![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
36 Cards in this Set
- Front
- Back
|
ligand and effect of plaetelet receptor glycoprotein Ia, IIa
|
receptor ligand, collagen; effect: platelet binds collagen
|
|
|
ligand and effect of plaetelet receptor glycoprotein Ib
|
vWF, platelet binds vWF
|
|
|
ligand and effect of plaetelet receptor glycoprotein IIb-IIIa
|
fibrinogen, crosslinks platelets
|
|
|
Platelet Function Analyzer-100 (PFA-100) analysis
|
Whole blood is pumped through an aperture in a membrane coated with collagen and a platelet stimulant (either ADP or epinephrine). The time until the aperture is occluded by platelets is recorded. This test is more sensitive than the bleeding time for diagnosis of platelet disorders. (Of note, the PFA-100 can give a normal closure time when platelets and bleeding are affected by aspirin, if the ADP membrane is used.
|
|
|
primary hemostasis
|
initial platelet plug
|
|
|
secondary hemostasis
|
coagulation cascade
|
|
|
Aspirin inhibition of platelet function
|
inhibits cyclooxygenase so thromboxane A2 is not formed, decreasing platelet aggregation.
|
|
|
Steps of hemostasis after initial platelet adhesion
|
1 platelets release their granule contents, including ADP, fibrinogen and thromboxane A2, which recruit additional platelets to the plug and promote aggregation. /////////////
2 ADP modifies the platelet surface so that fibrinogen can attach to glycoproteins IIb and IIIa, thereby cross-linking platelets. /////////// 3 Activated platelets also express a phospholipid complex (platelet factor 3) which promotes activation of the coagulation factors |
|
|
Clotting pathway tested by PTT (partial thromboplastin time)
|
test of Intrinsic pathway
|
|
|
Clotting pathway tested by PT (Prothrombin time)
|
test of Extrinsic pathway
|
|
|
extrinsic pathway factors
|
includes factor VII and the common steps of factors X, V, thrombin and fibrinogen.
|
|
|
intrinsic pathway factors
|
includes factors XII, XI, IX, VIII and the common steps of factors X, V, thrombin and fibrinogen.
|
|
|
location of synthesis of clotting factors
|
liver, except for VIII (intrinsic pathway), made in endothelial cells
|
|
|
Tissue factor role
|
In vivo, tissue factor is crucial for initiation of the cascade. Tissue factor is expressed on the surface of affected cells when vessel walls are injured. binds to factor VII
|
|
|
role of factor XII
|
not important in vivo
|
|
|
Factor XI function
|
activation is thought to play a role in stabilizing formation of fibrin.
|
|
|
antistatin target
|
specifically inhibits activated factor Xa.
|
|
|
action of factor Xa
|
action of factor Xa, with factor Va, activates prothrombin to thrombin conversion.
|
|
|
action of thrombin
|
Thrombin cleaves fibrinogen to fibrin
|
|
|
fibrin role
|
polymerizes to form a fibrin clot
|
|
|
the fibrinolytic system
|
proteins which lyse clots or inhibit these clotting proteins Antithrombin III (potentiated by heparin) Protein C, Plasminogen, The fibrin split products
|
|
|
Protein C function
|
inhibit factor V and VIII.
|
|
|
Vitamin K dependent proteins involved in thrombosis/hemostasis
|
clotting factors II, VII, IX, and X. Protein C
|
|
|
Hemostasis/clotting factors which require Vitamin K,
|
Synthesis of factors II, VII, IX, X, Protein C and Protein S is dependent on the presence of Vitamin K
|
|
|
Vitamin K function
|
cofactor in a posttranslational modification
adds additional carboxyl group to the glutamate residue dicarboxylic acid appears critical for binding divalent calcium ion |
|
|
Plasminogen importance
|
a plasma protein, can be activated to plasmin, a potent fibrinolytic agent.
|
|
|
The plasminogen activators
|
1) urokinase-like plasminogen activator (uPA): activates free plasminogen in the circulation
2) tissue-type plasminogen (tPA) activates plasminogen only when attached to fibrin. 3)Streptokinase and tPA are used as thrombolytic drugs [Increased plasminogen activator inhibitor-1 (PAI-1) levels are associated with increased risk of MI and other thrombotic events.] |
|
|
The fibrin split products importance
|
the result of lysis of the fibrin, are also potent anticoagulants. A positive fibrin split product test indicates fibrinolysis above baseline.
|
|
|
hemophilia causes, epidemiology, symptoms
|
1 Deficiency of factor VIII (aka hemophilia A or classic hemophilia)
--most commonn incidence of 1 in 10,000, --X-linked recessive disorder --manifest by massive hemorrhage after trauma, and crippling recurrent hemorrhage into joints after minor trauma. --PTT is prolonged due to factor deficiency. --platelet count and the bleeding time, which depend on normal platelet function and normal vWF, may be normal. 2 Factor IX deficiency (aka hemophilia B or Christmas disease) --X-linked recessive, --clinically indistinguishable from classic hemophiliais --more rare (1 in 60,000). 3 Therapy consists of replacing the missing protein. |
|
|
von Willebrand's disease causes, symptoms
|
1 autosomal dominant disorder,
3 defect in the von Willebrand factor. 4 von Willebrand factor mediates binding of platelets to collagen, circulates as a complex with factor VIII 5 bleeding problems in platelet adhesion 6 Laboratory findings include prolonged bleeding time and usually a normal PTT. 7 Tx by replacing von Willebrand factor with cryoprecipitate. |
|
|
acquired disorders of the coagulation system
|
Vitamin K deficiency, Severe liver disease, Deficiency, either acquired or inherited, in protein C, S or antithrombin III, mutation of factor V, anti-phospholipid antibodies, Disseminated intravascular coagulation (DIC),
|
|
|
"Hemorrhagic" (red) infarct occurs in…
|
organs with parallel or double arterial supply, or with venous occlusion.
|
|
|
"White" (pale) infarct occurs in…
|
arterial occlusion of "solid" organs (solidity of tissue limits amount of hemorrhage into infarcted area).
|
|
|
consequences of thromboemboli to lungs
|
Consequences include sudden death (for saddle embolus), acute right heart failure (cor pulmonale), and hemorrhagic infarction of the lung with respiratory difficulties.
|
|
|
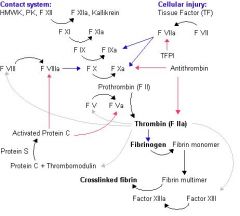
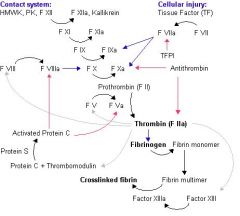
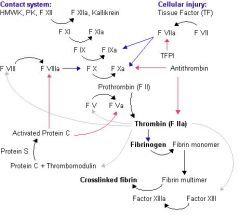
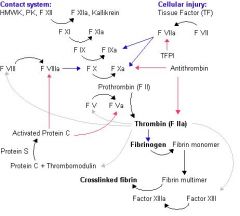
Steps of Extrinsic pathway
|
1) FVIIa circulates and
2) following damage to the blood vessel endothelium Tissue Factor (TF) is released, 3) this then forms a complex with FVIIa (TF-FVIIa) this activates 4) FIX and FX. 5) FXa and its co-factor FVa form the prothombinase complex which activates prothrombin to thrombin. 6) Thrombin then activates other components of the coagulation cascade, including FV and FVII (which activates FXI which in turn activates FIX), and activates and releases FVIII from being bound to vWF. FVIIIa is the co-factor of FXIa and together they form the "tenase" complex which activates FX and so the cycle continues. 7) Thrombin causes cleavage of fibrinogen to fibrin monomers, which 8) becomes crosslinked due to the action of factor XIIIa (activated by thrombin) |
|
|
Inhibition of coagulation
|
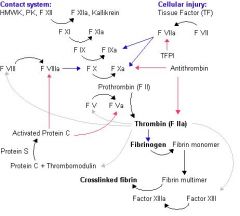
TFPI inhibits VIIa activation of IV and X. ANTITHROMBIN inhibits VIIa activation of X and Thrombin action. PROTEIN C prevents VIIIa activation of X and Va activation of prothrombin
|

