![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
184 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
HSV-1 remains dormant where? |
ganglia of trigeminal nerve
|
|
|
|
Triad of genital ulcers, aphthous ulcers and uveitis
|
Behcet syndrome, due to immune complex vasculitis
|
|
|
|
Behcet Syndrome clinical triad
|
Triad of genital ulcers, aphthous ulcers and uveitis, due to immune complex vasculitis
|
|
|
|
Leukoplakia
|
white plaque that can't be scraped away
|
|
|
|
Oral candidiasis
|
a white deposit on the tongue which is EASILY scraped away, usually seen in immunocompromised patients
|
|
|
|
hairy leukoplakia
|
a white rough patch that arises on the LATERAL tongue. Usually seen in immunocompromised and is due to EBV induced squamous cell hyperplasia. NOT pre-malignant.
|
|
|
|
bilateral inflammation of the parotid glands
|
mumps virus
a/w |
Orchitis that can cause STERILITY in teenagers
|
|
|
mobile painless circumscribed mass at the angle of the jaw
|
pleomorphic adenoma. Most common tumor of the salivary gland
What is unique about this? |
It is BIPHASIC -- it consists of both cartilage(stroma) and glands (epithelial tissue)
|
|
|
facial nerve runs through which gland?
|
parotid gland
|
|
|
|
What facial tumor has a high rate of recurrence?
|
Pleomorphic adenoma, due to the irregular margins. An inexperienced surgeon might miss part of it.
|
|
|
|
Esophageal webs a/w
|
Extension of MUCOUS membrane.
Plummer-Vinson syndrome... Severe Iron deficiency anemia, beefy red tongue due to atrophic glossitis and esophageal webs |
|
|
|
Location of Zenker's diverticulum
|
above upper esophageal sphincter at the junction of the esophagus and pharynx.
Above cricopharyngeus muscle |
|
|
|
Mallory Weiss syndrome a/w
|
alcoholics, bulemics, lots of PAINFUL vomiting of blood
|
|
|
|
Mallory Weiss a/w complication
|
Boerhaave syndrome -- rupture of esophagus leading to air in the mediastinum and subcutaneous emphysema
|
|
|
|
Arises secondary to portal hypertension
|
esophageal varices
|
|
|
|
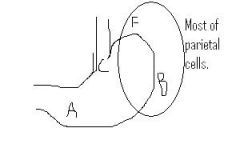
describe path of drainage of esophageal vein
|
esophageal vein --> left gastric vein --> portal vein
into portal vein via the LEFT gastric vein |
|
|
|
PAINLESS hematemesis in chronic alcoholic
|
think torn esophageal varices
|
|
|
|
inability to relax the lower esophageal sphincter
|
achalasia, bird's beak x-ray.
A result of damaged ganglion cells in myenteric plexus Dysphagia for solids AND liquids |
|
|
|
Location of damage in achalasia
|
myenteric plexus, which is between the inner circular and outer longitudinal layers of the muscularis propria.
|
|
|
|
Achalasia a/w
|
Trypanosoma Cruzi infection in Chagas disease
|
|
|
|
Barrett's esophagus metaplasia(BE SPECIFIC)
|
non-keratinized stratified squamous to non-ciliated mucinous columnar
|
|
|
|
Cancers of the esophagus
|
Upper to middle 1/3 is generally squamous cell carcinoma
lower 1/3 is generally adenocarcinoma arising from Barrett's esophagus. |
|
|
|
Progressive dysphagia with hoarseness, cough and weight loss
|
Squamous cell carcinoma of esophagus.
hoarseness indicates recurrent laryngeal nerve involvement |
|
|
|
Lymphatic spread in esophagus
Upper 1/3 |
Cervical nodes
|
|
|
|
Lymphatic spread in esophagus
Middle 1/3 |
mediastinal or tracheobronchial nodes
|
|
|
|
Lymphatic spread in esophagus
Lower 1/3 |
celiac and gastric nodes
|
|
|
|
bubbles underneath skin that crackle and pop when pressed down
|
subcutaneous emphysema
|
|
|
|
painless hematemesis
|
esophageal varices
|
|
|
|
painful hematemesis
|
mallory-weiss syndrome
|
|
|
|
Bowel sounds in lower lung fields
|
paraesophageal hernia
can cause lung hypoplasia due to space invading the pleural cavity |
|
|
|
adult onset asthma
|
think of GERD
|
|
|
|
Exposure of abdominal contents WITHOUT a sac
|
gastrochisis
|
|
|
|
Exposure of abdominal contents WITH a sac
|
omphalocoele
Sac is peritoneum and amnion of umbilical cord |
|
|
|
Olive like mass in abdomen
|
pyloric stenosis
|
|
|
|
Projectile non-bilious vomiting
|
pyloric stenosis
|
|
|
|
mucin producing cells of stomach
|
foveolar cells
|
|
|
|
bicarb secreting cells of stomach
|
surface epithelium
|
|
|
|
Curling ulcer
|
Severe burn leads to acute gastritis due to decreased blood supply secondary to hypovolemia.
Decreased blood supply inhibits ability to carry away excess acid from stomach. |
|
|
|
Prostoglandins
|
decrease acidity, increase ability of cell to produce mucus and bicarb, and increase blood flow
THEREFORE NSAIDS will increase acidity by destroying COX which produces PGE's. |
|
|
|
Cushing ulcer
|
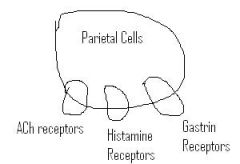
increased stimulation of vagus nerve secondary to increased ICP leads to increased acid production
increased vagus stim causes increase of ACh which binds parietal cells and increases acid production |
|
|
|
Chronic autoimmune gastritis etiology
|
autoimmune destruction of gastric parietal cells located in body and fundus of stomach by T-cells. Antibodies against parietal cells or intrinsic factor are created as a side effect.
Antibodies are SIDE EFFECT of damage, not CAUSING the damage. Damage is T-CELL mediated. |
|
|
|
Chronic autommune gastritis hypersensitivity
|
Type IV - mediated by T-cells.
Antibodies created as a consequence of damage |
|
|
|
Chronic autoimmune gastritis clinical symptoms
|
Achlorhydria(low acid production due to autoimmune destruction of parietal cells) with increased gastrin levels and antral G-cell hyperplasia. Megaloblastic(pernicious) anemia due to loss of intrinsic factor(made by parietal cells).
|
|
|
|
Most common form of gastritis
|
H. Pylori associated chronic gastritis
|
|
|
|
Most common site of infection of h.pylori
|
antrum of stomach
|
|
|
|
Layers of stomach muscle
|
THREE layers rather than the normal two
1.) inner oblique layer 2.) middle circular layer 3.) outer longitudinal |
|
|
|
Aurbach's plexus
|
AKA myenteric plexus, always BETWEEN inner circular and outer longitudinal
|
|
|
|
Meissner's Plexus
|
between the submucosa and the inner circular muscle.
|
|
|
|
presents 2 weeks after birth
|
pyloric stenosis
|
|
|
|
What prophylactic treatment might you put someone in shock on?
|
PPI's to prevent multiple stress ulcers.
|
|
|
|
Chronic Autoimmune gastritis affects mostly which part of stomach?
|
Body and fundus
|
|
|
|
Gastric Adenocarcinoma risk factors
|
Autoimmune Chronic Gastritis(chronic inflammation) causes intestinal metaplasia.
Peyer's patches have a bunch of lymphocytes in it, that's their normal function. As such, when the stomach sees a bunch of lymphocytes due to chronic inflammation, it will change to try to accommodate that crap. |
|
|
|
Foveolar cells secrete mucus but do not look like goblet cells. What do goblet cells in the stomach indicate?
|
Gastric adenocarcinoma
|
|
|
|
Involves predominantly the antrum of the stomach?
|
H. Pylori chronic gastritis
Contrast with autoimmune chronic gastritis which presents in the...? |
|
|
|
Describe histology of h.pylori infection
|
H.pylori sit on top of the epithelium(they do NOT invade). They secrete ureases and proteases that degrade the mucosal membrane though.
|
|
|
|
Duodenal Ulcer etiology
|
Etiology is almost always h.pylori but can also be due to Zollinger-Ellison tumor.
|
|
|
|
epigastric pain that improves with meals
|
duodenal ulcer
Duodenum creates bicarb protective substance to prepare for acidic food bolus |
|
|
|
What would show up on histology for duodenal ulcer?
|
Hypertrophy of Brunner's gland to compensate for the overproduction of acid.
|
|
|
|
Complications of posterior duodenal ulcers
|
bleeding from gastroduodenal artery and acute pancreatitis
|
|
|
|
Epigastric pain that worsens with meals
|
Gastric ulcer, acid production from onset of meal exacerbates ulceration.
|
|
|
|
Gastric Ulcer etiology
|
also caused by H. pylori. Can also be related to NSAID use.
|
|
|
|
Where is a gastric ulcer most likely to affect?
|
the lesser curvature of the antrum.
|
|
|
|
Gastric ulcer complication
|
Since they are usually located on the lesser curvature, rupture carries risk of bleeding from left gastric artery.
|
|
|
|
Benign/Malignant Stomach Ulcer
|
Duodenal Ulcers are never malignant. Gastric Ulcers on the other hand,
|
|
|
|
Intestinal metaplasia risk factors
|
Nitrosamines, Blood Type A, Chronic Gastritis
|
|
|
|
Diffuse type gastric carcinoma
|
signet rings that diffusely infiltrate gastric cell.
Desmoplasia results in thickening of stomach wall(linitis plastica) NOT associated with intestinal gastric carcinoma risk factors. |
|
|
|
Desmoplasia
|
Desmoplasia is a reactive response of the stroma.
Fibrous tissue and blood vessels responds to the invasive tumor which thickens the stomach wall(linitis plastica) |
|
|
|
Acanthosis Nigricans
|
thickening and darkening of skin near axillary region
A/w Diabetes Type II and gastric carcinoma |
|
|
|
Leser Trelat Sign
|

dozens of seborrheic keratoses erupt spontaneously.
|
|
|
|
Which notable lymph node drains the stomach?
|
left supraclavicular lymph node(Virchow's node)
|
|
|
|
Common metastasis of gastric carcinoma?
|
intestinal - Sister Mary Joseph nodule, metastasis to periumbilical region
Diffuse - Krukenberg tumor, bilateral metastasis to ovaries. |
|
|
|
Duodenal Atresia A/w?
|
Down's Syndrome
Failure of small bowel to canalize |
|
|
|
"double bubble" sign on x-ray
|
Duodenal atresia
|
|
|
|
bilious vomiting
|
Duodenal atresia
|
|
|
|
Meckel Diverticulum etiology
|
failure of vitelline duct to involute
|
|
|
|
Ectopic tissue in meckel's
|
Gastric and Pancreatic
|
|
|
|
Most common location of volvulus
|
Sigmoid colon(elderly)
Cecum(younger) |
|
|
|
Peyer's patches
|
characteristic of ileum
|
|
|
|
characteristic of jejenum
|
neither brunner's glands or peyer's patches
|
|
|
|
Intussusception in children a/w
|
lymphoid hyperplasia in terminal ileum(peyer's patches) causes intussusception into cecum
|
|
|
|
Intussusception in adults a/w
|
tumor
|
|
|
|
Which saccharides are absorbed in intestine?
|
Glucose, Galactose and fructose
|
|
|
|
HLA associations with Celiac?
|
DQ2 and DQ8
|
|
|
|
Celiac Disease hypersensitivity
|
Type IV hypersensitivity - T-cell mediated
|
|
|
|
Pathogenesis of Celiac disease
|
1.) Gluten is converted into Gliadin which is deamidated by Tissue Transglutaminase(tTG)
2.) Deamidated gliadin is presented by antigen presenting cells via MHC class II 3.) Helper T cells mediate tissue damage |
|
|
|
Small herpes like vesicles on the skin
|

Dermatitis Herpetiformis - due to IgA deposition at the tips of dermal papillae
resolves with gluten free diet |
|
|
|
Celiac disease A/w
|
IgA deficiency
|
|
|
|
Histological finding of celiac disease
|
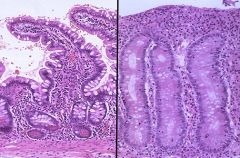
flattening of villi, hyperplasia of crypts and increased intraepithelial lymphocytes.
|
|
|
|
Where is damage of celiac disease most prominent?
|
Duodenum
|
|
|
|
Travel to a tropical region, onset of infectious diarrhea responsive to antibiotics.
|
Tropical Sprue
Damage to small bowel villi due to unknown organism. |
|
|
|
What are celiac patients at increased risk for DESPITE good dietary control?
|
T-cell lymphoma(rare) - Enteropathy Associated T-cell lymphoma
Small bowel carcinoma |
|
|
|
Where is the disease process for tropical sprue in the small bowel?
|
Jejunum and Ileum. This CONTRASTS Celiac which hurts the duodenum.
Secondary complications of Tropical Sprue is malabsorption of Folic Acid(jejenum) and Vitamin B12(ileum) |
|
|
|
Whipple Disease
|
macrophages loaded with T. Whippelii. Partially destroyed organisms in macrophage lysosomes.
|
|
|
|
histology of Whipple Disease
|
lamina propria of small bowel principally affected.
Connective tissue of villi is called lamina propria. Villi surrounded by enterocytes. |
|
|
|
What kind of stain will stain T. Whippelii?
|
PAS stain will show the lysosomes in macrophages filled with the corpses of the critters.
|
|
|
|
Describe pathophys of clinical symptoms of Whipple disease
|
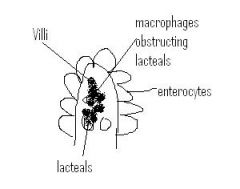
fat from food enters lumen of small bowel. Enterocytes package fat into chylomicrons where they are sent into lacteals present IN THE LAMINA PROPRIA. Since macrophages clog up these lacteals in Whipple disease, you get fat malabsorption and steatorrhea.
|
|
|
|
Abetalipoproteinemia
|
autosomal recessive deficiency of Apolipoprotein B-48 and B-100
|
|
|
|
An absence of plasma VLDL and LDL indicates?
|
an absence of apolipoprotein B-100
|
|
|
|
Defective chylomicron formation indicates?
|
An absence of apolipoprotein B-48
|
|
|
|
What tumor arises in the small bowel?
|
Carcinoid tumor. but these can arise anywhere as well
|
|
|
|
What do carcinoid tumors stain?
|
Chromogranin
|
|
|
|
5-HIAA secretion in urine
|
Serotonin secreted by carcinoid tumor of the small bowel which enters portal circulation and is metabolized by MAO to 5-HIAA.
|
|
|
|
A complication of carcinoid tumor?
|
It can metastasize to the liver, bypassing it's metabolic activity and allowing serotonin to enter systemic circulaiton causing Carcinoid syndrome and carcinoid heart disease.
|
|
|
|
bronchospasm, diarrhea and flushing of the skin
|
Carcinoid syndrome due to liver metastasis and release of serotonin
|
|
|
|
Carcinoid heart disease
|
Serotonin hitting the heart causes fibrosis of right heart valves. Generally right sided valvular fibrosis causing tricuspid regurg and pulmonary valve stenosis.
NO LEFT SIDED VALVULAR DISEASE because MAO in lung will metabolize serotonin before it hits left side. |
|
|
|
Ulcerative Colitis location
|
Starts in the rectum and moves proximally. Furthest it can go is cecum since it ONLY involves large bowel.
|
|
|
|
Ulcerative Colitis symptoms
|
left lower quadrant pain with BLOODY diarrhea
left lower quadrant since it affects the rectum... |
|
|
|
Ulcerative Colitis histological landmark
|
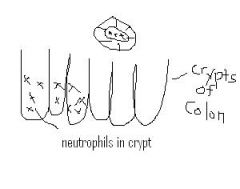
Crypt abscess with neutrophils
|
|
|
|
Ulcerative Colitis gross
|
pseudopolyps, loss of haustra |
|
|
|
Ulcerative Colitis complictions
|
Toxic megacolon - massive dilation of colon, along with febrile symptoms. Possible rupture. |
|
|
|
Ulcerative Colitis A/w
|
Primary Sclerosing Cholangitis and p-ANCA positivity
|
|
|
|
p-ANCA diseases...
|
Microscopic polyangitis
Churg-Strauss ULCERATIVE colitis!! |
|
|
|
What unique thing protects against Ulcerative colitis?
|
smoking/nicotine
|
|
|
|
Crohn's Disease location
|
Can present ANYWHERE from mouth to anus and presents in skip lesions. |
|
|
|
Crohn's disease symptoms
|
Right lower quadrant pain with NON-BLOODY diarrhea
right lower quadrant since terminal ileum usually involved |
|
|
|
Crohn's disease histology
|
Lymphoid aggregates with granulomas
|
|
|
|
Crohn's disease gross
|

cobblestone mucosa, creeping fat and strictures (string sign) |
|
|
|
Crohn's Disease complications
|
1. Malabsorption with nutritional deficiency
|
|
|
|
Calcium oxalate nephrolithiasis
|
Crohn's Disease |
|
|
|
fistula formation
|
Crohn's disease
|
|
|
|
Crohn's Disease A/w
|
Ankylosing Spondylitis, Sacroilitis, Migratory polyarthritis, Erythema Nodosum, Uveitis
|
|
|
|
"lead pipe" sign
|

associated with ulcerative colitis. The loss of haustra, the folds in the colon. |
|
|
|
Auerbach's Myenteric plexus function |
In the muscularis propria in between the inner circular layer and outer longitudinal layer |
|
|
|
Meissner's plexus functions |
in the submucosa |
|
|
|
What kind of biopsy do you need to diagnose Hirschprung disease?
|
Rectal Suction Biopsy
|
|
|
|
Colonic Diverticuli
|
Outpouchings of mucosa and submucosa through muscularis propria
|
|
|
|
"left sided" appendicitis
|
diverticulitis
|
|
|
|
most common disease at splenic flexure
|
ischemic colitis due to presence of watershed areas at splenic flexure
|
|
|
|
high stress right colon
|
angiodysplasia
|
|
|
|
high stress left colon
|
diverticulitis
|
|
|
|
post prandial pain and weight loss
|
ischemic colitis
|
|
|
|
Most common location of hyperplastic polyp
|
left colon(rectosigmoid)
|
|
|
|
Discuss Adenoma-->Carcinoma sequence
|

Normal --> APC increases risk of polyps --> KRAS mutations leads to formation of polyp --> p53 mutation and increased expression of COX allow for progression of carcinoma. |
|
|
|
What protects against the Adenoma --> Carcinoma sequence?
|
Aspirin. Reduces COX
|
|
|
|
Risk factors for adenoma progressing to cancer
|
1.) Size
2.) sessile more risk than pedunculated(mushroom) 3.) villous histology(villous is the villain) |
|
|
|
FAP A/w
|
Turcot Syndrome: |
|
|
|
benign growth in the skull
|
osteoma from Gardner Syndrome.
a/w Fibromatosis and FAP. |
|
|
|
Turcot Syndrome
|
FAP
CNS tumors |
|
|
|
Gardner Syndrome
|
Osteomas
Fibromatosis FAP |
|
|
|
Peutz-Jegher Syndrome
Genetics? |
Autosomal dominant |
colorectal, breast and gynecologic cancer |
|
|
HNPCC MOA?
|
DNA mismatch repair defect
association? |
Ovarian and endometrial carcinoma |
|
|
"napkin ring" lesions.
|
Left sided carcinoma mostly
Adenocarcinoma symptoms? |
Decreased stool caliber
|
|
|
Right sided carcinoma tendencies
|
iron-deficiency anemia secondary to bleeding.
A/w ? |
Microsatellite instability pathway
|
|
|
patient with endocarditis...what GI suspicions?
|
possibility of strep bovis infection that could lead to colonic carcinoma
|
|
|
|
Most common site of distant metastasis of colorectal cancer is...
|
liver
|
|
|
|
CEA
|
NOT useful for screening.
useful for treatment response and recurrence. |
|
|
|
Which is more likely to imply dysplasia? (Erythro or leukoplakia?)
|
Erythroplakia
|
|
|
|
Clinical features of TE fistula
|
air in stomach
aspiration polyhydramnios vomiting |
|
|
|
Esophageal web
|
outpouching of MUCUS layer only.
a/w increased risk of? |
Squamous cell carcinoma
|
|
|
Blood drainage anatomy of esophagus
|
most of esophageal drains to SVC via azygous vein
but some also drains through left gastric vein to portal venous system |
|
|
|
Oral herpes infxn occurrs when |
childhood
what activates it again? |
sunlight and stress |
|
|
oral leukoplakia and erythroplakia are signs of |
SCC of mouth - MC in the floor of the mouth - must biopsy it |
|
|
|
orchitis pancreatitis meningitis |
mumps virus
levels of what will be elevated in the blood |
amylase |
|
|
pleomorphic ademona is malignant or benign? |
benign - MC salivary tumor |
|
|
|
warthins tumor is mal. or benign? |
benign - aleways in parotic - 2nd MC tumor |
|
|
|
which tumor of salivary gland is malignant ? |
mucoepidermoid carcinoma |
|
|
|
vomiting abd distension aspiration |
tracheoesophageal fistula |
|
|
|
esophageal webb increases risk of |
SCC of esophagus |
|
|
|
zenker diverticulum is true or false diverticulum |
false |
|
|
|
painful heamatemesis |
mallory weiss syn (laceration of esophagus) |
|
|
|
painless heamatemesis |
esophageal varices |
|
|
|
describe the two types of esophageal carcinoma |
* both are malignant 1. adenocarcinoma: lower 1/3 / barrets/ GERD/ 2. SCC: upper and mid 2/3 / hot tea, alcohol, smoking, lye injestion, esophageal webb, |
|
|
|
weight loss pain progressive dyspagia hemataemesis |
esophageal cancer signs (hoarse voice is sign of SCC) |
|
|
|
acute gastritis is due to |
acid damage to the stomach mucosa |
|
|
|
causes of acute gastritis |
1. burn (curling ulcer) - hypovolemia 2. Inc ICP (cushing) (increase vagus so increased HCL) 3. NSAIDs 4. alcohol 5. chemo
|
|
|
|
two top causes of chronic gastritis |
1. H.pylori 2. autoimmune gastritis |
|
|
|
therapy for H.pylori |
triple therapy |
|
|
|
how can you prove H.pylori is gone |
1. negative breath urea 2. negative stool antigen |
|
|
|
gastic ulcer vs. carcinoma description |
ulcer is sharply demarkated and looks punched out. VS carcinoma has uneven raised edges - must biopsy |
|
|
|
describe gastric carcinoma |
* both are malignant 1. diffuse: signet cells, thickenining (linitis plastica)
2. intestinal : more common, large, irregular, antrum, due to H.pylori or autoimmune gastritis or nitrosamines or blood type A |
|
|
|
weight loss anemia early satiety abd pain |
gastric carcinoma |
|
|
|
is meckels diverticulum true or false |
true |
|
|
|
volvulus intusseption bleeding before age of 2 |
meckels diverticulum (most is assymptomatic tho) |
|
|
|
LLQ with bloody diarhea |
ulcerative collitis |
|
|
|
RLQ with non-bloody diarhea |
chrons |
|
|
|
define volvulus |
twisting of the intestines on their own messentery |
|
|
|
define intusseption |
telescoping of the proximal end of the bowel into distal end |
|
|
|
thrombosis or embolism of SMA or SMV? |
transmural infarction of small bowel |
|
|
|
abd pain bloody diarhea decreased bowel sounds |
infarction of bowel |
|
|
|
action of lactase |
breaks down lactose into gluc and galactose |
|
|
|
abd distension diarhea failure to thrive in a child |
celiac |
|
|
|
chronic diarhea BLOATING herpes like vesicles on lips |
celiac in adult (dermititis herpataformis) |
|
|
|
lab findings in celiac |
1. IgA or IgG AB to gliadina, tissue transglutaminase, endomysium 2. flattening of villi, elarged crypts |
|
|
|
late complications of celiac |
-T cell lymphoma - small bowel carcinoma (remember it is most prominent in the duodenum). |
|

