![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
40 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Transient Ischemic Attack (TIA)
|
<24 hrs of transient focal ischemic neurologic deficit. REVERSIBLE (an hour or so).
mostly due to emboli Can occur in the Anterior, or Posterior circulation. If untreated > 1/3 dev'p stroke (50% in first year) |
|
|
|
Anterior circ. TIA
|
Monocular blindness (TIA): 'pulling shade down on one eye'. than after a while 'shade pulled up'.
'amyrosis fugas' usually unilateral deficits |
|
|
|
Posterior Circ. TIA
|
bilateral deficits
|
|
|
|
Stroke: Cerebrovascular Accident (CVA)
|
suddent onset of non-convulsive, focal, neurological deficit.
Charact. temporal profile. abrupt onset, then progresses, then stops |
|
|
|
Vestibular Schwanoma (acoustic neuroma)
|
schwann cell tumor in inner ear (CN VIII), growing backwards into cerebellar-pontine (CP) angle. resectable.
Histo: a hypocellular area, and hypercellular area (cells form a Veroche body??) |
|
|
|
Craniopharyngioma
|
cystic "motor oil' spills out.
|
|
|
|
Appendimomas
|
cells lining the ventricle (appendimal cells), obstruct CSF flow, causing hydrocephalus
|
|
|
|
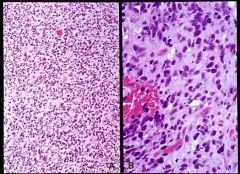
Medulloblastomas
|
exclusively (almost) in cerebellum. Common in childhood < 3yo (cerebellar vermis (midline)). Older, on a side of cerebellum.
could be in 4th ventricle. associated with PNET syndrome. sx: headache, morning emesis, ataxia, gaite disturbances Histo: attempt on neuronal differentiation, looks blue, stopped 12:00 |
|
|
|
Astrocytomas
|
Astrocytomas are classified into 4 grades based on histology: NAME C (necrosis, anaplasia, mitosis, endothelial proliferation, and cellularity). four grades.//
Grade I: well differentiated pilocytic astrocytomas, common in children and young adults, predilection for posterior fossa. Excellent prog.// Grade II: intermediately diff., 3-10 yr survival post tx.// Grade III. called 'anaplastic' astrocytomas, survival 2 years.// Grade IV: called Glioblastoma multiforme, highly malignant with 6 months- a year survial, has the NECROSIS component.// Gross: poorly defined, soft, pale mass in white matter.// Histo: area of hypercellularity, pleomorphic astrocytes with nuclear hyperchromasia and mitotic figure, COAGULATIVE NECROSIS ABSENT.// Presentation: ' 55 yo m with one year hx of headaches w/out any cause, with signs of increased intracranial pressure and left frontal mass on MRI scan. Died shortly afterwards.' |
Presentation: ' 55 yo m with one year hx of headaches w/out any cause, with signs of increased intracranial pressure and left frontal mass on MRI scan. Died shortly afterwards.'
|
|
|
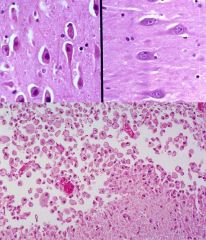
Glioblastoma multiforme
|
This is a grade IV astrocytoma, the most undifferentiated form. It's infiltrative so biopsy of less anaplastic area might mislead, giving false impression of less aggressive tumor. Poor prognosis (6-10 month survival).//
Gross: poorly delineated tan mass with areas of NECROSIS and hemmorhage. Surrounding edema and displacement of normal structure.// Histo: hypercellularity, hyperplasia of endothelial cells, must have necrosis, and serpentine areas of necrosis, bizzare nuclei, brisk mitosis.// 50 yo man admitted after sudden onset of grand mal seizure. He gave a 3 mo hx of heaches and complaining of continuously sensing a poorly defined 'strange smell'. |
50 yo man admitted after sudden onset of grand mal seizure. He gave a 3 mo hx of heaches and complaining of continuously sensing a poorly defined 'strange smell'.
|
|
|
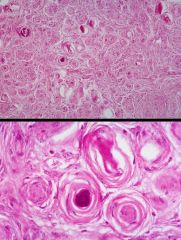
Meningioma
|
sx depend on location, slow growing, attain large size before medical attention sought, cured by resection unless located in surgically unfavorable place. High in middle and later life with 3:2 ration fem: male. associated w/ loss of 22q12 around NF2 gene.//
Gross: firm gray, rounded, well delineated , attached to dura, compresses underlying brain, may arise anywhere from meninges in CNS. Typical site is parasagittal area, dura adjacent to sagittal sinus.// Histo: composed of whorls resembling kertain pearls. Some calcify to form psammoma bodies. Other things with psammoma bodies incl. papillary carcinoma of thyroid, and serous cystadenocarcinoma of the ovary. /// |
47 yo woman with 2 mo hx of increasangly severe headache. Brain scan revealed tumor attached to the dura.
|
|
|
Cerebral Infarct
|
could be either thrombotic or embolic. Majority thrombotic due to atherosclerosis (carotid or vertibrobasilar system). MCA most common for embolic. Transient Ischemic Attacks (TIA) cause momentary focal neurodeficits... indicated of sign. ATH and often herald a total occlusive event. Hemorrhagic infarts are due to lysing of the embolus and restoration of blood flow.//
Ischemic stroke limited to territory irrigated, but hemorrhagic stroke may also involve areas due to edema, compression, and blood in ventricular system.// Primary intracerebral hemmorhage is caused by rupture of intracerebral vessel (freq. due to Charcot-Bouchard aneurysm- microaneurysm along course of small intraparenchymal arteries assoc. with hypertension). Majority occur in basal Ganglia-thalamus region. While, cerebral infarct is due to occlusion***. // Gross: recent ones aresoft to touch >> liquefaction >> cyst.// Histo: Recent infarct: 'dead red' neurons, pyknosis and loss of nuclei, cytoplasmic hypereosinophilia. Some PMNs, mostly 'gitter cells'. // Clinical presenation: 52 yo w/ acute onset of right-sided hemiplegia. He became more lethargic and comatosed and then died 4 days later. // |
Clinical presenation: 52 yo w/ acute onset of right-sided hemiplegia. He became more lethargic and comatosed and then died 4 days later. //
|
|
|
Amyotrophic Lateral Sclerosis (ALS)
|
Muscle degenerative disorder
Unknown cause (Lou Gehrig Disease) Due to degeneration of upper and lower motor neurons of pyramidal motor system Usually leads to death in 2-6 years (exceptional cases such as Stephen Hawking) Sensation remains intact and intelligence is unimpaired |
A 50-year-old male first noted weakness in his hands, with difficulty in handwriting and buttoning his shirt
Weakness progressed to involve upper and lower extremities: lower motor neuron symptoms (muscle atrophy and fasciculations), upper motor neuron symptoms (hyperreflexia, Babinski sign) brainstem involvement with weakness, atrophy and fasciculations in the tongue and facial musculature and dysarthria and impairment of chewing and swallowing Ocular motor function, bodily sensation, intelligence and awareness were unaffected (typical of ALS) The patient died 4 years after onset of symptoms due to progressive respiratory weakness and aspiration pneumonia |
|
|
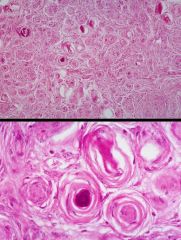
Gross and Histologic Features: ALS
|
Advanced ALS. The precentral gyrus is markedly thinned (<1/2
the thickness of the other gyri). Other cortex regions are unaffected. This atrophy results in a widening of the central sulcus between the precentral and postcentral gyri (top of the photo). The upper motor neurons of the pyramidal tract originate in the precentral gyrus.// Loss of myelin secondary to loss of axonal fibers (indicated by pallor) of lateral corticospinal tracts that carry the upper motor axons neurons of the pyramidal motor pathway. Areas of axonal loss undergo reactive gliosis. Loss of lower motor neurons results in depletion of neurons in the anterior motor horn of the spinal cord with consequent loss of axons in the anterior motor roots.// In addition, you may be able to appreciate demyelination of the ventral (uncrossed) corticospinal tracts.// Note pallor of the lateral corticospinal tracts and the marked atrophy of the anterior motor root (due to axonal loss) as compared to the unaffected posterior sensory root.// |
|
|
|
Clinical Features of ALS
|
Clinical features
Upper motor - hyperactive reflexes, spasticity, Babinski reflex Lower motor – muscle atrophy, fasciculations (esp of shoulder girdle and tongue), weakness Usually extraocular muscles and sphincters are not involved Mean age at onset – 60 years Most common form of motor neuron disease in adults M:F = 1.5-2.1:1 10% familial – earlier onset – SOD1 gene (21) abnormality.// |
|
|
|
What causes the fasciculations?
|
Early in denervation the acetylcholine receptors become
distributed over the whole muscle fiber surface, instead of in the neuromuscular junction. Small amounts of acetylcholine may then propagate an action potential. |
|
|
|
Babinski's Sign?
|
Dorsiflexion of big toe when you stroke the sole of the foot.
Normal for infants, otherwise suggestive of pyramidal tract lesion. |
|
|
|
Alzheimer's Dz
|
Gradual loss of cognitive functions (memory, speech,
orientation, attention, etc) and alteration of behavior (depression, delusions, hallucinations, aggresion, etc).// Definitive dx by Biopsy or autopsy material OR PET scan if the family doesn't want to do autopsy or biopsy.// Clinical severity of AD not correlated with plaque number. |
Case history:
A 62-year-old woman died of sepsis She had a 6 year history of progressive severe memory loss and dementia She was admitted to a psychiatric hospital where she was diagnosed with Alzheimer's disease |
|
|
morphologic features of
Alzheimer’s disease. |
1. Cortical atrophy
2. Neuronal degeneration/destruction 3. Neurofibrillary tangles 4. Neuritic plaques 5. Amyloid vasculopathy// Neurofibrillary tangles and neuritic plaques are essential for Dx.// |
|
|
|
How's definitive Dx of AD made?
|
On the basis of the density and widespread
distribution of these lesions, seen in the clinical setting of dementia. |
|
|
|
AD: Gross Features
|
Diffuse cortical atrophy – esp. Frontal, parietal, temporal
Narrow gyri Widened sulci Dilation of ventricles// |
|
|
|
What portions of the brain show the most prominent
neuronal loss in Alzheimer’s disease? |
Cerebral cortex, amygdala, hippocampus and basal
forebrain (basal nucleus of Meynert). |
|
|
|
Why is the basal nucleus of Meynert important?
|
It is the major source of cholinergic input to the other
areas and may be one important reason for the cognitive impairment. The acetylcholine (and related enzymes) depletion is most probably a secondary event. |
|
|
|
Histologic Features:Alzheimer Disease
|
Neurofibrillary tangles – bihelical filaments of abnormal proteins (tau, ubiquitin)
Neuritic plaques Amyloid angiopathy |
|
|
|
What do these
tangles contain? |
Aggregated paired helical filaments made of Tau protein.
The abnormal tau protein impairs binding of protein to microtubules, which then collapse. |
|
|
|
What is contained in the amyloid core?
|
Abnormally cleaved B amyloid protein, derived from APP
(amyloid precursor protein), encoded on chromosome 21. The neuritic processes form before the amyloid core. |
|
|
|
AD Epidemiologics.
|
50-70% of all dementia in adults
Onset 45 years and above Abnormalities of chromosome 1, 14, 19, 21 (Down Syndrome develop early Alzheimer’s) Amyloid derived from amyloid precusor protein (APP) coded by a gene on 21 The “A” peptide in plaques is derived from an APP residue |
|
|
|
What's Pick dz and how to distinguish it from Alzheimer's DZ?
|
Same dementia as in AD
Less frequent than AD Pronounced atrophy of frontal and temporal lobes – “knife-edge” gyri Spares the posterior 2/3 of superior temporal gyrus, and rarely affects parietal or occipital lobes. Neurons may contain basophilic cytoplasmic inclusions of tau and ubiquitin protein (Pick bodies) |
|
|
|
Dementia
|
Dementia is the progressive loss of cognitive function, independent of the state of attention.
|
|
|
|
List some causes of dementia.
|
Alzheimer disease
Pick disease Multi-infarct dementia Neurosyphilis Creutzfeldt-Jakob disease Frontotemporal dementia Dementia with Lewy bodies |
|
|
|
Why would a patient with cortical atrophy develop a chronic subdural hematoma?
|
Allows increased range of motion for bridging veins to rupture.
|
|
|
|
Gross features of cortical atrophy
|
Diffuse cortical atrophy – esp. Frontal, parietal, temporal
Narrow gyri Widened sulci Dilation of ventricles |
|
|
|
Pilocytic Astrocytoma
|
Pilocytic astrocytoma is a brain tumor that occurs predominantly in children and involves the midline, basal and posterior fossa structures. It is generally considered a benign tumor of childhood. It is often cystic and if solid, it tends to be well circumscribed. It is characteristically a contrast enhancing tumour by current imaging investigations (e.g. CT scan, MRI)
Microscopically, the tumor is composed of bipolar cells with long "hairlike" GFAP-positive processes. Rosenthal fibers, eosinophilic granular bodies and microcystes are often present. It is classified as Grade 1 Astrocytoma. |
Case History
Seven year old noted to be hyperactive with decreasing performance in school Complained of dull, generalized headaches, particularly in morning, relieved after standing or vomiting Bilateral papilledema MRI shows cystic lesion |
|
|
Discuss symptoms based on location of lesion
|
Optic nerve involvement: decreasing vision
Hypothalamic: emaciation, decreased skeletal growth, hypotonia, hypoglycemia Cerebellum: diplopia, nystagmus, ataxia Brain stem: weakness, spasticity, cranial nerve signs |
|
|
|
What genetic alterations are associated with astrocytomas?
|
Low grade - inactivation of p53, overexpression of PDGF-A
Higher grades - disruption of tumor-suppressor genes, the RB gene, the p16/CDKNZA gene and a putative suppressor on chromosome 19 Glioblastoma multiforme - 1/3 have a p53 mutation, another 1/3 have amplification of EGFR gene and the last 1/3 have neither change |
|
|
|
Incidence and location of more common CNS tumors in children
|
Astrocytoma: 50% (Supratentorial -50%,Cerebellum -35%, Brain Stem -15%)//
Primitive Neuroectodermal Tumor: 20% (Cerebellum -85%, Supratentorial -15%) Ependymoma: 13% (Infratentorial -65%, Supratentorial -25%, Spinal Cord -10%)// Craniopharyngioma: 10% (Suprasellar ~100%) |
|
|
|
Astrocytomas
|
Astrocytomas are classified into 4 grades based on histology: NAME C (necrosis, anaplasia, mitosis, endothelial proliferation, and cellularity). four grades.//
Grade I: well differentiated pilocytic astrocytomas, common in children and young adults, predilection for posterior fossa. Excellent prog.// Grade II: intermediately diff., 3-10 yr survival post tx.// Grade III. called 'anaplastic' astrocytomas, survival 2 years.// Grade IV: called Glioblastoma multiforme, highly malignant with 6 months- a year survial, has the NECROSIS component.// Gross: poorly defined, soft, pale mass in white matter.// Histo: area of hypercellularity, pleomorphic astrocytes with nuclear hyperchromasia and mitotic figure, COAGULATIVE NECROSIS ABSENT.// Presentation: ' 55 yo m with one year hx of headaches w/out any cause, with signs of increased intracranial pressure and left frontal mass on MRI scan. Died shortly afterwards.' |
Presentation: ' 55 yo m with one year hx of headaches w/out any cause, with signs of increased intracranial pressure and left frontal mass on MRI scan. Died shortly afterwards.'
|
|
|
Glioblastoma multiforme
|
This is a grade IV astrocytoma, the most undifferentiated form. It's infiltrative so biopsy of less anaplastic area might mislead, giving false impression of less aggressive tumor. Poor prognosis (6-10 month survival).//
Gross: poorly delineated tan mass with areas of NECROSIS and hemmorhage. Surrounding edema and displacement of normal structure.// Histo: hypercellularity, hyperplasia of endothelial cells, must have necrosis, and serpentine areas of necrosis, bizzare nuclei, brisk mitosis.// 50 yo man admitted after sudden onset of grand mal seizure. He gave a 3 mo hx of heaches and complaining of continuously sensing a poorly defined 'strange smell'. |
50 yo man admitted after sudden onset of grand mal seizure. He gave a 3 mo hx of heaches and complaining of continuously sensing a poorly defined 'strange smell'.
|
|
|
Meningioma
|
sx depend on location, slow growing, attain large size before medical attention sought, cured by resection unless located in surgically unfavorable place. High in middle and later life with 3:2 ration fem: male. associated w/ loss of 22q12 around NF2 gene.//
Gross: firm gray, rounded, well delineated , attached to dura, compresses underlying brain, may arise anywhere from meninges in CNS. Typical site is parasagittal area, dura adjacent to sagittal sinus.// Histo: composed of whorls resembling kertain pearls. Some calcify to form psammoma bodies. Other things with psammoma bodies incl. papillary carcinoma of thyroid, and serous cystadenocarcinoma of the ovary. /// |
47 yo woman with 2 mo hx of increasangly severe headache. Brain scan revealed tumor attached to the dura.
|
|
|
Cerebral Infarct
|
could be either thrombotic or embolic. Majority thrombotic due to atherosclerosis (carotid or vertibrobasilar system). MCA most common for embolic. Transient Ischemic Attacks (TIA) cause momentary focal neurodeficits... indicated of sign. ATH and often herald a total occlusive event. Hemorrhagic infarts are due to lysing of the embolus and restoration of blood flow.//
Ischemic stroke limited to territory irrigated, but hemorrhagic stroke may also involve areas due to edema, compression, and blood in ventricular system.// Primary intracerebral hemmorhage is caused by rupture of intracerebral vessel (freq. due to Charcot-Bouchard aneurysm- microaneurysm along course of small intraparenchymal arteries assoc. with hypertension). Majority occur in basal Ganglia-thalamus region. While, cerebral infarct is due to occlusion***. // Gross: recent ones aresoft to touch >> liquefaction >> cyst.// Histo: Recent infarct: 'dead red' neurons, pyknosis and loss of nuclei, cytoplasmic hypereosinophilia. Some PMNs, mostly 'gitter cells'. // Clinical presenation: 52 yo w/ acute onset of right-sided hemiplegia. He became more lethargic and comatosed and then died 4 days later. // |
Clinical presenation: 52 yo w/ acute onset of right-sided hemiplegia. He became more lethargic and comatosed and then died 4 days later. //
|

