due to UROBILINOGEN) |
|
|
Physiologic Jaundice of the Newborn
|
Newborn has transiently low UGT activity. UCB can deposit in brain and lead to neurologic deficits and death(kernicterus). UCB cannot leave in urine because it is not water soluble, but Phototherapy simply makes UCB water soluble.
|
|
|
Gilbert Syndrome
|
mildly low UGT, leading to an increase in UCB
|
|
|
Crigler-Najjar Syndrome
|
Absence of UGT, leads to kernicterus. It is a genetic disorder thats usually fatal.
|
|
|
Pitch dark liver incidental finding
|
Dubin Johnson Syndrome -
Deficiency of bilirubin canalicular TRANSPORT(after it has been conjugated). Not clinically significant, but will have a conjugated bilirubinemia(CB in blood). Can have this deficiency without discoloration(Rotor syndrome) |
|
|
Liver fluke
|
Clonorchis Sinensis
|
|
|
Biliary tract obstruction(obstructive jaundice)
|
anything that blocks bile duct.
--dark urine(water soluble CB in blood gets filtered --DECREASED Urobilinogen --pale stools(CB doesn't get to GI) --Lots of cholesterol in bile leaks into blood leading to hypercholesterolemia with xanthomas --steatorrhea with malabsorption of fat soluble vitamins |
|
|
Viral hepatitis
|
Inflammation disrupts hepatocytes and small bile ducts leading to an increase in increased CB and UCB
Dark urine due to increase CONJUGATED bilirubin. Urine urobilinogen is normal or decreased due to the hepatocyte +bile ductules dysfunction |
|
|
Acute Hepatitis lab tests
|
ALT >> AST
|
|
|
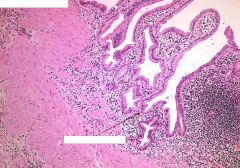
Chronic Hepatitis predominantly involves...?
|
Portal tract
|
|
|
Fecal-oral transmission?
|
Hep A and E
No Chronic state |
|
|
Pregnant women with fulminant hepatitis(liver failure and massive liver necrosis)
|
Hepatitis E
|
|
|
Immunization is available for what heps? What antibody signifies immunity?
|
Hepatitis A, IgG
|
|
|
Commonly acquired by travelers
|
Hep A
|
|
|
Commonly acquired from contaminated water or undercooked seafood
|
Hep E
|
|
|
How is hepatitis B transmitted?
|
parenteral tranmission(childbirth, intercourse, IV drugs)
|
|
|
Hep B Serology
|
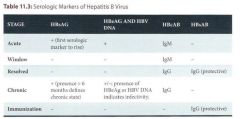
1.) HBsAG is KEY MARKER for infection. First marker that arises during infection. If it stays for longer than 6 months, then you're chronic.
2.) IgM vs core in the beginning. Transition to IgG when you level up. If you WIN then HBsAG goes away. If you don't it stays 3.) IgG vs HBsAB means VICTORY.(or immunization) 4.) HBeAG indicates infectivity. "need an envelope to mail to friend, etc." |
|
|
How is Hepatitis C transmitted?
|
Parenterally.
HCV-RNA test confirms infection. Decreased RNA indicates recovery while persistence indicates disease. |
|
|
What virus more commonly progresses to chronic hepatitis?
|
Hepatitis C OFTEN progresses to chronic disease vs Hep B which rarely progresses.
|
|
|
Which is worse? coinfection or superinfection of Hep D?
|
superinfection
|
|
|
Decreased detox in liver failure can lead to what symptoms?
|
Excess estrogen(gynecomastia, spider angiomata, palmar erythema)
Jaundice, mental status changes |
|
|
What lab test gauges coagulopathy in liver disease?
|
PT - loss of epoxide reductase
|
|
|
Enzyme elevation in Alcoholic hepatitis. Why?
|
AST>>ALT
AST is mitochondrial, and alcohol is a mitochondrial poison |
|
|
What distinctive histologic feature presents in alcoholic hepatitis?
|
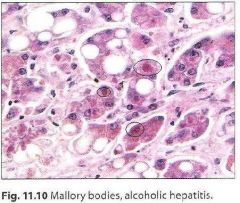
Mallory bodies which are damaged cytokeratin filaments(IMF)
|
|
|
The protein coded for by the gene involved in primary hemochromatosis is most similar to what other protein?
|
Mutations in the HFE gene
Similar to MHC Class I. HFE also associated with Beta 2 microglobulin. Regulates interaction of transferrin receptor with transferrin |
|
|
What is the triad for hemochromatosis?
|
cirrhosis, secondary diabetes mellitus, and bronze skin.
Also find cardac arrhythmias and gonadal dysfunction. |
|
|
What labs do you find with hemochromatosis?
|
Increased ferritin, decreased TIBC, inreased serum Iron and increased Saturation.
|
|
|
What stain, stains for iron?
|
Prussian Blue, will distinguish between iron and lipofuscin which is commonly present in hepatocytes.
|
|
|
Wilson disease
|
Autosomal recessive defect(APT7B) in ATP mediated hepatocyte copper transport. Can't transport copper into bile or ceruloplasmin.
|
|
|
Lab findings in Wilson disease
|
increased urinary copper, decreased serum ceruloplasmin(can't transport copper into this transport protein), and increased copper on liver biopsy.
|
|
|
Primary Biliary Cirrhosis demographic
|
40 yr old women
|
|
|
What classic lab finding do you see in Primary Biliary Cirrhosis?
|
antimitochondrial antibody
|
|
|
Primary Sclerosing Cholangitis
|
Inflammation and fibrosis of intrahepatic and extrahepatic bile ducts that presents with obstructive jaundice
|
|
|
Primary Sclerosing Cholangitis associated with?
|
Ulcerative Colitis(p-ANCA positive)
|
|
|
What one disease do you give aspirin to children for?
|
Kawasaki Disease
|
|
|
What microbe is a risk factor for hepatocellular carcinoma?
|
Aspergillus that releases aflatoxins. These toxins induce p53 mutations.
|
|
|
Serum tumor marker for Hepatocellular Carcinoma?
|
alpha-fetoprotein
|

