![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
39 Cards in this Set
- Front
- Back
|
What arm of the nervous system is involved in MS (i.e., central or peripheral)?
|
CNS (i.e., brain and spinal cord)
|
|
|
What specifically does the immune system “attack” in multiple sclerosis?
affect on the nervous system? |
Myelin-effecting the conductivity of the action potential (nerve impulse) traveling along the axon
|
|
|
What is myelin?
|
insulation sheath that surrounds the nerve fibers (axons) located in the CNS
|
|
|
Give examples of what de-myelination will have nervous system.
|
fatigue, disturbances of vision, strength, coordination, balance, sensations, bladder and bowl function
|
|
|
Why was this disease called “multiple sclerosis”?
|
Multiple= many areas of the CNS
Sclerosis= scars of plaques |
|
|
What are the four functions of astrocytes?
|
1. Formation of the blood-brain barrier
2. Neurotransmitter reuptake and release 3. Regulation of ion concentration in the extracellular space 4. Promotion of the myelinating activity of the oligodendrocytes |
|
|
What is the function of microglia cells?
|
-macrophages (of brain and spinal cord)
-immune defense of the CNS |
|
|
What is the function of Oligondendrocytes?
|
Myelination:
-of the neuronal axons -can myelinate 50 axons (1um sheath) |
|
|
Why is it that no two MS patients have exactly the same symptoms?
|
Symptoms depend on:
-locations of the lesions within CNS |
|
|
What are the 4 subtypes of MS?
|
1. relapsing-remitting
2. secondary progressive 3. primary progressive 4. progressive relapsing |
|
|
The least common of all subtypes of MS is called?
|
Type 4: Progressive Relapsing MS
steady neurologic decline but also suffer clear superimposed attacks |
|
|
The initial course of all subtypes of MS are called what?
|
Type 1: Relapsing-remitting MS
unpredictable relapses followed by periods of months to years of relative quiet (remission) |
|
|
Sometimes called “galloping MS”, describes around 65% of those with an initial relapsing-remitting MS are called what?
|
Type 2: Secondary progressive MS
begin to have progressive neurologic decline between acute attacks without any definite periods of remission |
|
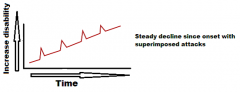
Which MS is this called?
|
Type 4: Progressive Relapsing MS
steady neurologic decline but also suffer clear superimposed attacks |
|
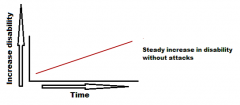
Which MS is this called?
|
Type 3: Primary Progressive MS
~10-15% never have remission after their initial MS symptoms |
|
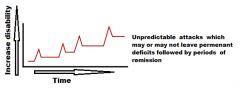
Which MS is this called?
|
Type 1: Relapsing-remitting MS
unpredictable relapses followed by periods of months to years of relative quiet (remission) |
|
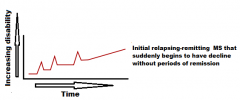
Which MS is this called?
|
Type 2: Secondary progressive MS
begin to have progressive neurologic decline between acute attacks without any definite periods of remission |
|
|
In the genetics of MS, explain ethnicity risk for MS in terms of alleles.
|
Africa: < 0.5 per 100,000
East Asia: 2.8 per 100,000 Americas: 8.3 per 100,000 Europe: 80 per 100,000 Northern European Descent: 200 Per 100,000 |
|
|
What is the chief candidate for the environmental triggers of MS?
|
Epstein-Barr Virus
|
|
|
Does EBV “cause” the disease (i.e. infect the cells of the CNS)?
|
-No
-immune response to this virus is different in MS patients |
|
|
What system of the body actually causes the disease?
|
-altered immune response
EX. EBV "mimics" myelin sheath |
|
|
What autoreactive lymphocyte initiates the pathology of MS?
|
Th1 and Th2 cells
|
|
|
What role do B cells play in the pathology of MS?
|
Activated B:
-enter the CNS -become plasma cells -produce antibodies against myelin sheath -activate the complement system -cause inflammation / demyelination |
|
|
What role do CD8+ cells play in the pathology of MS?
|
-Attack oligodentrocytes
-cause demyelination |
|
|
What type of lesions in the CNS are identified by contrast magnetic resonance imaging (MRI)?
|
Active Lesions
MRI contrast agents (gadolinium): -improve visibility (internal body structures) -administered orally or intravenously -exposed to strong magnetic field -radiofrequency pulse -causes the atoms in the contrast agents to spin -then relax after the pulse stops -detected by the scanner -mathematically converted to an image |
|
|
Explain diagnosis of MS by the presence or absence of oligoclonal bands of IgG in the plasma and cerebral spinal fluid.
|
Immunoglobins produced in CNS IF:
+Oligoclonal bands in CSF --(absent) in blood serum -79%-90% MS patients observable oligoclonal bands |
|
|
What medical procedure is performed to sample cerebral spinal fluid?
|
-Lumbar puncture or Spinal tap
-electrophoresis of CSF -presence of oligoclonal bands in the CSF |
|
|
Whether it be sensory evoked potentials, visual and auditory evoked potentials, what does the latency tell you about the nerve being tested?
|
Speed (ms) of nerve action potential
*Latency / amplitude: -compared to the "normal" |
|
|
Whether it be sensory evoked potentials, visual and auditory evoked potentials, what does the amplitude tell you about the nerve being tested?
|
Strength (mV) of nerve action potential
*Latency / amplitude: -compared to the "normal" |
|
|
Interferon beta-1a (Rebif) and Interferon beta-1b (Betaseron):
What is the type of management of MS for this: a. Corticosteroids (e.g., methylprednisolone) b. Immunomodulators c. Cancer chemotherapeutic Drug d. Humanized Monoclonal antibody e. Exercise |
Immunomodulators
|
|
|
This mode of treatment is counterindicated during relapsing periods:
What is the type of management of MS for this: a. Corticosteroids (e.g., methylprednisolone) b. Immunomodulators c. Cancer chemotherapeutic Drug d. Humanized Monoclonal antibody e. Exercise |
Exercise
|
|
|
During symptomatic attacks (i.e., acute relapses) high doses are used but this treatment is only effective for the short term in relieving symptoms:
What is the type of management of MS for this: a. Corticosteroids (e.g., methylprednisolone) b. Immunomodulators c. Cancer chemotherapeutic Drug d. Humanized Monoclonal antibody e. Exercise |
Corticosteroids (e.g. methylprednisolone)
|
|
|
Appear to reduce the movement of Th1 into the central nervous system by interfering with the Th1 integrin receptor molecules adhering to the VCAM-1 endothelial adhesion molecule:
What is the type of management of MS for this: a. Corticosteroids (e.g., methylprednisolone) b. Immunomodulators c. Cancer chemotherapeutic Drug d. Humanized Monoclonal antibody e. Exercise |
Humanized Monoclonal Antibody
|
|
|
These immune suppressing drugs have little to no impact on recovering function after the attack or prevention of new attacks:
What is the type of management of MS for this: a. Corticosteroids (e.g., methylprednisolone) b. Immunomodulators c. Cancer chemotherapeutic Drug d. Humanized Monoclonal antibody e. Exercise |
Corticosteroids (e.g. Methylprednisolone)
|
|
|
Glatiramer acetate (Copaxone):
What is the type of management of MS for this: a. Corticosteroids (e.g., methylprednisolone) b. Immunomodulators c. Cancer chemotherapeutic Drug d. Humanized Monoclonal antibody e. Exercise |
Immunomodulators
|
|
|
Mitoxantrone, a topoisomerase inhibitor, disrupts DNA synthesis and DNA repair:
What is the type of management of MS for this: a. Corticosteroids (e.g., methylprednisolone) b. Immunomodulators c. Cancer chemotherapeutic Drug d. Humanized Monoclonal antibody e. Exercise |
Cancer chemotherapeutic Drug
|
|
|
Shifts population of T cells from proinflammatory Th1 to regulatory T cells that suppresses inflammation:
What is the type of management of MS for this: a. Corticosteroids (e.g., methylprednisolone) b. Immunomodulators c. Cancer chemotherapeutic Drug d. Humanized Monoclonal antibody e. Exercise |
Immunomodulators
|
|
|
Reduces T-cell activation and proliferation and reduces secretion of pro-inflammatory mediators:
What is the type of management of MS for this: a. Corticosteroids (e.g., methylprednisolone) b. Immunomodulators c. Cancer chemotherapeutic Drug d. Humanized Monoclonal antibody e. Exercise |
Immunomodulators
|
|
|
When using this mode of treatment, it is important for the physical therapist to guard against hyperthermia in that thermal stress can result in decreased motor function and increased symptomatology:
What is the type of management of MS for this: a. Corticosteroids (e.g., methylprednisolone) b. Immunomodulators c. Cancer chemotherapeutic Drug d. Humanized Monoclonal antibody e. Exercise |
Exercise
|

