![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
42 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
LN micro findings in SLL?
|
soccer ball nuclei …plasmacytoid nuclei. Small Man plays Soccer (mantle cell lymphomas have same nuclei)
|
|
|
|
nuclear features in mantle cell lymphoma
|
mosaic stainglass nuclei (molded into each other an irregular shaped). compare with SLL nuclei (see hint)
|

|
|
|
mutations in follicular thyroid Ca?
|
PIck my pTen Follicular Rash (PI3k, Pten, Ras)
|
|
|
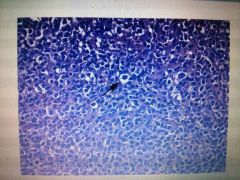
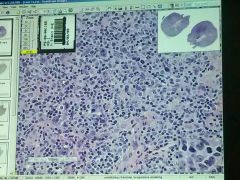
what is this disease? what is the arrow pointing to?
|
marginal zone lymphoma. marginal zone cells classically have a monocytoid appearance (meaning there is a distinct thin halo of clear cytoplasm)
|
|
|
|
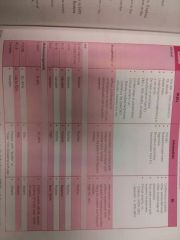
what do the following components of flow cytometry stain for:
CD3, CD20, CD 43, CD5, CD10 |
CD3 is t cell marker
|
|
|
|
What changes do the drug Fibristal cause in the endometrium? what is fibristal?
|
pAEC (progesterone associated estrogen changes). paec is reversible and expected to disappear 6mos after treatment. The drug is approved for use for only three months.
A combo of tubal metaplasia (from estrogen stimulation), inactive epithelium (low cuboidal cells). Glands are NOT hyperplastic (less than 50percent of the field) but are dilated (cystic). + apoptosis of gland cells. + Cytoplasmic vacuoles. stroma: +/-predecidualization (more eosonophilic cytoplasm), There is NO stromal breakdown as seen menstruation or in disordered proliferation. Fibristal is a selective progesterone modulator approved for shrinking fibroids. It has BOTH progesterone antoagonist and agonist changes. Previous cncern that is may cause state of unopposed esteogen and lead ti endometrial hyperplasia and cancer, has been dispelled by research. bottom line: see inactive, cuboidal epithelium that nonetheless has features of secretory phase (vacuoles) and precidualization changes of stroma. |
|
|
|
microscopic findings in psmammomatous melanotic schwanoma? what syndrome is it a part of?
|
found anywhere in PNS, but likes GIT (esophagus, etc).
see pasmmoma bodies and spindle cell architecture. has metastatic potential despite having benign features. Part of the Carney Complex. Multiple neoplasia syndrome with multiple tumors, skin and cardiac myxoma. many pigmented lesions of skin, genitals, mucosa. see eyelid myxomas. |
|
|
|
ddx of multilobulated cystic lesion on Xray of mandible?
|
ondotogenic keratocyst
intraosseous amyloblastoma |
|
|
|
ameloblastoma symptoms and histo?
|
commonly (multicystic)
unicystic also possible. painless swelling of jaws or asymptomatic. micro: highly fibrous (desmoplastic) with crushed glands. sometimes this is all you see! otherwise, supposed to see single tall columnar ameloblast like epithelium see polarization of epi cells with subnuclear vacuolization/clearing. up to 20percent recurrence with curretage |
|
|
|
organs involved in sarcoidosis?
|
90percent have lung lesions.
one third have erythema nodosum. CNS involvement. heart (dilated CMP?) Lofgren's syndrome? |
|
|
|
distribution and histo of pulm sarcoidosis?
|
pulmonary lesions have bronchovascular distribution and vein also penetrate veins-- hemoptysis.
see multinucleated giant cells, asteroid bodies (condensed vimentin and microtubules). also see Schaumann bodies (Schaumann bodies are calcium m=am1"s. protein inclusions inside of Langhans giant cellsas part of a granuloma.) not specific. 25percent of patients get irreversible pulmnoary fibrosis. |
|
|
|
which artery fistualizez with trachea after tracheostomy? what is the incidence?
|
innominate artery. 0.3 to 0.7percent incidence, usually three weeks post tracheostomy. close to 90percent mortality due to hemorrhage.
|
|
|
|
ankylosing spondylitis causes what aortic abnormality?
|
aortic anuerysm
|
|
|
|
what lymphoma is most commonly associated with HTLV? where is it more common?
|
adult t cell leukemia/lymphoma, Japan, southeast asia
|
|
|
|
three post transplant malignancies (PTM)?
|
nonmelanotic skin cancers.
Post transplant lymohomas (EBV implicated often, also HTLV), and Kaposi's (Herpes 8) |
|
|
|
three main mechs of Post transplant malignancies
|
donor malignancy (usually screened out(
recurrent malignancy in recipient de novo malignancy. immunosuporession due to transplant drugs predisposes to malignancy. |
|
|
|
which transplants r most predisposed to PTLD?
|
small bowel transplants are most predisposed to PTLD (post transplant lymphoma disease?). 20percent in adults 30 in kids.
|
|
|
|
who clasification of PTLDs (2008)
|
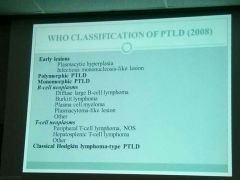
any high grade lymphoma may occur. thr fact the pt is post transplant makes it PTLD.
early lesions still may occur few YEaRS(!) after transplant. monomorphic PTLD include B and T cell neoplasms. |
|
|
|
whatnis the prognosis of early lesions im PTLD? what may be a precurosr lesion to early lesions?
|
some may spontaneously regress. these lesions occur mostly in children and young adults.
possible.precursor: FFH (florid follicular hyperplasia), which is sometimes undistinguished from other inflammatory conditions. |
|
|
|
what are trandformed cells seen in plasmacytic hyperplasia?
|
(larger cells that look like lymphoblasts) note that architecture of LN are.preserved |
|
|
|
tingible body Mphages: how r they formed? what do they look like? significance?
|
Are seen as large cleared out areas in germinal centers. are formed by histiocytes eating up apoptotic bodies (the dying centrocytes, since not all antigen activated Bcells should become memory Bcells).
the apoptic debris forms tingible bodies. Often denotes benign process but not alwsys. |
|
|
|
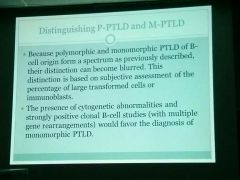
what stain can be used to Ddx PTLD from acute rejection?
|
EBER (EBV stain).
if positive, favor PTLD rather than in acute rejection |
|
|
|
what does CD45 stain? what does CD138 stain? Mum1?
|
CD45 (lymphocyte common antigen) stains lymphocytes.
cd138: plasma cells. BEWARE!! also staims hepatocytes and epithelial cells. correlate with HE! Mum1: plasma cells and other activated (larger) cells. |
|
|
|
what r findings in polymorphic PTLD?
|
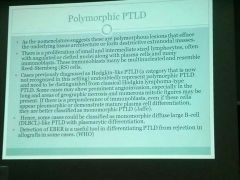
these lesions look like Hogkins but do not STAIN like hogkins. effaces architecture.
do not call these lesions *Hodgkin's like PTLD*. may see prominent angioinvasion and necrosid along with mitosis. polymorphic does not mean benign. bottom line: Polymorphic PTLD immunoblasts may appear like Hodgkin's reed sternberg cells. |
|
|
|
monomorphic PTLD looks like?
|
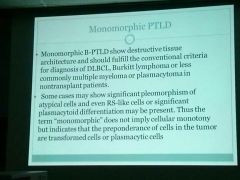
transformed cells= large, activated cells.
|
|
|
|
immunophenotypes of DLBCL? why is it clinically important?
|
germinal center type: CD+, Mum1-
non germinal center type: positive for Mum 1. CD10neg. +/-bcl6. treated the same, but prognostically different: germinal center phenotype has better prognosis. *10 Germs scare away Mums* (germinal center type is CD10+, Mum negative) |
|
|
|
what stains must be done on ALL DLBCLs?
|
cd10 (germinal center marker), bcl6 ( bcl6 stains nuclei), MUM1 is needed
needed to Ddx germinal center vs Non phenotypes. *10 Germs scare away Mums* (germinal center type is CD10+, Mum-) Non germinal center type is the exact opposite. |
|
|
|
what does CD79a stain?
|
Bcells
|
|
|
|
what lymphoma has 99percent ki67?
|
Burkitts.
however, DLBCL can also have skyhigh ki67. To make it conclusive between the two, do FISH: (C-MYC) and/or t(8,14), variant t(2:8) is seen in near 100percent of Burkitts, but is in only 5-8percent of DLBCL. |
|
|
|
what does CD15 stain?
|
CD15 is present on almost all Reed–Sternberg cells, including their rare mononuclear variants, and, as such, can be used inimmunohistochemistry to identify the presence of such cells in biopsies. The presence of these cells is diagnostic of Hodgkin's lymphoma. Reed-Sternberg cells display a characteristic pattern of CD15 positivity, with membranous staining combined with staining of the golgi apparatus. Immunohistochemical panels for the diagnosis of Hodgkins disease typically employ CD15 along with CD30 and CD45; the latter does not stain Reed-Sternberg cells, but does stain almost all other lymphoid cells. CD15 is also present in about 50% of adenocarcinoma cells and can be used to distinguish such conditions frommesothelioma, which is typically negative.[4]
(15 year old boy with a reed in his mouth) CD15 reedsternberg |
|
|
|
what does CD30 stain?
|
this is an activation marker.
expressed by activated, but not by resting, T and B cells. CD30 is associated with anaplastic large cell lymphoma. It is expressed in embryonal carcinoma but not in seminoma and is thus a useful marker in distinguishing between thesegerm cell tumors.[2] CD30 and CD15 are also expressed on classical Hodgkin LymphomaReed-Sternberg cells.[3] |
|
|
|
Bcell markers? other than Cd20
|
pax5, cd79. these r helpful since CD20 not always positive.
B odd: 5 , 79 (+2) |
|
|
|
DLBCL: EBV stains and light chain stains may show what?
|
EBV stains (eBEr) may be negative.
Light chains may show predominance of one type (lamba vs kappa) |
|
|
|
how to do Bcell clonal studies?
|
study for light and heavy chains.
|
|
|
|
many monomorphic PTLDs types are CD? positive?
|
and actually monomorphic and polymorphic has no treatment differences... and no prognosis difference.
many monomorphic types are CD30 positive. |
|
|
|
reed sternberg CD staining results?
|
45-,30+ 15+ (usually), EBER +.
mnemonic: older people (45) do not like chewing reeds. |
|
|
what is this lymphoma? CD45- for the large RS-like cells. CD3 very positive in the small cells. CD20- in atypical cells. CD30 weakly positive in atypical cells. CD15-. EBER++
|
see reed sternberg cells.
Dx was Hodgkin's, despite nonperfect staining. mixed cellularity hogkins: see plasma cells, eosinophils++ (not the case here) so despite its polymorphic look, this is not mixed cellulalarity hodgkins. CD45 can stain RS cells faintly. |
|
|

|
|
|
|

which is TRAP+?
which is CD5 negative? which is t(11:14) positive? |

TRAP+ and CD5-: Hairy cell (trapped in hair)
t(11:14) positive: Mantle cell lymphoma. (11-14 year olds playing on a mantle) |
|
|
|
when is Burkitts called intermediate to DLBcL?
|
when architecture (starry sky) and ki67 (very high).correspond tk Burkitts but it stains positive for bcl2 (favors dlbcl) and is negative for the mutation (t8:14).
|
|
|
|
kappa to lamba relative staining. what ratio is significant?
|
must be 5:1 or more to be significant.
lamba to kappa relative staining must be 2:1 to be significant. normal staining potency is 3:1 kappa to lambda positive staining. |
|
|
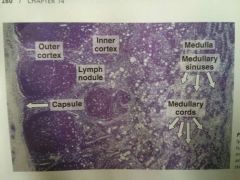
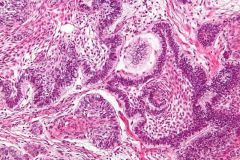
what is each of these structures made of? (cell types)
what is continuous with what? |

continuous: subcapsular sinus (btwn capsule and outerncortex) - intermediate sinuses (which run parallel to invaginations of the capsule)- medullary sinus. ALL SINUSES are partially lined by reticular cells, reticular fibers and macrophages. Carries lymph. The medullary sinuses (pale) run between the medullary chords (basophilic). Continuous: Outer cortex (B cells), inner cortex (T cells), medullary chords (B +plasma cells). Outer cortex: reticular fibers network (and reticular cells) containing B cells. Has nodules of B cells reacting with antigens and becoming immunoblasts (which form the germinal centers) Inner cortex: Fewer nodules. Predominantly T cells. Medullary chords (darkly basophilic): B Cells, plasma cells |
|

