![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
118 Cards in this Set
- Front
- Back
|
What part of the GI does not have a Serosa?
|
Esophagus
|
|
|
What is the clinical significance of the Esophagus having no serosa?
|
The esophagus has a worse prognosis with tumors than other parts of GI b/c a tumor growing from the inside-out does not have the Serosal barrier
|
|
|
What is Stomatitis?
|
inflammation of the mucus lining of any structures in the mouth
|
|
|
What is the cause of Viral Stomatitis?
|
HSV-1
|
|
|
What is the agent of Fungal Stomatitis (oral thrush)?
|
Candida albicans
|
|
|
What 3 groups of people are particularly susceptible to Oral Thrush?
|
1. neonates
2. Immunosuppressed with drugs 3. AIDS patients |
|
|
Small vesicles on the lips caused by HSV-1
|
Herpes labialis
|
|
|
Where do dormant HSV-1 migrate to in Herpes Labialis?
|
Trigeminal ganglion
|
|
|
What is another name for Apthous ulcers?
|
Canker sores
|
|
|
What is the cause of Hairy Leukoplakia and what disease is it associated with?
|
1. EBV
2. AIDS |
|
|
Term for a persistent white plaque/patch on the mucosa
|
Leukoplakia
|
|
|
Why does Leukoplakia appear as a white patch?
|
because it is an accumulation of Keratin over the epithelium = Hyperkeratosis
|
|
|
What should Leukoplakia always be considered as potentially being
|
Precancerous!!! So biopsy whenever indicated
|
|
|
Name 4 possible causes of Leukoplakia
|
1. Smoking / chewing tobacco
2. Chronic irritation (dentures) 3. HPV 4. heavy Alcohol use |
|
|
List 3 possible histological appearance of Leukoplakia
|
1. Hyperkeratosis and reactive Acanthosis
2. Dysplasia 3. Carcinoma in situ |
|
|
What is Acanthosis?
|
thickening of squamous epithelium
|
|
|
What is the differential diagnosis with Leukoplakia?
|
Candidiasis
Lichen planus = associated with HCV |
|
|
What is the main clinical significance of of Leukoplakia?
|
it may progress to Invasive Cancer (5%)
|
|
|
Elevated, rugged Leukoplakia that tends to recur and spread and progress to warty squamous cell carcinoma
|
Verrucous Leukoplakia
|
|
|
Red, demarkated flat or raised patch on the mucosa
|
Erythroplakia
|
|
|
What is the histology of Erythroplakia?
|
Epithelial dysplasia
|
|
|
Which has a worse prognosis, Leukoplakia or Erythroplakia?
|
Erythroplakia -> 50% progress to invasive cancer
*Leukoplakia = 5% |
|
|
What percent of all cancers does Oral cancer represent?
|
3%
|
|
|
What gender and age have a higher incidence of Oral Cancer?
|
Males
>40 |
|
|
What are precursor lesions to Oral Cancer?
|
Erythroplakia
Leukoplakia |
|
|
What type of cancer is Oral Cancer (epithelial type)?
|
Squamous cell carcinoma
|
|
|
What are the 3 most often sites of Oral Carcinoma (highest to lowest)
|
1. Floor of the mouth
2. Tongue 3. Palate |
|
|
What are the 3 macro-appearances that Oral Carcinoma can take on?
|
1. Leukoplakia / Erythroplakia
2. Ulcer with indurated margins 3. Nodular or fungating mass |
|
|
What is the significance of metastasis in Oral Carcinoma?
|
Metastases are present in local lymph nodes in >50% at the time of diagnosis!!!
|
|
|
What is the 5-year survival rate for Oral Cancer with surgery and chemotherapy?
|
40%
|
|
|
What is the survival rate if the lymph nodes are involved in Oral Cancer?
|
20%
|
|
|
What percent can be cured surgically if Oral Cancer is caught in the early stages?
|
90%
|
|
|
Inflammed Salivary glands = ?
|
Sialadenitis
|
|
|
What is the primary cause of Sialadenitis?
|
-A calculus, which obstructs the duct in post-operative patients
-Bacteria inflammation is secondary |
|
|
What is an autoimmune cause of Sialadenitis?
|
Sjogren syndrome
|
|
|
Bacterial pathogen most often the cause of Sialadenitis?
|
S. aureus
|
|
|
Name 3 things that can predispose to Sialadenitis
|
1. Oral dehydration
2. immunodeficiency 3. major infections of the mouth |
|
|
What Salivary Gland tumors are more common, benign or malignant?
|
Benign
|
|
|
Name the 3 major salivary glands
|
1. Parotid
2. Sublingual 3. Submaxillary |
|
|
What is the most common site for Salivary gland tumors
|
Parotid gland
|
|
|
T or F: The ratio of benign to malignant tumors in Salivary Glands increases proportionally with the decreasing size of the glands?
|
False: as the size of the glands get smaller the benign:malignant ration decreases = more malignant tumors with smaller gland size
|
|
|
What is the most common benign Salivary Gland tumor?
|
Pleomorphic adenoma
|
|
|
What is the second most common benign salivary gland tumor?
|
Warthin's tumor
|
|
|
What are the 2 most common malignant salivary gland tumors?
|
Mucoepidermoid carcinoma
Carcinoma ex pleomorphic adenoma |
|
|
Part of the esophagus is not formed = ?
|
Agenesis
|
|
|
Absence of a lumen = ?
|
Atresia
|
|
|
A connection between the lumen of the GI tract and another tubular system = ?
|
Fistula
|
|
|
What is the most common Tracheoesophageal Fistula?
|

- Atresia of the proximal esophagus
-fistula connecting trachea to stomach |
|
|
What clinical maternal finding is associated with TE fistula?
|
Polyhydramnios = excess amniotic fluid = swallowed amniotic fluid cannot be reabsorped in the SI
|
|
|
What 3 clinical newborn findings are associated with TE fistula?
|
1. Abdominal distention due to air in stomach from tracheal fistula
2. food regurgitation out of mouth due to Proximal Esophagus atresia 3. Chemical pneumonia from aspiration |
|
|
Upper esophageal diverticula = ?
|
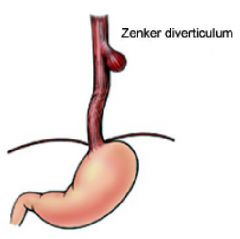
Zenker's (pulsion)
|
|
|
Diverticula of the midportion of the Esophagus (tracheal bifurcation)
|
Traction diverticulum
|
|
|
Pulsion diverticulum at the lower part of the Esophagus
|
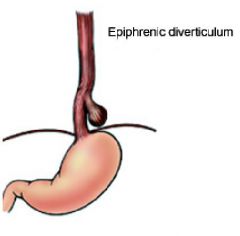
Epiphrenic
|
|
|
What are Traction diverticula due to? give example
|
Pull from the outside
-fibrous adhesions from scarring of lymph nodes in TB |
|
|
What are Pulsion Diverticula due to?
|
Pushing from the inside = increased intraluminal pressure
|
|
|
What 2 things that are associated with causing Epiphrenic Diverticula?
|
1. GERD
2. Diaphragmatic hernia |
|
|
How does a patient with Zenker Diverticulum present?
|
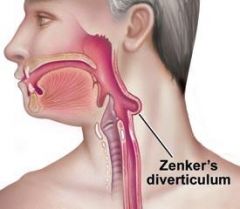
1. Foul odor in mouth (Halitosis) = due to food entrapped in diverticulum
2. Painful swallowing = dysphagia |
|
|
Protrusion of part of the stomach through a hole in the diaphragm into the thoracic cavity
|
Hiatal hernia
|
|
|
What is the most common type of Hiatal hernia?
|
Sliding (90%)
|
|
|
Describe a Sliding Hernia
|
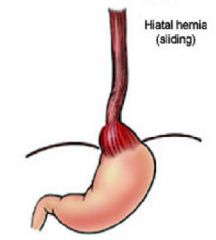
herniation of the proximal stomach through a widened diaphragmatic hiatus = Stomach is pulled up through diaphragm
|
|
|
Describe Paraesophageal hernia
|
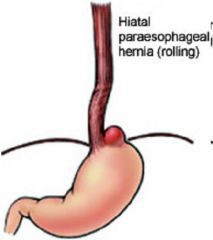
portion of the stomach herniates alonside the distal esophagus
|
|
|
Which Hiatal hernia is more likely to cause necrosis and infarction?
|
Paraesophageal
|
|
|
What 2 things is the incidence of Hiatal hernia increased with?
|
1. age
2. obesity |
|
|
What % of adults have Hiatal Hernias?
|
10-20%
|
|
|
What can be the possible complications of Hiatal Hernia?
|
1. GERD
2. Mucosal ulceration 3. bleeding 4. strangulation of paraesophageal hernia |
|
|
Esophageal motility disorder characterized by aperistalsis and the inability of the Lower Esophageal Sphincter (LES) to relax
|
Achalasia
|
|
|
What is the primary etiology of Achalasia?
|
unknown - but leads to a loss of intrinsic inhibitor innvervation of LES = Vasointestinal peptide
|
|
|
What is the acquired (secondary) cause of Achalasia?
|
Chagas disease = Trypanosoma cruzi
|
|
|
Describe the pathology of Chagas disease causing Achalasia
|
T. cruzi destroys Ganglion cells in Myenteric plexus
- decreases proximal smooth muscle contraction - Loss of Vasointestinal Peptide that normally relaxes LES |
|
|
What is the secondary finding in Achalasia?
|
-Dilation of the aperistaltic esophagus proximal to the constriction
-Muscular hyperplasia |
|
|
What are the clinical findings associated with Achalasia?
|
1. Dysphagia
2. Nocturnal regurgitation with aspiration of food |
|
|
What dose Achalasia pose an increased risk for?
|
Esophageal cancer
|
|
|
Mechanical tears in the mucosa deeper wall of the esophagus following bouts of strainful vomiting
|
Mallory Weiss Syndrome
|
|
|
Who is Mallory-Weiss syndrome usually encountered in?
|
Chronic Alcoholics
*Bulimics too |
|
|
How does a person with Mallory-Weiss Syndrome present clinically?
|
Hematemesis = vomiting blood
|
|
|
What are Esophageal varices due to?
|
increased blood flow through the anastomoses between the portal and central venous circulation
|
|
|
What is the most common cause of Esophageal Varices?
|
Cirrhosis leading to Portal Hypertension
|
|
|
What are the clinical presentations of Esophageal Varices? (3)
|
1. Hematemesis = vomiting blood
2. Melena = black, bloody stools 3. Anemia |
|
|
What is the major complication of Esophageal Varices?
|
Ruptured varices --> bleeding
|
|
|
What is the Prognosis for Esophageal Varices?
|
First episode = 30% die
70-90% die from rebleeding during first 2 years |
|
|
What is the anastomosing vein in Portal Hypertension leading to Esophageal Varices
|
Left gastric vein
|
|
|
inflammation of the esophageal mucosa = ?
|
Esophagitis
|
|
|
What accounts for 90% of Esophagitis?
|
Chemical irritation (reflux of gastric juice) = GERD
|
|
|
What is the underlying cause of infectious esophagitis in most cases?
|
Immunosuppressed persons
Poor Health Debilitated patients |
|
|
What viruses most commonly cause Infectious Esophagitis?
|
HSV-1
CMV |
|
|
What fungus most commonly causes infectious Esophagitis?
|
C. albicans
|
|
|
Focal metaplasia of squamous mucosa to intestinal epithelium
|
Barret esophagus
|
|
|
What gender and race is most often affected by Barrett Esophagus?
|
M:F = 4:1
Whites *Barrett = White Male |
|
|
What is the etiology of Barret Esophagus?
|
Reflux Esophagitis (GERD)
|
|
|
What is the most important complication of Barrett Esophagus?
|
Adenocarcimona of the Esophagus
|
|
|
What is the most common complication of Barrett's Esophagus?
|
Ulceration with stricture formation = narrowing
|
|
|
What countries are more susceptible to getting Carcinoma of the Esophagus?
|
Iran and China
|
|
|
What gender is more likely to get Esophageal Carcinoma?
|
Males are 4X more likely
|
|
|
What part of the Esophagus is more likely to develop cancer?
|
Lower part
|
|
|
What are the 2 types of cancer possible in the Esophagus?
|
1. Squamous cell
2. Adenocarcinoma |
|
|
What is the prognosis for Esophageal Carcinoma?
|
<20% 5-year survival
|
|
|
What is the most common benign tumor of the Esophagus?
|
Leiomyoma
|
|
|
Difficult swallowing = ?
|
Dysphagia
|
|
|
Painful swallowing = ?
|
Odynophagia
|
|
|
What are Esophageal Webs?
|
mucosal folds causing narrowing of the lumen
|
|
|
-Dysphagia caused by webs in the upper esophagus
-Leukoplakia in oral mucosa or esophagus = glossitis -Iron deficiency anemia is the cause |
Plummer-Vinson Syndrome
|
|
|
Subepithelial semicircular fibrous strand in the wall of the esophagus that narrows the lumen at the G-E junction
-May cause dysphagia |
Schatzki ring
|
|
|
Most common tumor of the Salivary Glands
|
Mixed tumor = Pleomorphic adenoma
|
|
|
If someone has viral esophagitis, what is normally the underlying condition?
|
Cancer or Immunosuppression
|
|
|
If someone has Bacterial Esophagitis, what is normally the underlying condition?
|
from chemicals (GERD)
|
|
|
T or F: the most common cause of Dysphagia is functional rather than anatomical
|
False: Anatomical rather than functional
*functional = something is wrong with the wiring |
|
|
What is the most common type of Esophageal Cancer in the upper part?
|
Squamous cell carcinoma
|
|
|
How could you differentiate between Leukoplakia and Candidiasis?
|
Leukoplakia does not wipe off
|
|
|
Leukoplakia
|

This does not wipe off...what is it?
|
|
|
Achalasia
|

What is this pathology?
|
|
|
Mallory-Weiss Syndrome
Alcoholics -> violent retching |

What is this pathology?
Who is it most commonly observed in? |
|
|
Esophageal varices
|

What is this pathology?
|
|
|
Left Gastric Vein
Esophageal varices |

What is the arrow pointing at?
What will this cause? |
|
|
1. Barrett Esophagus
2. chronic GERD 3. Columnar Metaplasia (Squamous -> Columnar) |

What is this called?
What is the most common cause? What pathology is seen? |
|
|
1. Barrett Esophagus
2. Columnar Metaplasia = Goblet cells |
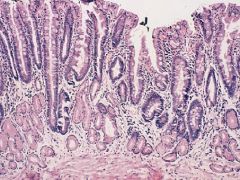
Biopsy from an Esophagus
1. What is the disease? 2. How do you know? |
|
|
What is the treatment for Barrett Esophagus and GERD?
|
Cimetidine = proton pump inhibitor = H2 receptor antagonist
Antacids |
|
|
Squamous cell carcinoma of the Esophagus
-has invaded |
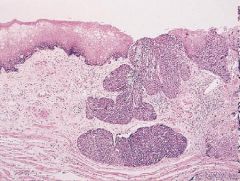
This is a biopsy taken from the Esophagus...what is the diagnosis?
|
|
|
Adenocarcinoma of the Esophagus
Barrett Esophagus |
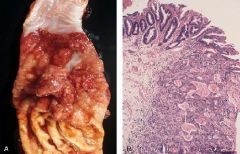
Left?
Right? |

