![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
33 Cards in this Set
- Front
- Back
.
|
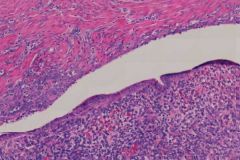
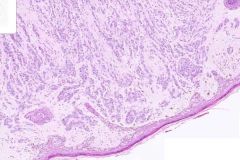
DCIS:
This shows intraductal carcinoma in-situ (DCIS) growing in a comedo pattern. The involved ducts are large and round, and their periphery is lined by a monomorphic population of cytologically malignant cells. These have large atypical nuclei, variably coarse chromatin, and prominent nucleoli. Mitotic figures are easily found. The central part of the involved duct is replaced by brightly eosinophilic necrotic debris, and it is this latter finding that is typical of the comedo pattern of growth. Calcifications are frequently associated with this type of intraductal carcinoma. |
|
.
|
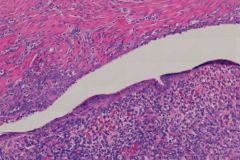
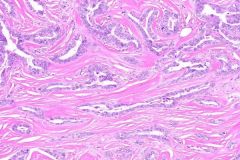
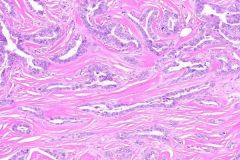
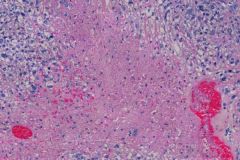
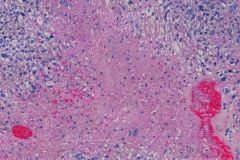
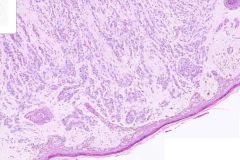
DCIS and Invasive Ductal Carcinoma:
Both intraductal (DCIS) and infiltrating ductal carcinoma (invasive) are present in this image. The intraductal carcinoma is growing in a comedo pattern. In addition, multiple foci of infiltrating ductal carcinoma are also present. Notice the small poorly formed ducts infiltrating through the breast stroma and fat. These are lined by malignant cells similar to those seen in the in situ lesions. |
|
.
|
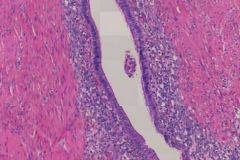
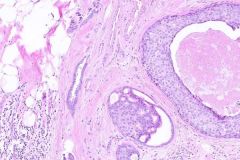
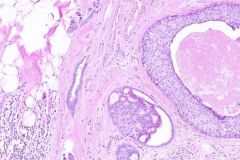
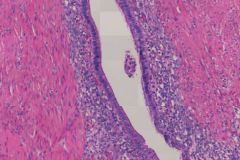
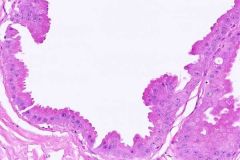
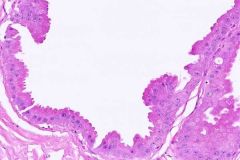
Endometriosis:
The histologic section shows a full thickness section of colon with a normal appearing mucosal surface with underlying smooth muscle. However, there are foci of glandular elements cuffed by a small blue cell population within the smooth muscle. The glandular structures correspond to “normal” endometrial glands surrounded by endometrial type stromal cells. Endometriosis can cause a reactive muscular hypertrophy and thus can simulate a mass. Hemosiderin deposition can be seen but it must be combined with endometrial glands and/or endometrial stroma to make the diagnosis. |
|
.
|
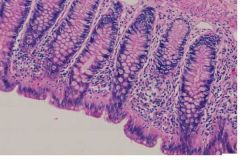
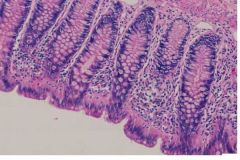
Endometriosis:
(I think this is just normal colon...) **I think you're right! The slides for endometriosis really suck and made no sense to me. The histologic section shows a full thickness section of colon with a normal appearing mucosal surface with underlying smooth muscle. However, there are foci of glandular elements cuffed by a small blue cell population within the smooth muscle. The glandular structures correspond to “normal” endometrial glands surrounded by endometrial type stromal cells. Endometriosis can cause a reactive muscular hypertrophy and thus can simulate a mass. Hemosiderin deposition can be seen but it must be combined with endometrial glands and/or endometrial stroma to make the diagnosis. |
|
.
|
Endometriosis:
The histologic section shows a full thickness section of colon with a normal appearing mucosal surface with underlying smooth muscle. However, there are foci of glandular elements cuffed by a small blue cell population within the smooth muscle. The glandular structures correspond to “normal” endometrial glands surrounded by endometrial type stromal cells. Endometriosis can cause a reactive muscular hypertrophy and thus can simulate a mass. Hemosiderin deposition can be seen but it must be combined with endometrial glands and/or endometrial stroma to make the diagnosis. |
|
.
|
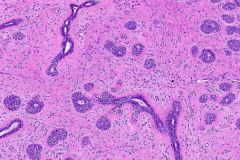
Fibroadenoma:
At higher magnification, fibroadenoma is a biphasic neoplasm composed of both glandular and stromal elements. The glandular component consists of ducts lined by epithelial and myoepithelial cells, some ducts are compressed by the stroma and appear long and cleft-like. The fibrous component is derived from the lobular stroma and is composed of fibroblasts and collagen. The stroma can be myxoid or hyalinized. |
|
.
|
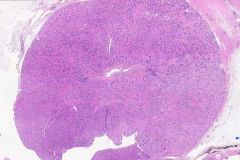
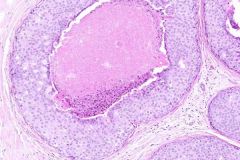
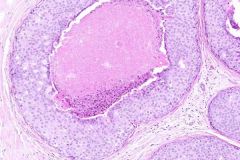
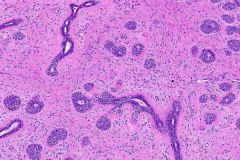
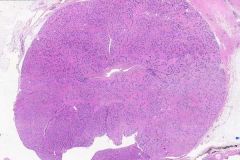
Fibroadenoma:
Fibroadenoma is a benign circumscribed tumor. At low power, you can notice that it is well demarcated from the surrounding breast tissue. Most common benign tumor of the female breast. More common before 30! Presents as mammographic calcification. The epithelium is hormonally responsive, and a slight increase in size may occur during the late phase of menstrual cycle. Regression usually occurs after menopause. The stroma often becomes hyalinized and may calcify. (p 1149 Robbins) |
|
.
|
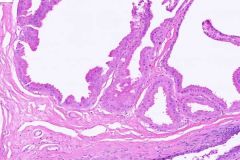
Fibrocystic changes:
The image shows small cysts, stromal fibrosis, and focal ductal epithelial hyperplasia. At low power, you can notice that many of the ducts are cystically dilated. Some of the cysts are lined by tall columnar epithelial cells with pink granular cytoplasm and vesicular nuclei with prominent nucleoli. This is apocrine epithelium, commonly encountered in benign breast diseases, and often lines cysts. The apocrine epithelium is focally hyperplastic, and is thrown up into papillary folds. There is focal evidence of proliferative activity characterized by the piling up of epithelial cells within the ducts. There is no evidence of atypical epithelial hyperplasia. |
|
.
|
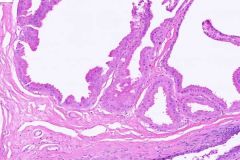
Fibrocystic changes:
The image shows small cysts, stromal fibrosis, and focal ductal epithelial hyperplasia. At low power, you can notice that many of the ducts are cystically dilated. Some of the cysts are lined by tall columnar epithelial cells with pink granular cytoplasm and vesicular nuclei with prominent nucleoli. This is apocrine epithelium, commonly encountered in benign breast diseases, and often lines cysts. The apocrine epithelium is focally hyperplastic, and is thrown up into papillary folds. There is focal evidence of proliferative activity characterized by the piling up of epithelial cells within the ducts. There is no evidence of atypical epithelial hyperplasia. Increased risk for cancer = 1.5 to 2 times |
|
.
|
Fibrocystic changes:
The image shows small cysts, stromal fibrosis, and focal ductal epithelial hyperplasia. At low power, you can notice that many of the ducts are cystically dilated. Some of the cysts are lined by tall columnar epithelial cells with pink granular cytoplasm and vesicular nuclei with prominent nucleoli. This is apocrine epithelium, commonly encountered in benign breast diseases, and often lines cysts. The apocrine epithelium is focally hyperplastic, and is thrown up into papillary folds. There is focal evidence of proliferative activity characterized by the piling up of epithelial cells within the ducts. There is no evidence of atypical epithelial hyperplasia. May mimic carcinoma clinically by producing palpable lumps, mammographic densities or calcifications, or nipple discharge. |
|
.
|
Invasive Ductal Carcinoma:
Characterized by the presence of cords and tubules of infiltrating malignant cells. The stroma is fibrotic. At its periphery, the carcinoma infiltrates the breast parenchyma and fat. Women who are not screened: this presents as a mass and has spread to axillary LNs in over 50%. Women who are screened: this presents as density on mammogram and fewer than 20% have nodal metastases. |
|
.
|
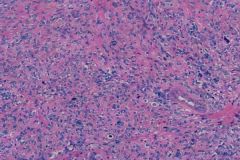
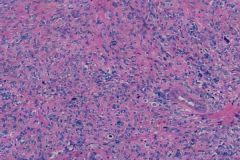
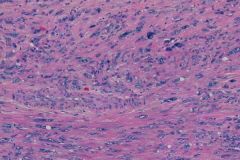
Leiomyosarcoma:
The slide shows a malignant population of smooth muscle cells (spindled cells) with all three features necessary for the diagnosis of a leiomyosarcoma: tumor cell necrosis, nuclear atypia (large bizarre cells of varying sizes and shapes with irregular dark blue nuclei sometimes with prominent nucleoli) and increased mitotic activity including atypical mitotic figures. Uncommon malignant neoplasm, pre and postmenopausal women, recur after removal and distant metastasis. |
|
.
|
Leiomyosarcoma:
The slide shows a malignant population of smooth muscle cells (spindled cells) with all three features necessary for the diagnosis of a leiomyosarcoma: tumor cell necrosis, nuclear atypia (large bizarre cells of varying sizes and shapes with irregular dark blue nuclei sometimes with prominent nucleoli) and increased mitotic activity including atypical mitotic figures. |
|
.
|
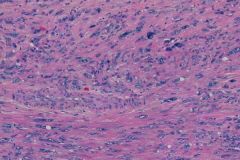
Leiomyosarcoma:
The slide shows a malignant population of smooth muscle cells (spindled cells) with all three features necessary for the diagnosis of a leiomyosarcoma: tumor cell necrosis, nuclear atypia (large bizarre cells of varying sizes and shapes with irregular dark blue nuclei sometimes with prominent nucleoli) and increased mitotic activity including atypical mitotic figures. |
|
.
|
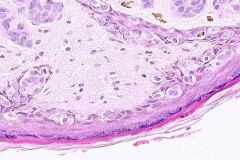
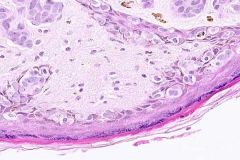
Pagets/Invasive ductal carcinoma:
Look at the stratified squamous epithelium under medium power. You will note the characteristic feature of Paget's disease, namely the presence of numerous atypical nuclei, mainly in the basal portion of the epithelium, and some migrating to upper layers of the epidermis. At high magnification, you will note the presence of individual malignant cells amongst the keratinocytes of the epidermis. The malignant cells frequently have abundant lightly staining cytoplasm, and they have large, cytologically malignant nuclei. The malignant cells are present individually, and in clusters. The stroma is fibrotic. |
|
.
|
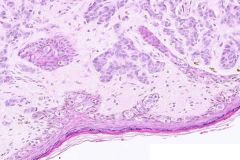
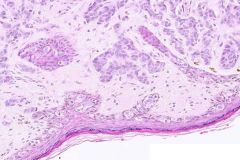
Pagets:
This image shows Paget’s disease of the nipple with underlying infiltrating ductal carcinoma. Paget's disease is characterized by the presence of malignant cells within the epithelium of the nipple. Notice the infiltrating ductal carcinoma within the dermis. It is characterized by poorly formed ducts and cords of malignant cells (similar to the malignant cells infiltrating the epidermis). Remember Paget’s disease is associated with an underlying invasive carcinoma of the breast in 50-60% of cases. |
|
.
|
Pagets / Invasive Ductal Carcinoma:
This image shows Paget’s disease of the nipple with underlying infiltrating ductal carcinoma. Paget's disease is characterized by the presence of malignant cells within the epithelium of the nipple. Notice the infiltrating ductal carcinoma within the dermis. It is characterized by poorly formed ducts and cords of malignant cells (similar to the malignant cells infiltrating the epidermis). Remember Paget’s disease is associated with an underlying invasive carcinoma of the breast in 50-60% of cases. |
|
|
Stages of cervical squamous cell carcinoma (FIGO):
|
I. confined to cervix
II. beyond cervix but not lower 1/3 of vagina; NOT on pelvic wall III. to pelvic wall (lower 1/3 vagina) IV. beyond pelvis (bladder, rectum) |
|
|
Female repro. adenocarcinoma that is associated with p53 mutation and is always considered a Grade 3 tumor with poor prognosis:
|
Serous adenocarcinoma of the uterus
* fibrovascular core * prominent nucleoli * hyerchrom... yadda, yadda... |
|
|
Treatment for cervical carcinoma:
|
I. radical hyst and LN-ectomy or radiotherapy
II. radiotherapy and chemo (as radiosensitizing therapy) |
|
|
Treatment for uterine carcinoma:
|
Radiotherapy for extrauterine
Chemo is actually considered palliative. **wow! that sounds rather grim. |
|
|
Treatment for ovarian cancer:
|
Surgery and chemo is most effective combination.
|
|
|
FIGO Stages of endometrial carcinoma:
|
TMN:
I. confined to corpus uterri II. corpus and cervix III. outside uterus, but in pelvis IV. bladder, bowel, or distant mets **most important for prognosis! **check depth from hysterectomy |
|
|
Grading of endometrial carcinoma:
|
G1. well-diff
G2. differentiated with partly solid areas G3. predominantly solid or entirely unndifferentiated **serous and clear cell are automatically classified as G3! |
|
|
Adenocarcinoma endometriod type is associated with:
|
55-65 yo age group
CA-125 Marker! Obesity DM HTM infertility PTEN inactivation Estrogen DES p53 mutation **most common invasive CA in female genital tract. |
|
|
What are the 3 locations/layers in which a Leiomyoma may be found?
|
Subserosal
Submucosal Intramural **spindle cells are Smooth Muscle |
|
|
This histologic finding is found in what disorder:
"Stromal hyperthecosis" or diffuse hyperplasia of the theca cells of the graafian follicles |
Polycystic Ovarian Disease
**recall that the primary function of LH is to stimulate the THECA cells to produce androgens. In PCOD the LH levels are high and there are higher levels of androgens, too. |
|
|
Which tumor marker do you see in Serous Adenocarcinoma:
Yolk Sac Tumor: Choriocarcinoma: |
CA-125
AFP hCG |
|
|
Thecoma of the ovary
|
Is a tumor of the ovarian stroma and resembles a fibroid. Combination of fibroblasts and lipid droplets.
Often associated with Meigs Syndrome (ascites and hydrothorax) Also associated with basal cell nevus syndrome. |
|
|
3 types of Borderline LMP Neoplasms of the ovary:
|
Transitional
Serous Mucinous **prolif of epi cells with no invasion into stroma. |
|
|
Cal-Exner bodies are found in:
|
Granulosa Cell Tumor (ovary)
**post-menopausal women **precocious sexual development **may contribute to endometrial hyperplasia and endometrial carcinoma (due to extra Estrogen secretion) |
|
|
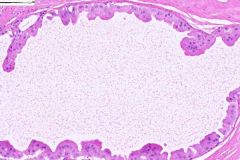
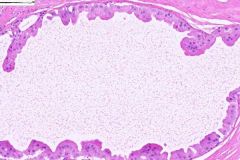
Complete Mole:
|
Diploid karyotype
Nucleus of egg is either lost or inactivated. Sperm duplicates itself! Usually no fetal stuff. All villi are edematous! beta-hCG elevated! 2% risk of choriocarcinoma |
|
|
Partial Mole:
|
Triploid
Egg is ferilized by two sperm. There may be partial placentas, membrane and fetal parts. Half of villi are edematous. * beta-hCG is less elevated. * choriocarcinomas are rare. |

