![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
58 Cards in this Set
- Front
- Back
|
What are the two loops that influence or assist the cerebral cortex (direct motor pathways) in motor control?
|
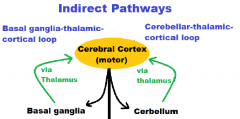
1. Basal ganglia-thalamic-cortical loop
2. Cerebellar-thalamic-cortical loop |
|
|
What type of walking movement is seen with damage to the cerebellum?
|
Ataxic gait
**wide stance, side way jerking back and forth for balance, unability to walk on straight line |
|
|
What type of tremor is seen with damage to the cerebellum?
|
Intention tremor
|
|
|
What does intention tremor do?
|
increases as an extremity approaches the endpoint of deliberate and visually guided movement (hence the name intention tremor).
(overshoot/undershoot; miss target) |
|
|
What are the two loops by which the basal ganglia controls movement?
|
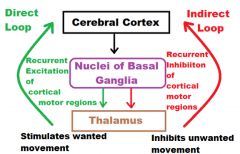
Direct Loop
Indirect Loop |
|
|
Which of the two basal ganglia loops involves recurrent excitation of cortical motor regions (via thalamus)?
Recepetors? Neurotransmitter? |
Direct Loop
D1 Dopamine |
|
|
Which of the two basal ganglia loops involves recurrent inhibition of cortical motor regions (via thalamus)?
Recepetors? Neurotransmitter? |
Indirect Loop
D2 Dopamine |
|
|
Which nucleus in the basal ganglia is directly involved in Parkinson’s disease?
|
Substantia nigra compacta (SNc)
|
|
|
What neurotransmitter is produced by the neurons of SNc (substantia nigra compacta) nucleus?
|
Dopamine
|
|
|
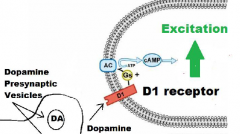
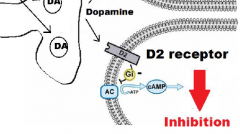
What determines whether the release of Dopamine neurotransmitter in other nuclei within the basal ganglia is excitatory or inhibitory?
|
D1 receptor = excitation
D2 receptor = inhibition |
|
|
What are the two nuclei in the basal ganglia onto which Dopamine neurotransmitter is released?
|
Putamen
Caudate Nuclei |
|
|
What receptor does dopaminergic input from the substantia nigra compacta (SNc) to the putamen and caudate nuclei stimulate in the direct loop?
What is the result? |
D1 receptor:
Increase in thalamocortical excitation |
|
|
What receptor does dopaminergic imput from the SNc to the putamen and caudate nuclei stimulate in the indirect pathway?
What is the effect? What is the result? |
D2 receptor:
-Inhibiting indirect pathway -Results in increasing excitation of the motor cortex |
|
|
What is the overall effect of dopaminergic imput from the SNc to the putamen and caudate nuclei?
|
Increasing excitation of the motor cortex:
-exciting: direct loop -inhibiting: indirect loop |
|
|
What are the neuropathological changes in Parkinson’s disease?
|
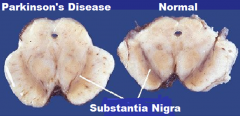
Degeneration:
Substantia nigra compacta (SNc) |
|
|
What is degeneration (in terms on neurophysiology)?
|
Neuronal loss
De-Pigmentation |
|
|
When considering the direct loop, what is the effect of the depletion of dopamine in the
SNc? |
Decreased cerebral cortical excitation over the thalmocortical projection fibers
|
|
|
When considering the indirect loop, what is the effect of the depletion of dopamine in the
SNc? |
Increases:
-putamen / caudate inhibition of the thalamus Results: -inhibits cortex cortical motor regions |
|
|
Characteristics of Parkinson's Disease:
Lines of the patient’s face become smooth, the expression becomes fixed: a. Bradykinesia b. Rigidity c. Postural instability d. Resting tremor e. Parkinsonian gait f. Masked face |
f. Masked Force
|
|
|
Characteristics of Parkinson's Disease:
Slowness of movement, difficulty to initiate and stop movement: a. Bradykinesia b. Rigidity c. Postural instability d. Resting tremor e. Parkinsonian gait f. Masked face |
a. Bradykinesia
|
|
|
Characteristics of Parkinson's Disease:
Shuffling walk with a stooped position and a diminished or absent arm swing: a. Bradykinesia b. Rigidity c. Postural instability d. Resting tremor e. Parkinsonian gait f. Masked face |
e. Parkinsonian gait
|
|
|
Characteristics of Parkinson's Disease:
Trembling in fingers, hands, arms, feet, legs, jaw, or head: a. Bradykinesia b. Rigidity c. Postural instability d. Resting tremor e. Parkinsonian gait f. Masked face |
d. Resting Tremor
|
|
|
Characteristics of Parkinson's Disease:
Stiffness of limbs and trunk: a. Bradykinesia b. Rigidity c. Postural instability d. Resting tremor e. Parkinsonian gait f. Masked face |
b. Rigidity
|
|
|
Characteristics of Parkinson's Disease:
Difficulty to adjust posture to maintain balance, leads to falls: a. Bradykinesia b. Rigidity c. Postural instability d. Resting tremor e. Parkinsonian gait f. Masked face |
c. Postural Instability
|
|
|
When considering the neuropsychiatric disturbances, what is the Parkinsonian patient at risk for that is accompanied with behavior and mood alterations such as depression, apathy, and anxiety?
|
Dementia
|
|
|
Besides the deficits caused by depletion of dopamine in the SNc, what is the second major cause of behavioral alterations?
|
Medication used to managed the disease
|
|
|
Why is levodopa (L-DOPA) rather than dopamine used in the treatment of Parkinson’s disease?
|
L-DOPA:
-cross the blood-brain barrier (unlike dopamine) -enters neurons in SNc (substantia nigra compacta) |
|
|
Initially, why was large doses of L-DOPA needed to treat the disease?
|
L-DOPA rapidly metabolized by DDC (dopadecarboxylase)
|
|
|
What are the side-effects of large doses of L-DOPA?
|
Nausea
Dyskinesias (motor conditions) Joint Stiffness |
|
|
What role does a dopa-decarboxylase (DDC) inhibitors play in the treatment of Parkinson’s disease?
|
DDC inhibitor:
-inhibiting DDC -keeps Levodopa concentration higher -allows 70 % reduction of Levodopa dose -reduces severity of side-effects |
|
|
What role does a catechol-O-methyl transferase (COMT) Inhibitors play in the treatment of Parkinson’s disease?
|
When DDC is inhibited another enzyme, catechol-O-methyl transferase (COMT), takes over the breakdown of Levodopa to 3-O-methyldopa (3-OMD. Consequently, COMT inhibitors were recently developed as a way of further improving the delivery of Levodopa to the brain
|
|
|
What three drugs make up levodopa preparations?
|
1. L-DOPA
2. DDC inhibitors 3. COMT inhibitors |
|
|
Define “on state” in terms of the patients response to Levodopa preparations.
|
Time in which:
-good response to meds -few symptoms |
|
|
Define “off state” in terms of the patients response to Levodopa preparations.
|
Time in which:
-not responding to medication (significant motor defects) -more symptoms |
|
|
What are the two approaches used to extend the time of either no doses or low doses of levodopa preparations?
|
1. Use of Pharmaceutical Alternatives
2. Exercise |
|
|
What is the main reason pharmaceutical alternatives are used in the treatment of Parkinson’s Disease?
|
delay use of levodopa preparations
lower dose of levodopa preparations |
|
|
Explain the action of Dopamine agonists
|
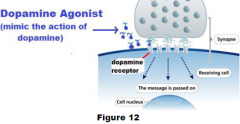
Binds to dopaminergic post-synaptic receptors
(similar effects at L-DOPA) |
|
|
Explain the action of monoamine oxidase-B (MAO-B) inhibitor.
|
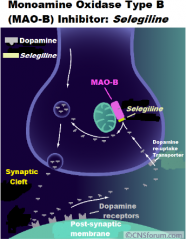
Decreases the metabolism of dopamine:
-in basal ganglia cells -increasing dopamine's availability |
|
|
In terms of Parkinson:
Physical functioning, health-related quality of life: a. Evidence supporting the benefit b. Insufficient evidence to support or refute the benefit c. Need for future research |
a. Evidence supporting the benefit
|
|
|
In terms of Parkinson:
Frequency of exercise in days per week: a. Evidence supporting the benefit b. Insufficient evidence to support or refute the benefit c. Need for future research |
c. Need for future research
|
|
|
In terms of Parkinson:
Reducing falls or depression: a. Evidence supporting the benefit b. Insufficient evidence to support or refute the benefit c. Need for future research |
B. Insufficient evidence to support or refute the benefit
|
|
|
In terms of Parkinson:
Intensity of exercise in terms of RP: a. Evidence supporting the benefit b. Insufficient evidence to support or refute the benefit c. Need for future research |
c. Need for future research
|
|
|
In terms of Parkinson:
Strength, balance and gait speed. a. Evidence supporting the benefit b. Insufficient evidence to support or refute the benefit c. Need for future research |
a. Evidence supporting the benefit
|
|
|
In terms of Parkinson:
Length of exercise bouts in minutes. a. Evidence supporting the benefit b. Insufficient evidence to support or refute the benefit c. Need for future research |
c. Need for Future research
|
|
|
In terms of Parkinson:
Type or mode (e,g, aerobic or resistant) of exercise a. Evidence supporting the benefit b. Insufficient evidence to support or refute the benefit c. Need for future research |
C. Need for future research
|
|
|
What has research demonstrated when comparing an exercise program under physiotherapist supervision vs self-supervised home program?
|
physiotherapist supervision > a self-supervised home program
|
|
|
With Parkinson's Disease:
Why is an exercise program under physiotherapist supervision better than self-supervised home program? |
Found to be more effective at improving:
ADL Motor Mental Emotional Function General Health |
|
|
In this stage levodopa preparations are usually first prescribed. Exercise prescription should be adjusted to the patient’s capabilities and capacities, but continued if the patient is willing.
Which stage of Parkinson’s disease is this? |
Parkinson's Disease: Stage III
|
|
|
Most advanced Parkinson’s disease.
Which stage of Parkinson’s disease is this? |
Parkinson's Disease: Stage V
|
|
|
Exercise should be continued as the primary treatment, with dopamine agonist and MAO-B inhibitors either initiated or continued.
Which stage of Parkinson’s disease is this? |
Parkinson's Disease: Stage II
|
|
|
Physical movements become much slower and major impairments in walking straight and standing are present. Falling down is more common increasing the risk of injuries, especially in the elderly. Generalized dysfunction is moderately severe.
Which stage of Parkinson’s disease is this? |
Parkinson's Disease: Stage III
|
|
|
Symptoms are severe and the individual is unable to complete day-to-day tasks and walking is little, if at all. For these reasons, patients are unable to live alone and are generally confined to a wheelchair. Surgery (e.g., deep brain stimulation therapy) is an option at this stage to alleviate some of the symptoms, but only in young and healthy individuals. A paucity of research exists to determine the feasibility, safety, and outcomes of exercise.
Which stage of Parkinson’s disease is this? |
Parkinson's Disease: Stage IV
|
|
|
Early-Stage Parkinson’s disease
Which stage of Parkinson’s disease is this? |
Parkinson's Disease: Stage I
|
|
|
In Dr. Pitetti’s opinion, exercise should be the primary treatment approach. However, medications may be started during this stage and typically involves the L-DOPA alternatives such as dopamine agonists and monamine oxidase-B (MAO-B) inhibitors.
Which stage of Parkinson’s disease is this? |
Parkinson's Disease: Stage I
|
|
|
Moderate Parkinson’s Disease.
Which stage of Parkinson’s disease is this? |
Parkinson's Disease: Stage III
|
|
|
Symptoms are generally mild and only cause minor inconveniences in day-to-day living. Minor tremors or shaking occurs, but is unilateral, affecting only one side of the body. Along with minor tremors, an individual's posture and balance become poorer and abnormal facial expressions become apparent. Overall, this stage causes no major problems and can last for several years.
Which stage of Parkinson’s disease is this? |
Parkinson's Disease: Stage I
|
|
|
Symptoms are severe enough that individuals are unable to provide self-care and require around-the-clock care. Cachexia occurs in which unwanted loss of weight and muscle mass occurs. The overall quality of life of individuals in this stage declines due to multiple reasons such as speaking and movement difficulties, incontinence issues, frequent hospitalizations and recurrent infections. Therapies are the least effective in this stage of the disease.
Which stage of Parkinson’s disease is this? |
Parkinson's Disease: Stage V
|
|
|
Bilateral symptoms develop in which both sides of the body are affected. Disability is minimal and daily tasks can still be performed, but are much harder to complete. Walking and balance problems become more severe with further declines in posture.
Which stage of Parkinson’s disease is this? |
Parkinson's Disease: Stage II
|

