![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
1036 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Normal Vulva
|
1. stratified squamous epithelium that is keratinized.
2. has hair, sebaceous glands, and sweat glands, the normal components of skin. 3. So, anything that can happen in dermatopathology can also happen in the vulva. |
|
|
|
Herpes Simplex infection of Vulva
|
1. is an STD
2. Can involve the vulva, vagina, and cervix. 3. 80% are due to HSV2 infections 4. Clinically, it presents 3-7 days after sexual intercourse with painful papules that progress to vesicles and ultimately ulcers. 5. These lesions heal spontaneously in 1-3 weeks. 6. Latent infection occurs in the regional nerve ganglia. So, 2/3 people will suffer recurrences. 7. The gravest consequence of herpes simplex is transmission to the neonate during delivery. This risk is highest during active infection, especially the primary infection. |
|
|
|
Herpes Simplex infection of Vulva - Microscopically
|
1. see intranuclear viral cytopathic effects including
a. glassy chromatin, b. margination of the chromatin, c. multinucleation, and d. molding |
|
|
|
Benign conditions of vulva
|
1. Bartholin cyst
2. bartholin abscess 3. ectopic breast tissue |
|
|
|
Bartholin glands
|
1. are paired
2. produce a clear mucoid secretion for lubrication of the vestibule. |
|
|
|
Bartholin cysts
|
1. occur when the ducts that drain the gland are obstructed
2. relatively common, 3. occurs in women of all ages. 4. The cyst is lined by transitional epithelium, which is the epithelium of the normal duct. 5. Less often, you may see a squamous lining due to squamous metaplasia. |
|
|
|
Bartholin Abscess
|
when the bartholin cyst becomes infected with bacteria such as gonorrhea, staph, and some anaerobes.
|
|
|
|
Ectopic breast tissue
|
1. milk-line runs from the axilla to the vulva.
a. So, there may be ectopic breast tissue in the vulva. b. present as small isolated nodules along the milk line 2. This ectopic tissue may enlarge during pregnancy. 3. It can progress into cancer. |
|
|
|
Vulva dystrophy
|
1. presents as leukoplakia
2. patient may have pain or itching on the vulva. 3. two causes are lichen sclerosis and lichen simplex chronicus |
|
|
|
Lichen sclerosis
|
1. is an atrophic vulvitis.
2. Skin is described as being pale, gray, and resembling parchment. 3. usually occurs in post-menopausal women. 4. It may have an auto-immune etiology. 5. There is a slight risk of carcinoma (1-4%). 6. Microscopically, the epidermis is thin, the basal layer becomes hydropic, and the stroma is sclerotic. 7. Will also see dermal inflammation. |
|
|
|
Lichen simplex chronicus
|
1. usually the result of rubbing or scratching.
2. Microscopically, you see hyperplastic dystrophy, a. the squamous epithelium is thickened, b. hyperkeratosis, c. and dermal inflammation. |
|
|
|
Condyloma acuminatum—genital warts
|
1. Related to HPV (usually types 6 or 11)
2. Clinically, it presents as soft, elevated masses. 3. Considered benign tumors 4. Microscopically, a. there is a papillary arrangement of well-differentiated squamous epithelium. b. Will see koilocytes, which are enlarged cells with hyperchromatic raisinoid nuclei with perinuclear clearing. - Koilocytes are the typical viral change associated with HPV. - Koilocytes = diagnostic for HPV |
|
|
|
Premalignant Conditions of the Vulva
|
Dysplasia
|
|
|
|
Dysplasia of vulva
|
1. an abnormal growth and maturation of the epithelium.
- This has been designated vulva intraepithelial neoplasia (VIN) 2. Patients with dysplasia associated with HPV are 15 years younger than those patients whose dysplasia is not associated with HPV. 3. HPV types 16 and 18 are the high risk types for developing dysplasia --> present in 90% of cases a. 5% will progress to invasive carcinoma. b. These 2 types are present in over 90% of cases 4. Bowen’s disease is another term for carcinoma- in –situ. This is in VIN 3. a. Full thickness involvement of epidermis |
|
|
|
Three VINS
|
1. VIN 1= mild dysplasia- bottom 1/3 of the epidermis
2. VIN 2= moderate dysplasia- from bottom, encompasses 2/3epidermis 3. VIN 3= severe dysplasia (carcimona-in-situ): goes to the surface of the epidermis. |
|
|
|
Squamous Cell Carcinoma of the Vulva
|
1. Most common primary cancer of the vulva.
2. It may be exophytic or ulcerated. 3. It is usually slow growing. 4. It can metastasize to inguinal, femoral, or pelvic lymph nodes. 5. Treatment is a vulvectomy. |
growth
metastases = fip treatment |
|
|
Extramammary Paget disease of the Vulva
|
1. This is a very rare intraepithelial adenocarcinoma
2. It probably arises de novo from the epidermal adnexal structures. Uncommonly associated with an underlying malignancy. 3. Clinically, presents as a crusty, elevated, erythematous, and scaly rash. 4. Microscopically: large, pale clear cells along the basal cell layer that will form clusters or glands |
|
|
|
Malignant Melanoma of the Vulva
|
1. Second most frequent cancer of the vulva. Accounts for 5% of vulva neoplasms.
2. More commonly occurs in the 6th or 7th decade. |
|
|
|
Normal Vagina
|
lined by stratified squamous epithelium.
Unlike the vulva, this is nonkeratininzing. |
|
|
|
Benign conditions of the vagina
|
1. Gardner's duct cysts
2. atrophic vaginitis 3. bacterial vaginosis 4. mycotic and yeast infections 5. tricomonas vaginalis |
|
|
|
Gardner’s duct cysts
|
1. develop from mesonephric (Wolffian) duct rests in the vagina.
2. These are usually located on the lateral walls. 3. They are very common 1-2 cm cysts that are lined by cuboidal or low columnar epithelium |
|
|
|
Atrophic Vaginitis
|
1. secondary infection of atrophic vaginal epithelium due to post-menopausal estrogen deficiency.
2. Microscopically, the epithelium has become thin and is easily abraded, which allows organisms easy access resulting in a vaginitis. |
|
|
|
Bacterial Vaginosis
|
1. Due to a shift in the bacterial flora. Normally, lactobacillus is the major component of the vaginal flora, but there can be a shift to more coccobacilli
2. Clinically, this presents as a watery discharge. 3. Microscopically, will see clue cells, which are squamous cells covered with the coccobacilli 4. Gardnerella vaginalis = predominant bacteria |
watery discharge is a CLUE to bacterial vaginosis
|
|
|
Mycotic and Yeast Infections
|
1. Usually due to Candida spp.
2. Affects about 10% of women, who are thought to be carriers of the fungi. 3. More common in people with diabetes, on oral contraceptives, or in pregnancy. 4. Clinically, will see small white surface patches (pruritic) and cheesy discharge. These patients will often complain of itchiness. 5. Microscopically, will see pseudohyphae of the fungus. |
DOC P
|
|
|
Trichomonas Vaginalis
|
1. Due to a protozoan infection.
2. Clinically, this presents with a purulent vaginal discharge, and the cervix looks fiery red (strawberry cervix). 3. Microscopically, one will see a pear-shaped protozoan with one flagella. |
|
|
|
Premalignant conditions of the Vagina
|
1. vaginal intraepithelial neoplasia (VAIN).
- Three types of VAIN a. VAIN I- mild b. VAIN II- moderate c. VAIN III- severe 2. Dysplasia is a precursor lesion for vaginal carcinoma 3. Similar to dysplasia of the vulva, dysplasia of the vagina is often related to HPV. 4. Vaginal lesions are rare. |
|
|
|
Squamous cell carcinoma of the Vagina
|
1. 95% of the primary malignancies of the vagina are squamous cell carcinoma
2. It is most common in the posterior wall of the upper 1/3 of the vagina. 3. Usually affects women between 60-70 years old. 4. These are most often due to extension from a cervical squamous cell carcinoma. Extension from the cervix is much more likely than a primary squamous cell carcinoma in the vagina. |
|
|
|
Vaginal Adenosis
|
1. The presence of glandular tissue within the vagina (usually in the upper 1/3)
2. Not very common anymore 3. Associated with diethylstilbistrol (DES), |
|
|
|
DES
|
1. diethystillbistrol
2. was given in the 1940s and 1950s to women. 3. medication inhibited the normal transformation of the glandular to squamous epithelium in the fetus in the 8th to 18th weeks of gestation. 4. This inhibition was more likely to happen if the medicine was taken earlier in pregnancy and in higher doses. 5. At the time, 1/3 of patients (the babies in utero) exposed developed adenosis. 6. once used extensively during pregnancy to treat threatened and habitual abortion. 7. An estimated 5 million to 10 million Americans received DES during pregnancy 7. Those who were exposed to DES in utero were found to be at risk of developing reproductive tract abnormalities such as clear-cell cervicovaginal cancer in women and reproductive tract abnormalities in men. 8. This is associated with the development of clear cell carcinoma. 9. Very few women who were exposed to DES will develop clear cell carcinoma |
|
|
|
Clear Cell Adenocarcinoma
(Vagina) |
1. Occurs in the anterior upper 1/3 of the vagina (similar to vaginal adenosis)
2. 2/3 of the patients with clear cell carcinoma have a history of exposure to DES 3. Occurs in young age group, 17-22 years old. 4. Cells are clear due to the abundant intracytoplasmic glycogen that is lost during processing |
|
|
|
Embryonal rhabdomyosarcoma (aka Botryoides rhabdomyosarcoma)
|
1. Occurs in young girls, 90% of patients are less than 5 years old.
2. Occurs in anterior vaginal wall 3. Grossly, it looks like a bunch of grapes 4. Microscopically, there is proliferation of myxoid stroma with undifferentiated round and spindle cells, looks like primitive skeletal muscle. 5. has a Cambian layer, which is where the cells crowd around the blood vessels and beneath the squamous epithelium. 6. This is a highly malignant neoplasm with extensive local spread that may metastasize. |
|
|
|
Normal Cervix
|
1. ectocervix is lined with stratified squamous epithelium.
2. The endocervix is lined with mucin-producing columnar epithelium. 3. The squamo-columnar junction is the junction between the ectocervix and the endocervix 4. Squamous metaplasia occurs at the squamo-columnar junction; hence, it is called the transformation zone. This is where most dysplasias and carcinomas originate. 5. Females normally have squamous metaplasia throughout life but the transition zone moves. |
|
|
|
Benign conditions of the Cervix
|
1. Endocervical polyp
2. Microglandular hyperplasia |
|
|
|
Endocervical Polyp
|
1. Most common benign cervical growth
2. This is a complex proliferation of tightly packed, small glands within the endocervix 3. They are lined with mucinous or squamous epithelium. 4. The thing that differentiates this as a polyp is the thick- walled blood vessels within 5. Associated with progestin stimulation due to pregnancy, progesterone, or pills. 6. Clinically, it may present as vaginal bleeding or discharge. |
|
|
|
Microglandular Hyperplasia
|
1. (complex proliferation of tightly packed small glands), presenting as a polypoid mass
2. can be confused with well-differentiated adenocarcinoma 3. associated with progestin stimulation due to pregnancy, progesterone, or pills |
|
|
|
HPV
|
1. an oncogenic DNA virus
2. Associated with intraepithelial neoplasia and carcinoma. However, only a small percentage of patients with HPV develop CIN (cervical intraepithelial neoplasia) 3. Many lesions regress spontaneously 4. More than ¾ of early dysplasias have evidence of infection with HPV. 5. With HPV you can see condylomas, low-grade dysplasia, and high-grade dysplasia. a. Low-grade dysplasia is usually associated with types 6 and 11, which are the low-risk types. b. High-grade dysplasia is usually associated with types 16, 18, 31, 33, and 35 which are the high-risk types. |
|
|
|
Cervical Dysplasia
|
1. progressive changes from the basal layer up
2. Same classification system as vulva and vagina. Cervical intraepithelial neoplasia (CIN) a. CIN I- mild- affects bottom 1/3 of the epithelium, slightly higher than normal N/C ratio, will see koilocytes b. CIN II- moderate- affects bottom 2/3 of the epithelium, moderate N/C ratio c. CIN III-severe- extends to the top of the epithelium, high N/C ratio 3. As the grade of the lesion progresses, the N/C ratio also increases. 4. With mild to moderate dysplasia, 62% regress, 22% persist, and 16% will progress to a more severe lesion. 5. With severe dysplasia, invasive carcinoma develops in 11% within 3 years, 22% within 5 years, and 33% within 9 years. 6. Pap Smear- screening test for cervical dysplasia |
|
|
|
Pap Smear- screening test for cervical dysplasia
|
1. Is no longer a smear; instead, it is collected in a liquid solution
2. Stained with Papanicolaou stain: pink cells are more superficial, bluish cells are more parabasal 3. Low grade= CIN I 4. High grade= CIN II and III |
|
|
|
Squamous cell carcinoma of the cervix
|
1. Deaths due to SSC of the cervix are less common thanks to PAP smears and colposcopy (biopsy).
2. More common in third world countries 3. May grow in exophytic or endophytic manner 4. Clinically, may present with post-coital bleeding 5. Microscopically, will see keratinizing and non-keratinizing types. 6. Spreads by direct extension or lymphatic spread. 7. Usually will have ureteral compression, hydronephrosis, and renal failure (which is the most common cause of death.) |
squamous squashes the ureter
paps sqash the death rate. both keratin and non keratinizing types. hitting the sqashed cervix causes bleediong. |
|
|
Adenocarcinoma of the cervix
|
1. Represents about 8-10% of malignant cervical tumors
2. Associated with high-risk HPV, usually type 18. 3. Mean age of occurrence is 56 years 4. Most of these tumors are well-differentiated and mucin-producing |
A to C by 18
8-10% of malignant cervical tumors. |
|
|
Anatomy of the Uterine Corpus
|
Two components- endometrium and myometrium
|
|
|
|
Endometrium
|
1. the glandular epithelium, it lines the corpus and its divided into:
a. Functionalis- the functional portion that is hormone responsive and shed during the menstrual cycle b. Basalis- the basal layer, the deepest 1/3, endometrium regenerates from this part |
|
|
|
Myometrium
|
the smooth muscle layer
|
|
|
|
Phases of Menstrual Cycle
|
1. Proliferative phase
2. Secretory phase 3. Menstrual phase |
|
|
|
Proliferative phase
|
1. first 14 days of the cycle,
2. functionalis proliferates, 3. the glands change from tubular to coiled, and the stroma becomes more cellular, see mitoses within the glands and stroma |
|
|
|
Secretory phase-
|
1. starts at day 14 (ovulation),
2. the endometrium is under the influence of progesterone produced by the corpus luteum, 3. will see sub-nuclear vacuoles that appear in the endometrial glands. 4. As this phase progresses, the vacuoles will move to a supra-nuclear location, towards the lumen and 5. finally, the secretions in the vacuoles are secreted into the lumen. --cells of the stroma appear plump |
|
|
|
Menstrual phase
|
1. occurs in the absence of fertilization,
2. the degeneration of the corpus luteum resulting in decreased progesterone, 3. collapse of the spiral arteries, and disintegration of the endometrium. |
|
|
|
Endometrial changes associated with pregnancy
|
1. hCG produced by the trophoblast sustains the corpus luteum resulting in a marked increase in progesterone,
2. progesterone has a hypersecretory effect on the endometrium- referred to as an Arias-Stella reaction. 3. This reaction is an exaggerated hyperplasia of the endometrium during pregnancy. This is often confused with a carcinoma. |
|
|
|
Endometritis
|
1. inflammation of the endometrium
2. two types - acute and chronic |
|
|
|
Acute endometritis
|
1. Characterized by PMNs
2. Usually due to an ascending infection 3. Associated with abortion, post-partum changes, or medical instrumentation. |
|
|
|
Chronic endometritis
|
1. Characterized by plasma cells
2. Associated with intrauterine devices, PID, or with retained products of conception 3. Makes dating of the endometrium impossible |
|
|
|
Endometriosis
|
A. Is the presence of endometrial glands and stroma outside the uterine corpus. It can occur anywhere, but it occurs most commonly above the ovaries (about 80% of the time).
B. 10% of women are affected C. Clinically, patients present with pain during intercourse (dyspareunia), dysmenorrhea, or infertility D. Theories about endometriosis: 1. Retrograde menstrual implantation of the endometrial glands 2. Endometrial metaplasia 3. Vascular or lymphatic dissemination of the endometrial tissue |
|
|
|
Chocolate Cyst-
|
1. an ovary that has a cyst due to endometriosis
2. Grossly, will see a blood clot within the cyst 3. Microscopically, will see evidence of hemorrhage, hemosiderin laden macrophages |
|
|
|
Adenomyosis
|
A. It is the presence of endometrial glands and stroma deep into the myometrium.
- The glands may cycle with the endometrium, which can result in menstrual pain. B. Grossly, see dark discoloration at the edges of the endometrial cavity C. Microscopically, may see evidence of hemorrhage in the tissue surrounding the glands |
|
|
|
Endometrial Polyps
|
A. They are benign sessile masses that project into the endometrial cavity. They can be solitary or multiple.
B. Most commonly occur perimenopausal C. Have been seen in association with Tamoxifen, used in breast cancer therapy. D. Clinically, may present with abnormal bleeding E. Grossly, the polyp has a smooth surface and is not invasive F. Microscopically, see dilated glands in the stroma and thick blood vessels (characteristic of polyps) |
they pop up around your menopause.
many or a few associated with tamoxifen... breast cancer therapy POLYPS HAVE THICK BLOOD VESSELS |
|
|
Endometrial hyperplasia
|
1. This is secondary to endogenous or exogenous estrogen
2. There are many causes of endogenous estrogen production such as polycystic ovary disease, obesity, estrogen secreting tumors, and anovulatory cycles 3. The background of endometrial hyperplasia is proliferative endometrium 4. Two types: a. Simple hyperplasia- b. Complex hyperplasia |
|
|
|
Simple hyperplasia
|
1. minimal gland complexity,
2. cystic alterations to the glands with gland crowding, 3. 5% risk of progression to carcinoma |
|
|
|
Complex hyperplasia
|
1. severe gland complexity and crowding,
2. loss of intervening stroma between the glands, 3. 25% risk of progression to carcinoma |
|
|
|
Atypical hyperplasia
|
1. can occur with either the simple or complex hyperplasia,
2. is more likely to happen with complex hyperplasia. 3. It is characterized by atypical cell nuclei. 4. Over a 50% risk of progression to carcinoma. |
|
|
|
Endometrial Adenocarcinoma
|
1. It is the most common invasive cancer of the female genital tract in the US.
2. It occurs most frequently in post-menopausal women, 55-65 years old. a. It usually presents as post-menopausal bleeding. b. Post-menopausal bleeding is considered endometrial adenocarcinoma until proven otherwise. 3. Endometrial carcinomas associated with endometrial hyperplasia tend to be well differentiated; mimicking normal endometrial glands. (you would call this endometrioid adenocarcinoma) |
|
|
|
Risk Factors: related to unopposed estrogen levels
|
1. These women tend to be nulliparous (never having had children).
2. They usually have a history of functional menstrual irregularities consistent with anovulatory cycles. 3. Diabetes 4. Obesity 5. Hypertension 6. Infertility |
|
|
|
common in endometrial adenocarcinoma, as well as endometrial hyperplasia.
|
Inactivation of the PTEN gene and microsatellite instability
|
|
|
|
serous carcinomas
|
1. In these patients, one sees more poorly differentiated tumors.
2. older, subset of patients with endometrial adenocarcinoma that is unrelated to estrogen levels or endometrial hyperplasia 3. Serous carcinomas are more frequently seen in the ovaries. 4. They are linked to p53 mutations and have an overall worse prognosis. |
SERIOUS CARCINOMAS... WORSE PROGNOSSES...
p53 = people aged 53 are serious.... and don't have estrogen!! AD = after death/after menopause |
|
|
Tumors of the Endometrium with Stromal Differentiation
|
1. Endometrial Stromal Sarcoma
2. Malignant Mixed Müllerian Tumors |
|
|
|
Endometrial Stromal Sarcoma
|
1. It presents in middle-aged women (~45 yo), with vaginal bleeding or pelvic pain.
2. It consists of neoplastic endometrial stroma that invades between muscle bundles of the myometrium. 3. Microscopically, you can see spindle cells, which are characteristic of sarcomas. |
stroma is between shit... so it's middle aged women --> 45
|
|
|
Malignant Mixed Müllerian Tumors
|
1. Carcinosarcomas, per Robbins)
2. It’s a relatively rare tumor, often seen in post-menopausal women with prior radiation exposure. 3. Grossly, they present as bulky and very polypoid and usually arise from the POSTERIOR UTERINE FUNDUS. 4. Histologically, there are carcinomatous and sarcomatous elements to these tumors. a. The sarcomatous components may mimic extrauterine tissues (i.e. bone, cartilage, etc.) 5. These tumors have a 5 year survival rate of 20-30%. |
|
|
|
Tumors of the Myometrium
|
1. Leiomyomas (commonly called fibroids)
2. Leiomyosarcomas |
|
|
|
Leiomyomas
|
1. Very common, white, well-circumscribed nodule within the myometrium.
2. When exposed to estrogen, there is enhanced growth of the nodules. 3. Present in 20% of women 30-50 years old, and 40% of women over 50 years old. 4. Histologically, they are composed of whorled bundles of smooth muscle that resemble the uninvolved myometrium. 5. They can occur a. intramurally (which are usually asymptomatic), b. sub-mucosally (which can sometimes occur with bleeding), c. or sub-serosally (which may undergo torsion). |
|
|
|
Leiomyosarcomas
|
1. Malignant neoplasm of the myometrium, usually occurring in older women (~55 yo).
2. Pretty rare (1 in 800 smooth muscle tumors turn out to be leiomyosarcomas) 3. They arise de novo (directly from the myometrium; not a pre-existing leiomyoma) 4. They present either as bulky fleshy masses invading the uterine wall, or as polypoid masses projecting into the uterine lumen. 5. Compared to leiomyomas, you can see areas of hemorrhage and necrosis. 6. Greater than 50% spread to the lung, bone, or brain via hematogenous spread. 7. The diagnosis is based on the usual malignant characteristics (nuclear atypia, increased mitosis, etc.). |
Sarcoma Spreads to lung, bone, or brain by Blood... half of the time.
|
|
|
The Normal Ovary
|
1. Paired organ attached to the posterior aspect of the broad ligament.
2. The outer aspect is lined with epithelium. 3. It is divided into the outer cortex (contains germ cells) and the inner medulla. 4. The ovarian stroma is mesenchymal in origin, and the granulosa and thecal cells produce hormones there. |
|
|
|
Graafian follicle
|
dominant follicle which matures and is shed from the ovary at ovulation
|
|
|
|
Luteinization
|
the granulosa cells surrounding the follicle accumulate lipid and begin to produce progesterone and estrogen.
|
|
|
|
Corpus luteum
|
1. the collapsed follicle which is producing progesterone.
2. Typically has a yellow color, as most things that produce hormones do. |
|
|
|
Cystic Lesions of the Ovaries
|
1. Inclusion Cysts
2. Follicular cysts 3. Corpus Luteum 4. Polycystic Ovarian Disease |
|
|
|
Inclusion Cystys
|
1. very common cysts that result from invaginations of the surface epithelium.
2. They are so common that you could consider them physiological |
|
|
|
Follicular cysts
|
1. originate in unruptured graafian follicles or graafian follicles that ruptured then immediately sealed (Robbins, p. 1092)
2. To be termed a follicular cyst, the cyst has to be greater than 2 cm. If it’s less than 2 cm, it is considered a cystic follicle. 3. Follicular cysts are lined by granulosa cells which can sometimes produce estrogen. |
DEFG == follicular cysts are lined by granulosa cells.
|
|
|
Corpus Luteum cysts
|
1. are lined by luteinized cells and are usually yellow and convoluted with a thick rim.
2. Corpus luteum cysts can produce progesterone. 3. These can produce menstrual irregularities and hemorrhage, and can also rupture and cause peritonitis. |
|
|
|
Polycystic Ovarian Disease (PCOD)
|
(or Stein-Leventhal syndrome)
1. It affects 3-6% of reproductive-age women and is the most common cause of infertility. 2. Patients present with persistent anovulation along with oligomenorrhea (Stedman’s: scanty menstruation) (NT: props to Stedman on use of the word “scanty”) 3. 40% of pts are obese, 50% have hirsutism (Stedman’s: excessive male pattern hair), and very rarely you see virilism. 4. Due to the anovulation, there is an increase in estrogen levels, leading to an increased risk of endometrial and breast cancers 5. Ovaries are enlarged, the outer surfaces are smooth, and they are filled with subcortical follicular cysts. |
|
|
|
Ovarian Tumors
|
1. 80% are benign, with most of the benign tumors in women 20-45 years old.
2. Malignant tumors are found more frequently in older women, between 40 and 65. 3. Ovarian carcinoma is the most common cause of death of the Gyn malignancies, mostly because of its propensity for being detected late and lack of good screening. 4. Risk factors include: a. nulliparity, b. family history of ovarian tumors, c. heritable mutations (BRCA1 and 2), d. history of oral contraceptive use, e. and gonadal dysgenesis in children 5. Tubal ligation decreases the risk for ovarian tumors. 6. Ovarian tumors are divided into 4 categories: Surface epithelial, germ cell, sex cord-stromal, and metastatic |
|
|
|
Ovarian Tumor mutations
|
1. 5% of women less than 70 years old with ovarian cancer have a BRCA1 mutation.
2. 30% of ovarian adenocarcinomas express high levels of HER2/neu (ERB-B2) oncogene which correlates with a poor prognosis. 3. 50% of ovarian carcinomas have p53 mutations. |
|
|
|
Ovarian Tumor categories
|
1. Surface epithelial,
2. germ cell, 3. sex cord-stromal, 4. and metastatic |
|
|
|
Surface Epithelial Tumors
|
1. Serous tumors
2. Mucinous Tumors 3. Endometrial Carcinoma 4. Clear Cell Adenocarcinoma 5. Brenner Tumor 6. overview a. most frequent ovarian tumors (~70%) and most frequent to be malignant (90% of malignant ovarian tumors) b. The risk of malignancy increases as the amount of solid epithelial growth increases |
|
|
|
Serous Tumors
(categories) |
1. Benign
2. Borderline 3. Malignant |
|
|
|
Benign serous tumors
|
1. (70%):
2. present with a smooth wall 3. 20% of benign serous tumors are bilateral. 4. Serous cystadenomas can be very large (15-30 cm), with a smooth, single-cell epithelial-lined wall along with serous fluid inside of it. |
|
|
|
Borderline Serous tumros
|
1. (10-15%)
2. increasing papillary projections and architectural complexity but no evidence of invasion 3. Grossly, you see many papillary projections, but they do not form solid masses 4. Microscopically, you see a more complex papillary architecture, but no invasion into the wall. |
|
|
|
Malignant Serous Tumors
|
1. (15-20%):
2. larger amounts of solid or papillary tumor mass, 3. increased nuclear atypia, and fixation or nodularity of the capsule. 4. Malignant serous tumors are the most common malignant ovarian tumors. 5. 66% are bilateral. 6. The presence of calcified psammoma bodies is indicative of papillary neoplasms. (LYN: “they look like small, round tree stumps”) 7. High levels of serum marker CA-125 are suggestive of serous CystAdenocarcinoma and it is used as a screening test for ovarian tumors. 8. There is frequently peritoneal metastasis of these tumors. 9. Cystadenocarcinoma, the most common carcinoma of the ovary, is a bulky, very solid tumor along with a few papillary-looking areas. - A papillary tumor is defined as having a fibrovascular core with characteristic tumor cells surrounding the core |
|
|
|
Mucinous tumors
|
1. 25% of ovarian neoplasms
2. Only 5% of mucinous tumors are bilateral. 3. They are multi-cystic and contain a sticky, gelatinous fluid. 4. They are more likely to lead to pseudomyxoma peritonei, which consists of an ovarian tumor with extensive mucinous fluid in the peritoneal cavity (ascites), cystic epithelial implants on the peritoneal surfaces, and adhesions. a. Remember, though, that most cases of pseudomyxoma peritonei are associated with appendiceal tumors with secondary ovarian involvement. 5. Types: a. Mucinous cystadenoma b. mucinous cystadenocarcinoma |
|
|
|
Mucinous cystadenoma:
|
1. Grossly, they appear as multiloculated (“honeycomb-like”) tumors filled with the sticky, gelatinous fluid. (Fig 22-44A p. 1097)
2. Microscopically, they are characterized as having a tall columnar epithelial lining with apical mucin and the absence of cilia. (Robbins, p. 1097) |
|
|
|
Mucinous cystadenocarcinomas
|
1. make up 10% of ovarian cancers.
2. They contain more solid growth with epithelial lining atypia, loss of gland architecture, and necrosis (they resemble colon cancer in appearance). |
|
|
|
Endometrioid Carcinoma
|
1. 15-30% are accompanied by carcinoma of the endometrium.
2. 15% coexist with endometriosis. 3. Microscopically they resemble endometriod carcinoma, along with glands that resemble endometrial glands |
|
|
|
Clear Cell Adenocarcinoma
|
1. Rather uncommon and characterized by large epithelial cells with abundant, clear cytoplasm and hobnail cells.
2. Resembles the clear cell adenocarcinoma of the vagina. |
|
|
|
Brenner Tumor
|
1. They are usually unilateral and firm.
2. Microscopically, there is a fibrous stroma with well-demarcated nests of transitional cells (like the epithelium of the bladder). |
|
|
|
Germ Cell tumors
|
1. constitute the second most frequent ovarian tumor. (15-20%)
2. Most are seen in children or young adults, with malignancy rates increasing with younger ages. 3. However, 95% are benign cystic teratomas. 4. Types a. Teratomas b. Dysgerminoma c. Yolk Sac (Endodermal Sinus) Tumor d. Embryonal Carcinoma |
|
|
|
Teratomas (types)
|
1. Mature (Benign) Teratoma (Dermoid Cyst
2. Immature (Malignant) Teratoma 3. Monodermal (Specialized) Teratoma |
|
|
|
Mature (Benign) Teratoma (Dermoid Cyst)
|
1. Most common ovarian neoplasm.
2. Primarily cystic and contains tissue from all 3 germ layers. 3. The thickened area from which hair and teeth arise is called “Rokitansky’s Protuberance”. i. This area is where you would find immature teratoma characteristics. |
|
|
|
Immature (Malignant) Teratoma
|
1. Usually a mixture of embryonic and adult tissues from all 3 germ layers, with the main tissue component being immature neural epithelium rosettes and immature glial elements.
2. Predominantly solid with a smooth external surface. 3. Microscopically, it resembles embryonic rhabdomyosarcomas (you see dark spindle cells). 4. The immature component of this tumor is what makes it malignant. |
|
|
|
Monodermal (Specialized) Teratoma
|
1. Struma ovarii: ovarian tumor composed predominantly of thyroid tissue.
i. If the thyroid tissue is functional, hyperthyroidism can sometimes be seen secondary to the tumor. 2. Carcinoid tumor: presumably arises from the intestinal epithelium within the teratoma and can present with the typical carcinoid syndrome, with symptoms related to the release of serotonin. |
|
|
|
Dysgerminoma
(“The ovarian counterpart of a seminoma in the testis”) |
1. Usually unilateral, large, encapsulated, solid tumors with a lobulated surface.
2. The tumor cells are large cells with a clear cytoplasm which is secondary to glycogen. (Fig 22-51 p.1101) a. NT: I think this means the cytoplasm has aggregates of glycogen in it. 3. The tumor cells have prominent nuclei and are set in nests separated by a fibrous stroma which is infiltrated by lymphocytes. 4. 80% of patients are under 30 years old. 5. Dysgerminomas are very radiosensitive, so they can be controlled by radiation therapy. |
|
|
|
Yolk Sac (Endodermal Sinus) Tumor
|
1. It’s a tumor of children and young adults.
2. It’s important to remember that it produces alpha-fetoprotein (NT: “just like a yolk sac”) 3. Grossly, you can see hemorrhage and necrosis. 4. Microscopically, you see characteristic Schiller-Duval bodies, which are papillary, “glomerular-like” structures with a fibrovascular core surrounded by germ cells. (Fig 22-52 p.1101) a. “enveloped by germ cells within a space lined by germ cells” (Robbins, p. 1101) |
|
|
|
Embryonal Carcinoma
|
(rare in the ovary)
1. Grossly, it’s hemorrhagic and necrotic. 2. Microscopically, you see solid sheets and nests of primitive cells with abortive glandular structures. 3. It looks similar to the yolk sac tumors, except for the abortive glandular formations and that the nuclei are “very ugly” (NT: “the opposite of the kinda-alright , slightly good-looking Schiller-Duval bodies”). 4. You always see high serum HCG levels and AFP levels may be elevated as well. |
|
|
|
Sex Cord- stromal tumors
|
1. make up 5-10% of ovarian tumors
2. Types a. Granulosa Cell tumor b. Fibroma c. Thecoma |
|
|
|
Granulosa Cell tumor
|
1. They have a bimodal age distribution: 5% before puberty and 40% post-menopausal.
2. 75% of the tumor produces excessive amounts of estrogen, which increases the risk of developing endometrial hyperplasia or for endometrial carcinoma. 3. They are usually found unilaterally. 4. They can vary from small, microscopic foci, to large solid or cystic encapsulated masses. 5. Microscopically, characteristic coffee-bean nuclei are seen in rosettes called Call-Exner bodies. 6. Strong immunohistochemical positivity with an antibody to inhibin (an ovarian product produced by the tumor) characterizes these tumors. |
makes estrogen... so it's like a girl and can't decide... bi-modal age distribution... but usually unilateral
G = Grains = cal-exner bodies... and inhibin staining |
|
|
Fibroma
|
1. 76% of stromal tumors
2. Grossly, you see a solid, white, firm mass within the ovary. 3. Microscopically, you see spindle cell proliferation of fibroblasts. 4. When in combination with a hydrothorax (usually on the right side) and ascites, it is termed Meigs syndrome. |
|
|
|
Thecoma
(a tumor can be composed of both a fibroma and a thecoma, called a Fibroma-Thecoma) |
1. Occurs in post-menopausal women.
2. May produce excess estrogen, leading to problems discussed previously. a. The estrogen production gives it a yellow gross appearance. 3. The spindle cells in a thecoma are more “plump” and contain lipid droplets |
THE older population.
|
|
|
Metastatic tumors:
|
1. make up about 5% of ovarian tumors
2. krukenberg tumor |
|
|
|
Krukenberg Tumor
|
1. a metastatic gastrointestinal adenocarcinoma to the ovaries, characterized by bilateral metastases composed of mucin-producing, signet-ring cancer cells, and it is most often of gastric origin, but can be from the breast or large intestine.
2. ***When you see tumors bilaterally, you have to rule out metastases first*** |
|
|
|
The Fallopian Tubes
|
1. Pelvic inflammatory disease
2. ectopic pregnancy 3. adenocarcinoma of the fallopian tube |
|
|
|
Pelvic Inflammatory Disease
|
1. composed of 2 different processes; acute salpingitis and a tubo-ovarian abcess.
2. It is a common cause of infertility. 3. It is sexually transmitted and the most common cause is gonorrhea, followed by chlamydia. 4. It is a result of an ascending infection from the cervix, involving the ovaries and fallopian tubes. 5. Clinically, it presents as cervical motion tenderness, pelvic pain, and a vaginal discharge. 6. Grossly, (NT: “and I quote”), “…this is what you would see is just a big ovary and fallopian tube it’s just like a big inflammatory, nasty, inflammatory mass” (NT: quite the description…eh?) 7. Microscopically, you see numerous PMNs within the mucosa as-well-as within the lumen of the tube, signifying acute purulent exudate. |
|
|
|
Pyosalpinx
|
acute salpingitis with the fallopian lumen filled with acute purulent exudates
|
|
|
|
Tubo-ovarian abcess
|
inflammation involves both the ovary and fallopian tubes and is more associated with polymicrobial or enteric organisms instead of gonorrhea or chlamydia.
|
|
|
|
Atopic pregnancy
|
1. 95% occur in the fallopian tubes.
2. The incidence of atopic pregnancy is markedly increased following PID. 3. hematosalpinx - When trophoblastic invasion into the wall of the tube occurs, there is rupture of the vessels into the fallopian tube, causing a hemorrhage called a hematosalpinx. a. There can also be hemorrhage into the peritoneal cavity, causing life-threatening, massive bleeding. b. The vessels typically rupture around 12 weeks. |
|
|
|
Adenocarcinoma of the fallopian tube
|
1. Extremely rare to be a primary tumor, and much more likely to be a metastases from the ovary or endometrium.
2. Primary adenocarcinomas of the fallopian tubes have been associated with the BRCA mutations. |
|
|
|
The placenta
|
1. Chorioamnionitis
2. Funisitis 3. Vilitis: 4. Placenta accreta |
|
|
|
Chorioamnionitis:
|
1. inflammation of the chorion, amnion, and extra-placental membranes.
2. It results from an ascending infection and is usually associated with premature rupture of the membranes. 3. Pneumonia from inhaling amniotic fluid can occur in the fetus, as-well-as eye, skin, and GI tract infections. 4. Fever and endometritis are complications seen in the mother. 5. Grossly, you see greenish-yellow purulent exudates on the placenta. 6. Microscopically, you see many inflammatory PMNs invading and occupying the amnion and chorion. |
|
|
|
Funisitis
|
inflammation of the umbilical cord
|
|
|
|
Vilitis
|
1. inflammation involving the villi.
2. Both funisitis and vilitis reach the placenta via ascending infection through the birth canal or hematogenous (transplacental) spread. 3. The villi are most often affected by hematogenous spread and the main culprits are TORCH infections (toxoplasmosis, syphilis, TB, listeriosis, rubella, CMV, and herpes simplex). |
|
|
|
Placenta accreta
|
1. caused by partial or complete absence of the decidua with adherence of the placenta directly to the myometrium.
2. associoated with placenta previa |
|
|
|
placenta previa
|
when the placenta implants in the lower uterine segment or cervix
|
|
|
|
Placenta increta
|
when the villi invade into the myometrium
|
|
|
|
Placenta percreta
|
when the villi penetrate through the uterine wall (can cause massive hemorrhage)
|
|
|
|
Gestational Trophoblastic Disease
|
1. constitutes a spectrum of tumors and tumor-like conditions,
2. characterized by proliferation of pregnancy-associated trophoblastic tissue of progressive malignant potential. 3. Types: i. Hydatidiform mole ii. Invasive mole iii. Choriocarcinoma: |
|
|
|
Hydatidiform mole
|
1. . occurs in every 1 in 1,000 or 2,000 pregnancies.
2. They’re associated with high HCG levels. 3. Two types a. complete hydatidiform mole b. partial hydatidiform mole |
|
|
|
complete hydatidiform mole
|
1. presumed to result from fertilization by a sperm of an egg lacking chromosomes;
- so all the chromosomes are paternally derived. (46,XX…but rarely 46,XY) 2. Risk factors: - age less than 15 or more than 50 years old; - a previous molar pregnancy increases the risk 20-fold 3. Clinically, you see - a greatly enlarged uterus for a gestational age, - you may see bleeding, - and there is a markedly increased HCG levels. 4. Classically, on the ultrasound, you see a “Snowstorm effect”. 5. No fetal parts are identified. 6. Grossly, you see “grape-like”, swollen (hydropic) villi. 7. Microscopically, you see enlarged avascular villi with proliferative syncitiotrophoblast. |
|
|
|
partial hydatidiform mole
|
1. due to a normal ovum fertilized by 2 sperm resulting in a triploid (69,XXY).
2. This makes up 25-40% of all moles. 3. Often, fetal parts can be identified. 4. You can see normal and abnormal villi (compared to the complete version where all the villi are abnormal both grossly and microscopically). (NT: Hence the use of the word “complete”) 5. They do not carry a significant risk for choriocarcinoma |
|
|
|
Invasive mole
|
1. the villous trophoblast has invaded into the myometrium. (Fig 22-66 p.1113)
2. If the venous channels are invaded, you can see spread to distant sites, such as the lungs |
|
|
|
Choriocarcinoma:
|
1. epithelial malignant neoplasm of the trophoblast. (Fig 22-67 p.1114)
2. It occurs in 1 in 30,000 pregnancies. 3. 25% follow normal pregnancies, 25% follow spontaneous abortions, and 50% follow hydatidiform moles. 4. There are no chorionic villi present; just strictly cytotrophoblast and syncytiotrophoblast. 5. It’s typically an extremely hemorrhagic tumor 6. There is typically invasion through the venous sinuses into the myometrium and 90% metastasize to the lungs (NT: Robbins says 50%). They can also spread to the brain and GI tract. 7. Choriocarcinomas are associated with markedly elevated HCG levels. 8. Chemotherapy is remarkably effective against choriocarcinomas. |
90% metastasize to the lungs!!!
Venous invasion! |
|
|
Breast anatomy
|
1. Breast tissue consists mostly of fat, and it lies over the pectoralis muscles and the ribs.
2. Glandular organ: Ductules (acini) --> terminal ducts --> larger ducts, which converge at the nipple. 3. The terminal duct-lobular unit (TDLU) is the area of the breast with the most medical significance. a. Most pathological processes, including neoplasms, will be found within this anatomical unit |
|
|
|
Breast Histology
|
1. Stroma-- refers to the “supporting tissue”
2. Epithelium |
|
|
|
Breast Stroma
|
1. INTERlobular stoma represents the tissue lying in between lobules.
i. Dense collagenous material; appears “dark pink” under microscopic 2. INTRAlobular stroma is the tissue that is intimately involved with the ducts and epithelium i. Looser tissue with a lighter pink appearance |
|
|
|
Breast Epithelium
|
a. Duct system normally compromises 2 cell layers
i. Outer layer- flatter, darker, myoepithelial cells that surround the inner layer ii. Inner layer- luminal cells that are rectangular and low columnar in appearance |
|
|
|
Breast Functionality
|
1. Under hormonal influence, the breast matures to its adult form at puberty and menarche. Additional changes take place during pregnancy.
|
|
|
|
Breast changes during Menarche
|
a. Menarche--- onset of menses
i. Ductules form ii. Lobular units are established iii. Amount of adipose tissue decreases in relation to the rest of the breast stroma which results in the radiodense appearance of mature breast tissue during mammography. |
|
|
|
Breast changes during pregnancy
|
b. Pregnancy—change in function dictates the physical change in breast tissue
i. Increase in size and number of lobules; tissue takes on a “swiss cheese” appearance ii. Lipid vacuoles and secretions accumulate iii. The expanded lobular units may make mammography easier to interpret; however, milk deposits and secretions can be falsely identified as tumors or neoplasms rather than nor mal proliferative breast tissue. iv. When getting a mammogram, the physician should know when the patient was last pregnant and when she stopped lactating, as this will determine what you would expect to see. |
|
|
|
Breast Changes during menopause
|
c. Menopause---- breast tissue begins to involute
i. Lobules begin to atrophy and decrease in number ii. Amount of adipose material increases leaving a much fattier breast with decreased stromal density iii. Masses are easier to see with mammography |
|
|
|
Non-neoplastic breast pathology
|
1. Developmental
2. Inflammatory 3. Fibrocystic Change 4. Proliferative |
|
|
|
Developmental Breast Disorders
|
1. Polythelia (extra nipple): extra or supernumerary breast tissue along milk line
2. Gynecomastia: Enlargement of male breast |
|
|
|
Polythelia
|
1. Can be anywhere from the axillary region to the inguinal region
a. note any freckle, birthmark, etc. along this line because it can be ectopic breast tissue 2. Very common and affects at least 1% of the population (Dr. McGoey says this number is too low) 3. Important finding because breast cancer can develop in this extra tissue 4. Polythelia can exist as part of a syndrome and is associated with renal abnormalities 15-20% of the time. a. Physician may find an extra nipple, order a renal ultrasound, and then discover an extra kidney, a horseshoe kidney, or even renal cell carcinoma. |
|
|
|
Gynecomastia
|
1. Common
2. Due to hormonal imbalance caused by an increased estrogen : progesterone ratio. 3. Can be bilateral or unilateral i. Most often unilateral and affects the left breast more often than the right 4. Histologically, gynecomastia shows stromal fibrosis, ductal hyperplasia, and no lobular architecture. i. Looks like pre-pubertal female breast because there will be no menarche or pregnancy to illicit maturation of the tissue. |
|
|
|
hormonal imbalance caused by an increased estrogen : progesterone ratio
|
a. In pubertal or elderly males
b. Cirrhosis --- damaged liver does not breakdown estrogen properly, resulting in increased levels c. Other causes include... i. Estrogen-secreting testicular tumors (Leydig tumor) ii. Marijuana, heroin, anabolic steroids iii. Klinefelter syndrome (47XXY) |
|
|
|
Inflammatory Breast Disorders
|
1. Mastitis --- inflammation of the breast
2. Fat necrosis |
|
|
|
Types of Breast Mastitis
|
1. Acute mastitis
2. Granulomatous mastitis 3. Lymphocytic mastitis 4. Periductal mastitis |
|
|
|
Mastitis Clinical presentation
|
1. includes all the characteristics of inflammation: erythema, edema, pain, and heat.
2. This contrasts the ominous and painless findings of skin thickening and retraction seen in fat necrosis of the breast, another non-neoplastic inflammatory process. |
|
|
|
Acute mastitis
|
1. Occurs in lactating breast often in the 1st month of nursing
2. Patient can be febrile 3. Acute mastitis is most often the result of an infectious etiology i. Organisms invade via cracks or fissures in the nipple; can lead to bacteremia ii. Staph. aureus is the most frequent culprit followed by Streptococcus 4. Histology will show neutrophils (PMN’s) in the ducts 5. Treat with antibiotics and continued lactation |
|
|
|
Granulomatous mastitis
|
1. Associations:
i. Systemic diseases like sarcoidosis ii. Tuberculosis and fungal infections iii. Prosthetics and implants iv. There are also idiopathic causes. 2. Histologically, you would see multinucleated giant cells and a mononuclear inflammatory infiltrate including lymphocytes, macrophages, fibroblasts, etc. 3. Maybe or may not be caseating. |
stop the party iodiot
|
|
|
Lymphocytic mastitis
|
a. Multiple firm bilateral masses
b. Possible autoimmune etiology c. Associations i. Type 1 diabetes mellitus and thyroiditis |
|
|
|
Periductal mastitis
|
1. Can occur at any age
2. >90% smokers 3. Peri-areolar mass +/- fistulous tracts to skin +/- abscess 4. Histology will show squamous-lined fistula with surrounding inflammation (lymphocytes with or without mononuclear granular cells) i. Not infectious 5. Treatment is surgical excision of fistula. |
|
|
|
Fat Necrosis
|
1. Clinical presentation is very ominous; however, fat necrosis is not malignant.
a. There is thickening and retraction of the skin overlying the fat necrosis. b. Painless mass; pain is usually associated with –itis and cancerous masses are usually painless 2. Fat necrosis tends to be found in patients with a history of trauma or a previous surgery. 3. The lesion appears grossly as a mass with ‘chalky flecks of calcification’ 4. Histologically, you see fat necrosis, PMN’s followed by lymphocytes and fibrosis. |
|
|
|
The lesion is most likely not cancer, if one of the following is true
|
1. The patient has inflammatory signs and is lactating
2. The patient has diabetes, sarcoidosis, thryoiditis, or some systemic disease 3. The lesion is painless and the patient has a history of minor trauma (ex. hit steering wheel during car accident) or previous surgery. Think fat necrosis here. |
|
|
|
Inflammation with breast cancer is a poor prognostic sign.
|
With an inflammatory lesion in a non-lactating breast, or in a patient with no systemic disease or no history of trauma, you MUST rule out breast cancer
|
|
|
|
Breast implants
|
1. Are made of silicone or saline
2. Are used for augmentation or reconstruction after masectomy 3. There is NO reliable research to suggest that implants cause systemic disease 4. The body’s reaction to this foreign object is to illicit a granulomatous response 5. There are complications which include rupture, scarring, difficulty reading mammograms, and siliconoma (silicon leaks out of implant and forms a mass). |
|
|
|
Non-Proliferative Breast Disease (no increased cancer risk)
|
Fibrocystic change (FCC)
|
|
|
|
Fibrocystic change (FCC)
|
1. Extremely common finding amongst reproductive age women (25-45 years old).
2. Associated with drinking coffee 3. Clinically have ‘lumpy bumpy’ breasts; usually bilateral 4. Etiology is through an increased estrogen : progesterone ratio 5. No increased risk for cancer development because FCC is a non-proliferative condition. 6. Grossly, you would see firm, cystic masses (blue dome cysts) a. Histologically, you would see dense fibrosis (‘fibro’) and cysts (‘cystic’). b. Cysts are apocrine-lined and look like sweat glands. c. There is also some calcification present (appears dark purple). |
|
|
|
Proliferative Breast Disease
|
1. Sclerosing adenosis
2. Radial scar 3. Epithelial hyperplasia *** When a proliferative disease is diagnosed there is now an increased risk of cancer development *** |
|
|
|
Sclerosing adenosis
|
1. Affects younger women
2. Histological findings: i. Sclerosis--- scarring or fibrosis that compresses ductules ii. There is more fibrosis and ductal compression in the center of the lesion iii. In the periphery the ducts and glands are more open. iv. The lesion takes on an overall swirling pattern v. Adenosis, or proliferating glands, is also present. vi. Calcification and density on mammogram 4. **Cancer risk: 1.5-2x** |
|
|
|
Radial Scar
|
1. Central stellate scar or “flower head” appearance
2. Center of this lesion is an actual scar; center of sclerosing adenosis is compressed ducts 3. Mammographic density without calcifications--- LYNs 4. **Cancer risk: 1.5-2x** |
|
|
|
Epithelial Hyperplasia
|
1. Ductal epithelium proliferation that is greater than two cell layers thick
i. Moderate-florid = >4 cells thick ii. Must be past 4 cell layers thick to increase the risk for carcinoma 2. **Cancer risk ranges from 1.5-5x** 3. Classification i. Typical hyperplasia ii. Atypical hyperplasia |
|
|
|
Fat Necrosis
|
1. Clinical presentation is very ominous; however, fat necrosis is not malignant.
a. There is thickening and retraction of the skin overlying the fat necrosis. b. Painless mass; pain is usually associated with –itis and cancerous masses are usually painless 2. Fat necrosis tends to be found in patients with a history of trauma or a previous surgery. 3. The lesion appears grossly as a mass with ‘chalky flecks of calcification’ 4. Histologically, you see fat necrosis, PMN’s followed by lymphocytes and fibrosis. |
|
|
|
The lesion is most likely not cancer, if one of the following is true
|
1. The patient has inflammatory signs and is lactating
2. The patient has diabetes, sarcoidosis, thryoiditis, or some systemic disease 3. The lesion is painless and the patient has a history of minor trauma (ex. hit steering wheel during car accident) or previous surgery. Think fat necrosis here. |
|
|
|
Inflammation with breast cancer is a poor prognostic sign.
|
With an inflammatory lesion in a non-lactating breast, or in a patient with no systemic disease or no history of trauma, you MUST rule out breast cancer
|
|
|
|
Breast implants
|
1. Are made of silicone or saline
2. Are used for augmentation or reconstruction after masectomy 3. There is NO reliable research to suggest that implants cause systemic disease 4. The body’s reaction to this foreign object is to illicit a granulomatous response 5. There are complications which include rupture, scarring, difficulty reading mammograms, and siliconoma (silicon leaks out of implant and forms a mass). |
|
|
|
Non-Proliferative Breast Disease (no increased cancer risk)
|
Fibrocystic change (FCC)
|
|
|
|
Fibrocystic change (FCC)
|
1. Extremely common finding amongst reproductive age women (25-45 years old).
2. Associated with drinking coffee 3. Clinically have ‘lumpy bumpy’ breasts; usually bilateral 4. Etiology is through an increased estrogen : progesterone ratio 5. No increased risk for cancer development because FCC is a non-proliferative condition. 6. Grossly, you would see firm, cystic masses (blue dome cysts) a. Histologically, you would see dense fibrosis (‘fibro’) and cysts (‘cystic’). b. Cysts are apocrine-lined and look like sweat glands. c. There is also some calcification present (appears dark purple). |
|
|
|
Proliferative Breast Disease
|
1. Sclerosing adenosis
2. Radial scar 3. Epithelial hyperplasia *** When a proliferative disease is diagnosed there is now an increased risk of cancer development *** |
|
|
|
Sclerosing adenosis
|
1. Affects younger women
2. Histological findings: i. Sclerosis--- scarring or fibrosis that compresses ductules ii. There is more fibrosis and ductal compression in the center of the lesion iii. In the periphery the ducts and glands are more open. iv. The lesion takes on an overall swirling pattern v. Adenosis, or proliferating glands, is also present. vi. Calcification and density on mammogram 4. **Cancer risk: 1.5-2x** |
|
|
|
Radial Scar
|
1. Central stellate scar or “flower head” appearance
2. Center of this lesion is an actual scar; center of sclerosing adenosis is compressed ducts 3. Mammographic density without calcifications--- LYNs 4. **Cancer risk: 1.5-2x** |
|
|
|
Epithelial Hyperplasia
|
1. Ductal epithelium proliferation that is greater than two cell layers thick
i. Moderate-florid = >4 cells thick ii. Must be past 4 cell layers thick to increase the risk for carcinoma 2. **Cancer risk ranges from 1.5-5x** 3. Classification i. Typical hyperplasia ii. Atypical hyperplasia |
|
|
|
typical hyperplasia
|
• Heterogenous population of cells
• Irregular, peripheral fenestra • **Cancer risk 1.5-2x** |
|
|
|
atypical hyperplasia
|
• 15% of breast biopsies
• Atypical features: monomorphous cells; round, punched out fenestra • **Cancer risk: 4-5x** |
|
|
|
Benign Breast Tumors
|
1. Papillomas
2. Fibroadenoma 3. Phyllodes tumor -- often compared with fibroadenomas |
|
|
|
Papillomas
|
1. Typically affects women 40-50 yrs of age
2. Patient classically presents with bloody nipple discharge 3. Histologically, you would see a papillary proliferation with a broad-based ‘stalk’ i. Torsion of this stalk results in the bloody discharge 4. **Cancer risk: 1.5-2x** i. Might be considered a proliferative breast lesion because it is associated with increased cancer risks. There is still some debate as whether or not the lesion is truly clonal. |
|
|
|
Fibroadenoma
|
1. #1 benign breast neoplasm
2. Stromal tumor--- the neoplastic part of the tissue is the fibrosis or stromal component (‘fibro’) not the glandular (‘adenoma’) component 3. Primarily affects reproductive age women 4. Can be multiple and/or bilateral 5. Hormonally responsive and cyclic in nature i. Changes with menstrual cycle ii. Grows during pregnancy and lactation iii. Regresses after menopause 6. During physical exam the lesion is: i. Freely movable; ‘like a marble’ and not adherent to the chest wall. ii. Size can range from 1cm to very large iii. Rubbery; Gray-white in color; and sharply circumscribed iv. Grossly, there are slit-like spaces in the lesion 6. Histologically, the stroma appears loose and myxoid and the glands are compressed into slits. i. Remember that the neoplastic portion is the surrounding stroma and it impinges on the glands. 7. Fibroadenomas appear dense on mammograms and are not associated with an increased cancer risk. |
|
|
|
Phyllodes tumor
|
1. Like fribroadenomas, they are hormonally responsive stromal tumors
2. Are associated with an older age of onset (occurs usually in 60’s) 3. Carry a 15-20% risk of cancer 4. Treated with wide excision because of risk of local recurrence 5. Malignant phyllodes tumors can metastasize 6. Grossly they look just like fibroadenomas. i. Size can vary from 1cm to very large ii. Gray-white iii. Slit-like spaces 7. Histology is used to differentiate the two lesions. i. Phyllodes tumors have a more cellular stroma with visible mitoses and pleomorphism. ii. More stromal proliferation leads to marked glandular compression |
|
|
|
Breast cancer
|
1. #1 malignancy in women
2. Women have a 1 in 8 chance of having breast cancer by the age of 90 (so a baseline lifetime risk of ~11%). 3. The number of women with breast cancer will increase by 1/3 in next 20 years. 1. However, this apparent increased incidence may be explained by the influence of better mammographic screening. |
|
|
|
Breask cancer Risk factors
|
1. Age is one of the biggest risk factors for breast cancer.
a. The average age of a woman with breast cancer is 64 years old. b. According to a 2004 NEJM study, the risk at 30 years old is 3.2%, while the risk at 70 years old is 85%. 2. Hormones also play an important role. a. If a woman had her first menses before the age of 11, her lifetime risk of breast cancer is increased by 20%. b. If a woman has her first child before 20 years of age, her risk is decreased by 50%. - Having multiple children also decreases the risk. c. So, a woman who is nulliparous and menstruated early has the highest risk. 3. Women with a 1st degree affected relative (i.e. mother or sister) have a 4-5 times higher baseline risk. a. Note that having an affected relative does not mean the cancer is hereditary/familial. 4. Proliferative breast disease (see Path C3) increases the risk 1.5 – 5 times. a. Epithelial hyperplasia of atypical type is the one that increases the risk 5-fold. 5. White women tend to have a higher breast cancer incidence than black women; however, cancer in black women generally is more advanced and carries a higher mortality. 6. The major risk factors for breast cancer are hormones, genetics, and age |
|
|
|
Familial Breast Cancer
|
1. True familial breast cancer is rare (< 15% of the time is a known gene to blame).
2. 25% of familial cases are due to the infamous BRCA genes (BRCA1 & 2), which is only 3% of breast cancers overall. a. Indicators include multiple affected relatives, premenopausal cancer, male breast cancer, and ovarian cancer in the family. 3. 10% of familial cases are due to other known genes. a. These include CHEK2, p53 (Li-Fraumeni syndrome), PTEN (Cowden syndrome), LKB1 (Peutz-Jegher), ATM (Ataxia-telengectasia). 4. The majority (~2/3) of familial cases are due to a gene that has not yet been identified and thus cannot be tested for. |
|
|
|
BRCA1
|
1. Chromosome 17q
2. More common 3. >500 known mutations 4. Younger (40-50y) 5. Associations: – Ashkenazi Jewish – Medullary type CA – Mucinous type CA – CA of colon, prostate, pancreas – More ovarian CA (30%) |
|
|
|
BRCA2
|
1. Chromosome 13q
2. Less common 3. >300 known mutations 4. Older (50yrs) 5. Associations: – Male breast CA – CA of colon, prostate, pancreas – Melanoma and gastric CA – Less ovarian (15%) |
|
|
|
BRCA1 and BRCA2 mutations
|
impart a lifetime risk for breast cancer of 60-80%
the gene doesn't show complete penetrance |
|
|
|
Breast Lesions
|
1. Most breast complaints are ultimately found to be benign, especially those with nipple discharge (usually associated with a papilloma) or in a woman < 50 years of age.
a. The chief complaints suggestive of a benign tumor are a ‘lumpy bumpy’ texture (fibrocystic change) and pain. b. The chief complaint suggestive of malignancy is a discrete palpable mass. 2. 60% of palpable breast masses in a woman > 50 years of age are malignant. a. If the lesion is first detected mammographically, the risk is 40%. 3. Therefore, the clinical scenario most likely to be breast cancer is a woman over 50 with a palpable mass and a lesion present on mammaogram. |
|
|
|
Detecting Breast Cancer
|
1. Clinical Breast Exam (CBE)
2. Breast Imaging [ 3. Pathology Diagnostics |
|
|
|
Clinical Breast Exam (CBE)
|
1. The CBE includes a monthly self-exam as well as a yearly physician exam.
a. Self-exams should be performed within 7 days after cessation of menses each month. 2. The average size of a mass found by a woman who does not examine herself monthly is 4 cm, whereas a mass of 2 cm may be found by a woman who examines monthly (practice makes perfect!). a. A skilled physician may be able to detect a mass as small as 1 cm. b. The average size mass found by mammogram is 0.5 cm. 3. Most breast cancer is in the upper outer quadrant (UOQ) and is in the left breast (remember that gynecomastia also has a left-breast preference). |
|
|
|
Breast Imaging
|
1. Women should have yearly mammograms beginning at 40 years of age (or before if there is a positive family history).
a. Some insurance companies encourage women to get a mammogram at age 35 to serve as a normal baseline against which future mammograms can be compared. 2. A screening mammogram takes pictures of the breast at 2 angles, and the results are returned within a few days. (very quick) 3. A diagnostic mammogram uses > 2 views and interpretation is immediate. a. This type of mammography is used if a screening mammogram is positive or if the patient has breast implants. (get info that day) 4. Radiologists report mammogram results as a BI RADS score (we don’t need to know the specifics of this), where a higher score signifies a more dismal prognosis. 5. Emerging methods include ultrasound (indicated when a cyst is suspected), MRI, CT, and PET scans. |
|
|
|
Pathology Diagnostics
|
1. Fine Needle Aspiration
2. Core Needle Biopsy 3. An emerging method that we may use more of in the future is ductal lavage. |
|
|
|
Fine Needle Aspiration
|
1. This technique uses a 20-25 gauge needle to remove a small aspirate of cells from a palpable breast mass.
i. Generally, a cytopathologist will both do the procedure and interpret the results on site. 2. It is a bedside, office procedure that requires no anesthetic. |
|
|
|
Core Needle Biopsy
|
1. A very large (small gauge) needle is used to remove 6-10 cores of tissue from the breast under local anesthesia.
2. This procedure must be done by a surgeon and sent to a pathologist for interpretation. |
|
|
|
Diagnostic Algorithm and Detection Success
|
1. The “Triple Test” for palpable lesions
2. The test is positive if any of the components is suspicious. 3. The test is negative only if all 3 components are negative, and the negative predictive value is ≥ 99%. 4. Overall, detection rates are improving, which explains the apparent increasing incidence of breast cancer. 5. Detection for low grade/stage tumors is specifically improving, so there has been a rise in in situ and Stage I disease. a. As a result of this earlier detection, mortality is decreasing; however, 20% of women who are affected will die of their disease. |
|
|
|
The “Triple Test” for palpable lesions is
|
1. CBE
2. Diagnostic mammogram 3. Fine Needle Aspiration (FNA) |
|
|
|
Prognosis upon breast cancer detection is determined by a compilation of several factors
|
1. Type of tumor
2. Grade / stage of tumor 3. Spread to axillary lymph nodes 4. Distant metastasis 5. Tumor size 6. Presence of inflammation (poorer prognosis) a. Peau d’orange—a swelling of the breast with skin thickening—is indicative of active inflammation. (While this sign is often emphasized to med students, Dr. McGoey has never seen an actual case where peau d’orange was present.) b. Always keep cancer in your differential when a woman presents with breast inflammation. 7. Estrogen and progesterone tumor receptors (ER / PR) 8. Tumor protooncogene (Her2Neu) |
|
|
|
Tumor Stains
|
1. ER/PR
2. Her2Neu |
|
|
|
ER/PR
|
• Immunohistochemical (IHC) stain
• Detects hormone receptor • 50-70% tumors stain positive • Better prognosis if positive • Therapy: Tamoxifen |
|
|
|
Her2Neu
|
• IHC stain and FISH
• Detects protooncogene • 20-30% tumors overexpress Her2Neu • Worse prognosis if positive • Therapy: Herceptin |
|
|
|
Histology of Breast Cancer
|
A. The #1 type of malignancy found in the breast is adenocarcinoma (95% of cases).
1. All adenocarcinoma arises in the TDLU (terminal duct lobular unit). B. Patterns 1. In situ vs. invasive a. In situ tumors are limited by the basement membrane of the TDLU. b. Invasive tumors infiltrate past the basement membrane and have the capacity to metastasize. 2. Ductal vs. lobular a. These are pattern descriptors only; they do not specify a certain type of carcinoma. |
|
|
|
Dr. McGoey’s “80-20 Rule
|
1. Generally, 80% of breast cancers are invasive, while 20% are in situ.
a. Of the 80% that are invasive, 80% are ductal, while 20% are lobular. b. Of the 20% that are in situ, 80% are ductal, while 20% are lobular. |
|
|
|
In Situ Breast Carcinoma
|
1. Ductal Carcinoma in situ
2. Lobular carcinoma in situ |
|
|
|
Ductal Carcinoma in situ (DCIS)
|
1 Women of older age
2 Stains positive for E-cadherin 3 Types – Comedo – Noncomedo – Paget’s |
|
|
|
Lobular Carcinoma in situ (LCIS)
|
1 Women of younger age
2 Stains negative for E-cadherin 3 No specific types 4 > 30% is bilateral |
|
|
|
Comedo DCIS
|
composed of ducts filled with pleomorphic cells and central necrosis
|
|
|
|
Noncomedo DCIS
|
can be further divided into
1. solid, 2. cribriform, 3. papillary, and 4. micropapillary |
|
|
|
Paget’s disease
|
1. characterized by a spreading of the tumor out of the TDLU and onto the surface of the nipple.
2. It presents as a pruritic, scaly, dry, erythematous plaque over the areola. 3. About ½ of patients have a palpable mass. 4. Histologically, clear cells (Paget cells) are seen in the epidermis and along the epidermal-dermal junction. (NT note: She hinted that 2nd year med students should be able to identify the clear cells shown in the H&E stain on Slide 54 as Paget cells.) 5. Even though it is considered a DCIS, > 90% of Paget patients have an invasive carcinoma component to the tumor. (so the physician goes back and looks again) |
|
|
|
LCIS
|
1. comprised of monomorphic cells and maintains a lobular architecture.
2. Remember, these tumors stain negative for E-cadherin, as is depicted by the absence of brown color in the picture on the right of slide 55 (she repeated the staining characteristics several times). |
|
|
|
Invasive Breast Carcinoma
|
1. Is adenocarcinoma 95% of the time.
a. Just as with in situ, lobular and ductal are pattern descriptors and not special types of tumors. - Again, a lobular invasive carcinoma is more likely to be bilateral than a ductal one. 2. Grossly, these tumors present as a hard, gritty, spiculated mass. 3. They are graded by pathologists with a Bloom-Richardson score (as opposed to BI RADS, which are assigned by radiologists). |
|
|
|
Bloom-Richardson score
|
1. This system is comprised of 3 morphological components, each worth 1-3 points:
a. Tubule formation b. Nuclear Grade / Pleomorphism c. Mitoses 2. Score of 3-5 = Grade I (best) 3. Score of 6-7 = Grade II 4. Score of 8-9 = Grade III (worst) a. All we really need to know is that a higher score indicates a higher grade tumor, which indicates a poorer prognosis. |
|
|
|
Ductal carcinomas
|
1. obviously malignant histologically (Slide 60).
2. They show hyperchromasia, desmoplasia, pleomorphic cells, and infiltrating glands |
|
|
|
Lobular carcinomas
|
1. don’t look nearly as aberrant.
2. The key with lobular is to look for signet ring cells (bottom left on Slide 61) and Indian filing (the way that the tumor cells arrange themselves in lines – left and middle picture on Slide 61). 3. Remember the negative E-cadherin stain for lobular! |
|
|
|
Types of Invasive Ductal Carcinoma
|
1. tubular
2. mucinous (colloid) 3. Medullary A. These special types are rare, but they carry a prognosis three times better than ductal CA-NST (NST = no special type). B. The tubular type appears very glandular and innocent looking, the mucinous type is mucin with tumor cells floating in it, and the medullary type has pleomorphic and lymphoplasmacytic cells. 1. The medullary variant “looks so bad it can’t be cancer.” |
|
|
|
Tubular Invasive Ductal Carcinoma
|
1 #1 variant
2 Younger (40s) 3 Excellent prognosis 4 10-40% bilateral |
|
|
|
Mucinous (colloid) Invasive Ductal Carcinoma
|
1 Elderly
2 Better prognosis 3 Associated with BRCA1 4 Circumscribed, soft |
|
|
|
Medullary Invasive Ductal Carcinoma
|
1 Younger (40s)
2 Better prognosis 3 Assoc with BRCA1 4 Circumscribed |
|
|
|
Non - Carcinoma Breast Malignancies
|
1. These are rare, making up < 5% of breast malignancies.
2. Types a. Sarcomas b. Lymphomas |
|
|
|
Sarcomas
|
1. These have the potential for hematogenous spread to the lungs.
2. The risk for breast angiosarcoma is increased after radiation therapy to that region, and the risk for angiosarcoma in the arms is increased after mastectomy. a. Stewart-Treves syndrome - The classic case will be a woman who shows up in the clinic with a lesion on her arm 20-30 years post-mastectomy. The lesion will be an angiosarcoma, and this phenomenon is known as Stewart-Treves syndrome. |
|
|
|
Lymphomas
|
1. Diffuse large B cell
2. Burkitt |
|
|
|
Male Breast Cancer
|
1. Is quite rare (100 times less common than in females).
2. It has similar risk factors to those seen in females. a. 5-10% are due to BRCA2 mutations. b. 3-5% are found in association with Klinefelter syndrome. c. Interestingly, gynecomastia does not increase the risk for breast cancer. 3. It has histologic patterns that are similar to those in females. a. Again, the lobular pattern is less common. b. There is greater ER (estrogen receptor) positivity in males than females. 4. If you age and stage match between breast cancer in a male and in a female, they have the same prognosis; however, breast cancer in men is often discovered much later. |
|
|
|
When Kidney's malfunction
|
1. edema
2. acidosis 3. hyperkalemia |
|
|
|
can cause secondary hyperthyroidism
|
1. hyperphosphatemia
2. hypocalcemia *** kidney involved with calcium and phosphorous metabolism |
Kidney get rid of positive but keep negative....
K mart tanked... so it likes negatives. |
|
|
erythropoietin
|
1. made by kidneys
2. stimulates RBC production 3.thus malfunction of kidneys can produce anemia |
|
|
|
Kidney malfunction can have these effects.
|
1. fluid and electrolyte imbalance
2. hematological manifestions 3. hyper calcium and phosphorous 4. cardiovascular effects 5. GI tract abnormalities 6. Neurologic 7. Skin |
|
|
|
Cardiovascular Effects
|
*** because it deals with fluid balances and intravascular volume.
1. Increased fluid load due to renal insufficiency leads to hypertension (resulting in CHF) and overt uremia (excess urea and nitrogenous wastes in the blood). 2. With uremia, you can get friction rub in the pericardium and classically present with uremic pericarditis. |
|
|
|
GI tract abnormalities
|
nausea, vomiting, diarrhea
|
|
|
|
Neurologic effects of kidney malfunction
|
peripheral neuropathy, myopathy
|
|
|
|
Skin
|
sallow (yellowish) color and pruritus
|
|
|
|
Acute nephritic syndrome
|
refers to a group of disease where the chief presenting symptom is hematuria
|
|
|
|
Nephrotic syndrome
|
1. Renal abnormality is manifested by severe amounts of proteinuria.
2. Rv note: May not see any color changes in the urine, therefore may present with chronic damage initially) |
|
|
|
Asymptomatic hematuria (microhematuria) or proteinuria
|
Microhematuria: hematuria not sufficient enough to make the urine look red
|
|
|
|
Acute renal failure
|
1. Azotemia – This is a group of biochemical abnormalities where your kidneys aren’t working enough to clear blood urea nitrogen (BUN) and creatinine. But there are no clinical symptoms yet.
|
|
|
|
Chronic renal failure
|
1. Uremia – This is when you have acute renal failure (the biochemical abnormalities seen in azotemia) accompanied with the clinical manifestations mentioned above (GI tract abnormalities, edema, anemia, pericarditis, etc).
|
|
|
|
Renal tubular defects
|
These can lead to
1. acid-base problems 2. as well as urine concentrating problems. |
|
|
|
Urinary tract infection
|
infectious and inflammatory condition that can affect the renal system
|
|
|
|
Nephrolithiasis
|
kidney stones
|
|
|
|
Urinary tract obstruction
|
the cardinal sign is the sudden cessation of any urine output (anuria) due do an obstruction.
|
|
|
|
Clinical Manifestions of Kidney Failure
|
1. Acute nephritic syndrome
2. Nephrotic syndrome 3. Asymptomatic hematuria (microhematuria) or proteinuria 4. Acute renal failure 5. Chronic renal failure 6. Renal tubular defects 7. Urinary tract infection 8. Nephrolithiasis 9. Urinary tract obstruction |
|
|
|
Kidney failure Histological Manifestations
|
1. Glomeruli Manifestations
2. Vessels can undergo arteriolosclerosis, vasculitis, and thrombosis. 3. Tubules Manifestations 4. Interstitium (“the stuff that’s in between and holds everything together”) can have inflammatory infiltrate, edema, and fibrosis |
|
|
|
Glomeruli Manifestations
|
1. Hypercellularity
2. Hyalinization 3. Sclerosis 4, Changes of the glomerular basement membrane (GBM) |
|
|
|
Hypercellularity
|
1. (proliferative reaction) of three cells of the glomerulus:
a. mesangial cells, b. endothelial cells, c. and epithelial cells. 2. Also, infiltration of inflammatory cells. |
|
|
|
Hyalinization
|
accumulation of acellular, amorphous, eosinophilic material.
|
|
|
|
Sclerosis
|
When the glomeruli lose their functional capability, they are replaced by collagenous/hyalinized material.
|
|
|
|
Changes of the glomerular basement membrane (GBM)
|
The GBM can get
1. thin, 2. get thick, 3. split, 4. accumulate deposits, etc. |
|
|
|
Tubules can undergo
|
1. Necrosis (b/c lined by epithelial cells)
2. Atrophy a. If you have sclerotic changes of the glomerulus, it can become nonfunctional and stop filtration. The tubules drop-out and undergo atrophy. 3. Neoplasia |
|
|
|
Pathogenesis of Glomerular Disease
|
1. Immune complexes
2. Antiglomerular basement membrane antibodies 3. Complement activation 4. Cellular activation 5. Cytokine synthesis/release 6. Glomerulosclerosis (FSGS) and tubulointerstitial damage (atrophy and fibrosis) 7. Glomerular disease |
|
|
|
Immunne Complexes
|
1. About 75% of glomerular diseases are immunologically-mediated- primarily involving immune complexes (Type III hypersensitivity).
2. An antigen can get deposited in the GBM; antibodies attach and make antigen-antibody complexes in-situ. 3. Or there are also circulating Ag-Ab complexes that can be deposited on the GBM. 4. The immune complexes can be subepithelial [12] or intramembranous [13] (Subepithelial can progress to intramembranous). |
|
|
|
Antiglomerular basement membrane antibodies
|
1. In an autoimmune disease, you can make autoantibodies that attach to components of the GBM or glomerular cells.
2. May not necessarily form a complex, but may be more insidious. 3. Can detect with immunofluorescence. |
|
|
|
Complement activation
|
Deposited Ab’s can bind and activate complement
|
|
|
|
Cellular activation
|
neutrophils, macrophages, platelets) – The hydrolytic enzymes from the neutrophils will be released, then digest the GBM and form holes. This allows RBCs to leak into the tubules and cause hematuria.
|
|
|
|
Glomerulosclerosis (FSGS) and tubulointerstitial damage (atrophy and fibrosis)
|
1. Glomerular damage results in scarring.
2. This healing and repair process results in a loss of function. 3. Once you get glomerulosclerosis, the glomerulus will not work again, and consequently results in atrophy and fibrosis because the rest of the tubule drops out as well. |
|
|
|
Glomerular disease – Immunofluorescence (FM) of the basement membrane
|
1. If antibodies attach directly to the GBM (e.g., autoimmune), you can get this immunofluorescence pattern. The antibody is uniformly distributed all along the GBM, and there is a very smooth, thin, ribbon-like deposit of immunofluorescence.
2. If antibody-antigen complexes get deposited in the GBM, it results in a more granular and dense appearance (“chunky bumpy”). This image has so many deposits that it resulted in an almost continuous immunofluorescent pattern all around. (“String of pearls appearance”) |
|
|
|
Acute Nephritic Syndrome (Acute Glomerulonephritis)
|
1. ***The predominant clinical presenting sign is hematuria (blood in the urine)*** [17].
2. Acute refers to the quick onset of symptoms. 3. Glomerular hypercellularity (inflammation and/or glomerular cell proliferation) 4. Usually as a rough rule of thumb, when you see hematuria and hypercellular changes in the glomeruli, think acute glomerulonephritis. 5. ***Red blood cell casts in urine 6. Because the glomerulus is hypercellular, the rate of blood flow going through is inhibited. |
|
|
|
3. Glomerular hypercellularity (inflammation and/or glomerular cell proliferation)
|
1. Glomerulus exceeds 200 cells.
2. This could be a proliferation of endothelial cells, epithelial cells, or mesangial cells. 3. This could be an infiltration of neutrophils or other inflammatory cells that are extraneous to the native cells present in the glomerulus. |
|
|
|
***Red blood cell casts in urine (Rv note: Casts = Aggregates of RBCs that form within the nephron unit)
|
1. As red blood cells get into the tubules of the nephron, they become meshed in a secreted protein that serves as a gel for the RBCs to become embedded in. This forms a cylindrical cast of RBCs that mimics the width and shape of the tubule, so when that nephron opens up and urine begins to flow through it, that cast/plug is flushed out. In a urinalysis, you can find these sausage-shaped segments.
2. ***RBC casts in the urine is diagnostic of a disease in kidneys (upper urinary tract). Casts cannot form in any other part of the urinary tract. *** |
|
|
|
Because the glomerulus is hypercellular, the rate of blood flow going through is inhibited
|
1. Azotemia results due to ineffective filtration.
2. Oliguria is decreased urine output. 3. Hypertension |
|
|
|
Nephritic syndrome disorders
|
1. Acute Proliferative Glomerulonephritis (Postinfectious/Poststreptococcal)
2. Rapidly Progressive Glomerulonephritis (RPGN) 3. IgA Glomerulonephritis 4. Benign Recurrent Hematuria 5. Hereditary [ |
HAIR B
|
|
|
Acute Proliferative Glomerulonephritis (Postinfectious/Poststreptococcal)
|
1. This is a proliferation of endothelial cells and inflammatory change in the glomeruli. It has an acute onset.
2. It predominantly occurs in the pediatric age group but can occur at any age. 3. This is one of the poststreptococcal sequelae (but can occur with other bacteria as well) i. This occurs 1 to 4 weeks after acute infection (pharyngeal or skin) so the urine is sterile (i.e. no bacteria). This is a delayed immunologic reaction that results in antibodies to streptococcal antigens, which form immune complexes, and remnant complexes end up in the glomeruli. ii. Non-infectious, immunologically mediated 4. Immune complexes are deposited sub-epithelially. 5. Low serum complement- complement is activated so serum levels are low 6. Treatment: for the most part is supportive because this disorder is self-limiting. Immune complexes will eventually degrade. Antibiotics will be useless because there are no bacteria. |
|
|
|
Acute Proliferative Glomerulonephritis (Postinfectious/Poststreptococcal) - Microscopic findings
|
1. H&E stain [Slide 20]: You cannot see glomerular capillary loops because they’re plugged up by the hypercellular and swollen endothelial cells (proliferative changes). Note the neutrophilic infiltrate and the increase in number of cells (black dots).
2. H&E stain [Slide 21]: This is another image showing the swollen, hypercellular, diffuse proliferative type of glomerular lesion. (Rv note; Diffuse because every glomerulus in the tissue looks like this.) 3. Immunofluorescent microscopy (FM) [Slide 22]: There are “chunky bumpy” bits of immune complexes scattered throughout the GBM. 4. Electron microscopy (EM) [Slide 23]: There are huge, subepithelial lumpy deposits (due to immune complex deposition) that are scattered on the epithelial side of the GBM. |
|
|
|
Acute Proliferative Glomerulonephritis (Postinfectious/Poststreptococcal) - prognosis
|
1. Pediatric – for the most part this is an acute episode and their renal function does not get severely impaired.
2. Adults – prognosis is more variable. You may have some persistence and loss of renal function, and rarely some may go into chronic renal failure. For the most part, this is not a bad renal disease to have. |
|
|
|
Rapidly Progressive Glomerulonephritis (RPGN)
|
1. Aka crescentic glomerulonephritis
2. The hallmark feature is the presence of epithelial cell proliferation that fills in Bowman’s space and forms crescents. The glomerulus is a little shrunken and compressed due to the epithelial cell proliferation. 3. Very acute onset, these patients’ renal function will deteriorate right in front of you from morning to evening. 4. There 3 types and they all clinically look identical and are managed the same. But they have distinguishable morphologic features that are used in pathology: 5. H&E stain [Slide 26]: You have small glomeruli, and the rest of it is made up of the proliferation of epithelial cells. There is a lot of interstitial edema. The key here is to see the crescent space of the glomeruli. 6. EM images are non-contributory, because mostly just looking for proliferation in Bowman’s space. [28] 7. Treatment for the most part is supportive. 8. Prognosis: long term prognosis is poor. The patient may need a transplant, but it may not be appropriate because you can still have antibodies floating around. This is a difficult management problem- may need chronic dialysis. |
|
|
|
Rapidly Progressive Glomerulonephritis (RPGN) - type 1
|
1. an idiopathic or autoimmune disease with anti-GBM antibodies that attaches to both the GBM and to the alveolar capillary basement membrane (Goodpasture’s syndrome) producing hemoptosis and hematuria. So you have a loss of both pulmonary and renal function. There are no discrete dense deposits.
2. does not involve circulating soluble immune complexes, so you will not see the “chunky bumpy” appearance in FM. With type I, you’ll see a smooth, homogenous, linear, ribbon-like deposit. |
|
|
|
Rapidly Progressive Glomerulonephritis (RPGN) - type 2
|
1. can be associated with
a. a postinfectious disease, b. systemic lupus erythematosus (SLE), c. Henoch-Schölein Purpura (HSP) d. or idiopathic. 2. It is immune complex mediated |
|
|
|
Rapidly Progressive Glomerulonephritis (RPGN) - type 3
|
1. least common,
2. associated with anti-neutrophil cytoplasmic antibodies (ANCA) 3. and has relatively few immune complex deposits (Pauci-immune). |
|
|
|
Rapidly Progressive Glomerulonephritis (RPGN) - treatment
|
i. If there are circulating immune complexes like in type II, you can do plasmapheresis (filter out the immune complexes from the blood and put clean blood back into the pt)
ii. Steroids have had some success as an anti-inflammatory agent. |
|
|
|
IgA Glomerulonephritis
|
1. Aka Berger’s disease
2. This condition is unique in that you have mesangial cell hypercellularity and IgA immune complexes deposited in the mesangials. (no crescents, no PMNs) 3. This is characterized by exacerbation and remissions of hematuria. 4. This is a relatively common condition. These need to be identified and recognized because long term prognosis is not particularly good. 5. IgA deposits can also be seen in SLE and Henoch-Schölein Purpura (HSP). |
|
|
|
IgA Glomerulonephritis - microscopic findings
|
1. H&E stain [Slide 31]: The glomeruli from this magnification do not look too bad. It’s hard to see how wide the mesangial cells are.
2. H&E stain [Slide 32]: At higher magnification, you can see how much wider the mesangium is. This glomerulus shows an increased number of mesangial nuclei (a little hard to see) due to hypercellularity. The GBM is not as thin and delicate as normal. 3. *FM [Slide 33]: This displays a unique pattern. The deposits are in the mesangium. This looks like a tree in winter where all the leaves are gone, staining only the limbs. 4. EM [Slide 34]: This confirms what you’ve seen already. There is a prominent mesangial cell nucleus and mesangium. There are deposits within the mesangium ***(LYN)NT Note: So far we’ve seen three different FM patterns: 1) smooth, linear, ribbon-like staining of GBM (autoimmunity against GBM), 2) “chunky bumpy” granular immune complex deposition diseases, and 3) the unique tree-like pattern in IgA glomerulonephritis. The IgA tree-like pattern is pathognomonic for IgA GN, so I’d know it.*** |
|
|
|
IgA Glomerulonephritis - treatment and prognosis
|
1. Treatment: mostly supportive; it’s important to counsel the patient and let them know that this disease does not have a good prognosis.
2. Prognosis: poor; this is a progressive disease (will eventually get sclerotic, non functional glomeruli) and will recur after transplants. |
|
|
|
Benign Recurrent Hematuria
|
1. All other glomerular disease must be ruled out before this diagnosis is made (diagnosis of exclusion).
2. There are no histologic abnormalities. Renal function and kidney is fine. ‘These patients just happen to pee blood every once in a while.’ Often seen in athletes due to trauma. |
|
|
|
Hereditary
|
1. This heterogenous group of diseases is not common.
2. This can be characterized by recurrent bouts of hematuria. 3. Types a. Alport syndrome: b. Benign familial hematuria: |
|
|
|
Alport syndrome
|
i. Eye disorders, hearing problems, albinism.
ii. Male predominance; usually a family history. iii. Irregular thickening and lamination (‘basket weave look’) in the GBM (trabecular changes). iv. Nephrotic syndrome may develop and proteinuria can occur. v. Rv note: NO immune complexes b/c NOT immune mediated because it is hereditary! |
Alport... like albinisim... male predominancy
Thickening and lamination of GBM alpOrt = nephrOtic syndrome |
|
|
Benign familial hematuria
|
i. This is unique in that these patients have a thin GBM, which is seen on EM (distinguishes from benign recurrent). Clinically, probably not too different from benign recurrent, but in this case, patients will need to know they have the hereditary form to inform their children.
ii. Prognosis: good; this is not progressive and will not impact or reduce your lifespan. |
|
|
|
Nephrotic Syndrome
Characteristics |
1. Massive proteinuria (>3.0 gm/24hrs) – The significant amount of protein reduces the surface tension in your urine so you get lots of foaming bubbles.
a. Normally you’re supposed to lose less than 150 mg of protein/24 hrs. It takes a lot of work to make proteins so your body does not want to lose them. 2. Hypoalbuminemia – Proteinuria leads to depletion of serum albumin levels. The liver can’t keep up with its albumin synthesis. 3. Generalized edema –Hypoalbuminemia reduces colloid osmotic pressure, leading to edema. (Rv note: Edema is more prominent in the dependent portions due to gravity.) 4. Hyperlipidemia – Because the body can’t keep up through protein production, the body tries to restore osmotic pressure by building lipoproteins. Does not have athlerosclerotic potential but is a marker. 5. GBM changes - *need to use EM* 6. Usually little (if any) cellular proliferation 7. Rv note: Protein and GBM changes (think, thin, woven, and very little if any cellular proliferation) are KEY! |
|
|
|
Nephrotic Syndrome Disorders
|
1. Minimal Change disease [39] aka Nil Disease aka Lipoid nephrosis
2. Focal Segmental Glomerulosclerosis 3. Membranous Glomerulopathy |
|
|
|
Minimal Change disease aka Nil Disease aka Lipoid nephrosis
|
1. Predominantly a pediatric disease
i. Sample scenario: 5 year-old patient with 12g of protein loss – he/she has minimal change disease until proven otherwise. 2. Key clinical aspect is that there’s a dramatic response to steroids. The proteinuria stops and does not return. 3. This is associated with atopic disorders (eczema, rhinitis) and respiratory infections and immunization. 4. There are no immune complexes. 5. There are no changes to the GBM, BUT there are changes to the epithelial cells (the foot processes/podocytes). 6. Treatment: steroids 7. Prognosis: good |
minimal change shows a big change to steriods.
minimal = little... so it's predominantly kids |
|
|
Minimal Change disease aka Nil Disease aka Lipoid nephrosis - Microscopic findings
|
i. H&E stain [Slide 40]: no increase in cellularity, capillary lumens are nice and patent, GBM looks thin, delicate, and normal. This looks like a normal glomerulus.
ii. EM [Slides 41, 42]: The GBM looks smooth and uniform, but where are the foot processes? This condition displays effacement of foot processes (cell cytoplasm basically flattens out). But once the proteinuria stops (steroids), the foot processes return. • Basically every glomerular disease that has proteinuria will show flattened epithelium. But this is the only morphological change that takes place in minimal change disease. If there is some other abnormality, then it is not minimal change. iii. FM: negative- no immune complexes |
|
|
|
Focal Segmental Glomerulosclerosis
|
1. It’s focal because only some glomeruli in the kidney are affected. (If every glomeruli were affected, it would be termed diffuse.)
2. It’s segmental because only portions of the affected glomerulus are affected. (If the whole glomerulus was affected, it would be called global.) 3. It’s more prevalent in late adolescents and early adults. 4. It’s idiopathic or associated with HIV or other forms of focal glomerulonephritis. 5. This was once thought to be a subtype of minimal change disease (no deposits). i. The sclerosis separates this from minimal change disease 6. Non-selective proteinuria (many types of proteins, not just albumin in the urine) 7. A subset of patients may have some nephritic features such as hematuria. 8. Kidney biopsies: If you do a biopsy in a disease like this and you perform a kidney biopsy with only 3 glomeruli in it, sampling error can be an issue. i. You need at least 5-7 glomeruli to make a better judgment of the disease. |
it selects the segment... but not the protein in the urine!!!
|
|
|
Focal Segmental Glomerulosclerosis - microscopic findings
|
i. H&E stain [Slide 45]: The upper left glomerulus has lesions (darker pink, swollen areas) in the right-half of it. The upper right glomerulus has lesions in the upper right-half of it. Then the lower glomerulus has no sclerotic segments at all.
ii. H&E stain [Slide 46]: These are focal segmental lesions. Sometimes these sclerotic segments form little adhesions with the Bowman’s capsule called synechiae. iii. FM [Slide 47]: If you perform FM on these sclerotic segments, it can be positive because it can show immunoglobulin that’s been trapped in the sclerotic segment (in synechial lesion). But this is truly not immune complex deposition – it is just entrapment of protein. iv. EM: It is non-contributory. It shows effaced foot processes (like in minimal change disease) of epithelial cells and sclerotic segments. There isn’t anything distinguishing on here compared to the H&E. |
|
|
|
Focal Segmental Glomerulosclerosis - treatment and prognosis
|
1. Long term prognosis is NOT good because focal sclerotic segments do continue to expand and eventually globally involve the glomeruli.
2. This is also a diagnosis of exclusion to some extent, because there are other glomerular diseases that can give focal, sclerotic lesions, pathologists are called to the rescue. |
|
|
|
Membranous Glomerulopathy
|
1. *This is the most common cause of nephrotic syndrome in adults.*
2. Can be idiopathic or secondary (drugs, underlying malignancies, SLE, chronic infections with continuing antigenic load (TB, HBV, HCV, parasites), metabolic disorders (thyroiditis)) i. (Rv note: Can be associated with any chronic process – any time you have a bunch of immune complexes floating around.) 3. There is subepithelial immune complex deposition (like acute proliferative glomerulonephritis) and NO hypercellularity. 4. Treatment: If it’s a secondary disease (like TB or chronic hepatitis), then treat the underlying disease. Otherwise provide supportive care. Can try steroids. 5. Prognosis: highly variable – you cannot tell your patient how long they will stay in their condition. |
Membraneous... people remember it....so it's the most common cause of nephrotic syndrome disorders.
But you can't remember the prognosis = highly variable membranes are parts of cells.. not cells = no hypercellularity. |
|
|
Membranous Glomerulopathy - microscopic findings
|
i. H&E stain [Slide 51]: This is definitely not hypercellular – this is not a proliferative change. Capillary lumen is a little open. GBM may be a little thicker. It’s hard to tell the changes just based on the H&E.
ii. H&E stain – higher power [Slide 52]: The GBM looks a little thicker. There is no endothelial or epithelial proliferation. iii. *FM [Slide 53]: Every glomerulus lights up and has granular, non-continuous deposits in the GBM. iv. EM [Slide 54]: The deposits (dark things) are on the epithelial cell side of the capillary lumen. Note no increase in the number of cells |
|
|
|
Membranoproliferative glomerulonephritis (MPGN) (Crossover diseases)(Also Mesangial Capillary Glomerular Nephritis)
|
1. This disease has characteristics of both nephritic and nephrotic diseases.
a. There are proliferation changes and GBM changes. 2. Type I (66%) – This type has subendothelial deposits (these are located on the capillary side of the GBM). 3. Type II (33%) – This type has intramembranous deposits. 4. Patients present with consistently low serum complement levels. (Also see with poststreptococcal GN.) 5. This can be idiopathic or secondary (SLE). 6. Treatment: Steroids and immunosuppressives are not effective. 7. Prognosis: Poor, progressive. May progress to a RPGN clinical pattern and can recur in transplants. |
PRO= poor prognosis... since it's a cross over... there's two types
II = two i's so Intramembranous deposits |
|
|
Membranoproliferative glomerulonephritis - Microscopic findings
|
1. H&E stain [Slide 57]: you can see proliferative changes and GBM changes. There is accentuation of the segmental architecture of the glomeruli.
[NT note: He really wants us to be able to tell if a glomerulus is hypercellular. So basically, every time you get a picture of glomeruli, ask yourself if there are more cells (more black dots) than there should be.] 2. H&E stain [Slide 58]: On higher magnification you can see trabecular changes in the GBM. You can see a split with “train tracks” with duplication. There is proliferation of mesangial cells and epithelial cells. Take home: you have both proliferative and membranous changes. 3. FM [Slide 59]: There are immune complexes all over the place. It doesn’t create the smooth linear pattern. It leans more toward the granular pattern. 4. EM-I [Slide 60, 61]: You can see two basement membranes going across. There are subendothelial deposits on the endothelial side (inside) of the GBM. There is an increase in mesangial matrix. 5. EM-II [Slide 62]: This type has intramembranous deposits in the GBM. This is clinically indistinguishable from Type I display, but the deposit locations are different. |
|
|
|
Secondary Glomerular Diseases
|
1. Diabetes Mellitus (Diabetic Nephropathy)
2. Amyloidosis [ 3. Systemic Lupus Erythematosus (SLE) |
|
|
|
Diabetes Mellitus (Diabetic Nephropathy)
|
1. People with diabetes don't die because they have high blood sugar. Most die of renal failure, stroke, or infections.
2. Diabetes is a renal and vascular disease. a. For example, the lower extremities of diabetics have good blood supply that is evident by a strong dorsalis pedis pulse, but problems at the microvascular level (i.e., the capillary bed) are what lead to the blackened, gangrenous toes characteristic of diabetics. This is the same process that happens in the retina leading to the characteristic features of diabetic retinopathy. 3. Because it's so pervasive and prevalent in the general population, it's a major cause of renal disease morbidity, mortality; HTN is a vascular disorder that goes along with diabetes too, and the kidney is a target organ. 4. There are vascular changes of arteriolosclerosis. 5. There is nodular glomerulosclerosis. Some may resemble focal segmental glomerulosclerosis (you need to be able to distinguish these two). 6. Papillary necrosis - The medullary papillae are at risk for microvascular changes. 7. Uniformly thickened GBM - Any capillary bed in the diabetic patient will be thick. 8. No immune deposits – This is not an immune-mediated disease! |
|
|
|
Diabetes Mellitus (Diabetic Nephropathy) - microscopic findings - H&E stain
|
a. H&E stain [Slides 66, 67]: There are some very characteristic lesions of the kidney that go along with diabetic neuropathy.
i. This is a nodular diabetic glomerulosclerosis. There are spherical "basketballs" in segments. ii. Vascular changes occur in the background as well, vascular changes can show up before the glucose problems. iii. For the most part, it's fairly diffuse (not focal), but it is segmental in its distribution. |
|
|
|
Diabetes Mellitus (Diabetic Nephropathy) - microscopic findings - EM
|
i. If you remember from previous images, normal GBM is about the width of one foot process. This is 3-5x thicker on the edge of one of the sclerotic nodules. There is a lot of mesangial matrix but not a lot cellularity, no granularity. (Rv note: If it is happening in the capillary bed of the kidney it is happening in every capillary bed in the body.)
ii. The thickened GBM contributes to relative "ischemic state" of the microvasculature that puts these patients at risk for other diseases. |
|
|
|
Amyloidosis
|
1. This can occur idiopathically or secondarily (in patients with long term antigenic stimulation).
2. It’s characterized by hyaline lesions; deposition of extracellular protein in kidneys (glomeruli, vessel walls, interstitium), though amyloid can affect other organs (cardiac, hepatic, splenic, single organ, systemic amyloidosis). 3. NON proliferative – no cellular proliferation 4. Heterogeneous composition – It’s not a single type of protein 5. Congo red stain - gives tissue unique tinctorial characteristics 6. This has unique EM structure-non-branching fibrils. 7. This is also associated with the nephrotic syndrome. |
|
|
|
Amyloidosis Microscopic findings - H&Estain
|
1. There are big sclerotic segments that are much more global, not focal or segmental.
2. This could be confused with diabetic glomerulosclerosis on H&E. But amyloid patients are not necessarily diabetic. 3. Amyloid can be deposited in media in the small arterioles, and can resemble changes of arteriolosclerosis seen in diabetic glomerulosclerosis. (Amyloid deposits are more “irregular”.) 4. Lesions of amyloidosis are more polygonal due to protein deposits (they’re not spherical "basketball"-shaped, but difference is subtle). |
|
|
|
Amyloidosis Microscopic findings - FM
|
1. Some forms of amyloid are positive on FM due to lambda light chains (they light up with light-chain antiserum).
2. This distinguishes amyloid from diabetic GS, where sclerotic lesions are negative on FM. |
|
|
|
Amyloidosis - microscopic findings - EM
|
It shows a fibrillar, non-branching material. (LYN: The diabetic sclerotic segments are more granular and homogenous on EM.)
|
|
|
|
Systemic Lupus Erythematosus (SLE)
|
1. This can mimic any form of glomerulonephritis (or may even have normal kidneys). They can have:
a. Nephritic syndrome with proliferative changes b. Nephrotic syndrome with minimal or membranous changes c. Membranoproliferative changes 2. Immune complex mediated 3. Progressive disease 4. Kidney is one of the major target organs in patients with SLE; significant cause of morbidity and mortality. 5. SLE diagnoses by clinical features – not by renal biopsy. You can do a biopsy when you have a urinalysis abnormality in a lupus patient. a. The biopsy distinguishes between severity for prognostic reasons to assess how progressive it's going to be: i. Nephrotic/minimal change is good. ii. Membranoproliferative is bad. 6. SLE patients don't die because of circulating auto-antibodies. They because the kidney, heart, and brain are target organs of these auto-antibodies. |
|
|
|
SLE - microscopic findings
|
a. H&E stain [Slide 74, 75]: This is a biopsy of lupus patient; there are membranoproliferative kinds of changes. This is classic evidence of membranoproliferative glomerulonephritis: lots of extra cells, capillary lumens are not evident, GBM are thick.
i. This is considered to be the membranoproliferative form of lupus glomerulonephritis. b. FM [Slide 76]: SLE is characterized by circulating immune complexes, so you would predict immunofluorescence would be positive. c. EM [Slides 77, 78]: *Immune complexes have subepithelial, subendothelial, AND intermesangial deposits.* i. They’re not in an isolated or regular pattern of immune complex deposition - not just epithelial, subepithelial, or subendothelial. ii. The "all over the place" hybrid/irregular pattern of immune complex deposition is a flag for undiagnosed lupus. iii. Long term prognosis is poor |
|
|
|
Chronic Glomerular diseases (“End stage kidneys”)
|
1. Diffuse global glomerulosclerosis
2. Diffuse tubular atrophy, interstitial fibrosis, shrunken kidneys 3. Kidneys are non-functional and patient is uremic. 4. Etiology may be difficult to determine 5. Must look carefully for any residual clues (if any persist) |
|
|
|
Glomerular Diseases Summary
|
1. There are no gross pathologic features to distinguish the forms of glomerular disease.
a. You can't diagnosis APGN by just looking at it. 2. Diagnosis is a combination of clinical information with multimodality examination of renal biopsy. a. Relatively few things are pathognomonic – one would be the FM IgA glomerulonephritis (naked tree with just the branches). 3. Biopsy must be adequate for evaluation – you need a certain number of glomeruli. 4. Biopsy can be important not only for diagnosis but for prognostic information. a. How advanced do kidneys look? 5. Not all diseases discussed are represented in slide set. 6. Need FM and EM to make specific diagnosis in most cases. |
|
|
|
Glomerular disorders that can be distinguished on a single H&E are
|
1. Cresentic GN (only when > ½ of glomeruli are involved)
2. Acute proliferative GN (postinfectious and SLE) 3. Nodular glomerulosclerosis (diabetes vs amyloid) 4. Chronic glomerulosclerosis (end stage kidney) 5. Focal segmental glomerulosclerosis (not in slide set) |
|
|
|
Tubulointerstitial Diseases – TID
|
1. Acute Tubular Necrosis (ATN)
2. Acute Pyelonephritis 3. Interstitial Nephritis |
|
|
|
Acute Tubular Necrosis (ATN)
|
1. This occurs when there is damage to the tubular epithelium lining the nephron causing necrosis and loss of function.
2. Various etiologies 3. It is a major cause of acute renal failure, but can be reversible because the renal tubule epithelium has the ability to regenerate if the underlying basement membrane is intact. (only other cells that regenerate are hepatocytes)(Rv: skin also) 4. Two broad categories of Acute Tubular Necrosis (based on cause of damage) a. Ischemic b. Nephrotoxic- 5. You don’t need to take a biopsy to diagnose acute tubular necrosis. A detailed history including all medications/ exposures to chemicals, biochemisty panels including elecctroytes, and the clinical presentation should be enough. 6. Grossly, Acute Tubular Necrosis [Slide 88] results in a pale cortex and a swollen kidney. ATN is treated with supportive therapy. a. Rv note: This is reversible, be sure to take a complete history and physical! 7. Slide 89 shows an example of cortical necrosis of the kidneys, which is also due to ischemia. Coagulative necrosis occurs in the kidney due to ischemia and usually appears as yellow tissue (but can’t really be seen well in this picture) |
|
|
|
Ischemic Acute Tubular Necrosis (ATN)
|
compromised intrarenal vascular supply leads to hypoxia causing cellular damage (ischemia can also result from large scale blood restriction such as clamping an aorta during major surgery)
|
|
|
|
Nephrotoxic Acute Tubular Necrosis (ATN)
|
1. due to cytotoxic elements; affects a particular segment of the tubule, most often the proximal convoluted tubule. (remember certain drugs act at certain parts of the tubules so these can cause damage if dosed incorrectly)
2. Heavy metal poisoning (ie: mercury) is a classic example of damage to the proximal convoluted tubule. |
|
|
|
Acute Pyelonephritis
|
1. Infection of the kidney; usually due to a bacterial infection (mostly gram negatives) that reach the kidneys either by ascending from ureters or via hematogenous routes (due to bacteremia).
2. Remember there is a special microenvironment in the kidney with the countercurrent mechanism creating high salt concentrations in the interstitium unlike anywhere else in the body. Some bacteria really like this salty spot, and may be able to grow here when they weren’t able to grow well in other parts of the body. a. Rv note: PMNs do not like this environment and do not function as well here. 3. Pyelonephritis is associated with urine stasis, obstruction, and retrograde flow (it often progresses from cystitis) because the bacteria are hanging around and given a chance to grow. 4. Results of an infection in the kidney are necrosis, edema, decreased urine production, and pus in the urine (pyuria) due to the presence of neutrophil infiltrates. Also it is common to see white blood cell casts. White blood cell casts are indicative of an infectious inflammatory process in the kidney itself. a. Rv note: Can get small pus pockets, suppuration with neutrophils. |
|
|
|
Acute Pyelonephritis - appearance
|
1. Grossly [93] the kidney will appear to have small white dots on the outer capsule that represent micro-abscesses. The mucosa in the calyx is markedly inflamed and dilated.
2. Due to the inflammation, the kidney will swell. Kidneys are enclosed in a capsule that is laced with nerve endings. The swelling of the kidney causes the nerves to get stretched and irritated, causing sharp pain radiating to the lower back. A light tap over the top of the kidney will result in sharp kidney pain, and this is a diagnostic maneuver called “Murphy’s Punch” 3. Slide 94 shows an example of the micro-abscesses, which give the speckled appearance. 4. Chronic Pyelonephritis results in fibrosis, necrosis, loss of nephron units, and scarring, decreasing the function of the kidney. Slide 95 shows a scarred shrunken kidney with a collapsed cortex due to infection. 5. Diagnosis can be based on the history and physical, with urine tests. Treat with broad spec ABX originally until you culture and narrow down your drug of choice. Do not biopsy for diagnosis. |
|
|
|
Interstitial Nephritis
|
1. The kidney has diffuse interstitial inflammation that is not caused by infection, but is instead an acute immunologic hypersensitivity reaction due to toxins or drugs (ex. NSAIDS or methicillin (a.k.a-synthetic penicillins))
a. History- APCs (aspirin, phenacetin and caffeine) – used for rheumatoid disease, the hypersensitive reaction resulted with prolonged use and increase dosing used in the treatment of RA. Pathogenesis due to the combined use and cumulative dose. 2. The interstitium becomes filled with acute inflammatory cells. This affects the microvasculature and results in papillary necrosis. |
|
|
|
Interstitial Nephritis - appearance
|
1. Histologically [97], the tubules are not back to back and are separated by the swollen interstitium due to the infiltrates. The interstitium is (diffusely) inflamed and expanded, causing the tubules to be compressed. Note however that the glomeruli look undamaged. If you stop the drug (inciting agent) this will clear up and return to normal.
2. [98] Grossly, the tips of the papillae become yellow from coagulative necrosis. a. In addition to acute pyelonephritits and interstitial nephritis, papillary necrosis also occurs in diabetic nephropathy and sickle cell disease. (note the 4 conditions with papillary necrosis) |
|
|
|
Renovascular Diseases
|
1. causes kidney damage based on vascular problems.
2. They are usually accelerated by hypertension and the resultant arteriolosclerosis and may eventually cause endothelial cell necrosis and kidney shut down (emergency situation). 3. Slide [102] shows an example of arteriolosclerosis, notice the thickening of the walls around the arterioles. 4. types: a. Benign Nephrosclerosis b. Accelerated Nephrosclerosis c. Renal Artery Stenosis d. Thrombotic Microangiopathic Disorders |
|
|
|
Benign Nephrosclerosis
|
1. occurs over a long period of time and produces gross cortical changes.
2. Small, shrunken kidneys, VERY thin cortex, would see advanced vessel changes of arteriolar sclerosis but pyramids remain around the normal size |
|
|
|
Accelerated Nephrosclerosis
|
the same process, but occurs much faster due to an acute rise in blood pressure (i.e. 220/160) as in the case of malignant hypertension. [103] Medical emergency!
(Arteriolosclerosis leads to nephrosclerosis – it’s just a faster process w/ HTN) |
|
|
|
Renal Artery Stenosis
|
either acquired due to plaque buildup, or may be congenital
|
|
|
|
Thrombotic Microangiopathic Disorders
|
a group of disorders which involve the activation of the coagulation cascade causing formation of fibrous strands within the microvasculature
|
|
|
|
Many different microangiopathies can cause renovascular disease, inclulding:
|
1. hemolytic uremic syndrome, thrombotic thrombocytopenia purpura, eclampsia and pre-eclampsia, lupus erythematosus, malignant hypertension, DIC, etc…(hemolytic anemia…)
2. To improve the underlying renal disease caused by these disorders, you have to really treat the contributing disease first, then the renal situation will hopefully improve. 3. Dr. Rodriguez said that whenever there is a problem with the kidney, always keep Lupus in your differential because it can “do anything in the kidney” –present many different ways. |
|
|
|
Infarcts
|
1. also considered a renal vascular disease.
2. usually embolic and cause the classic peripheral wedge shaped area of coagulative necrosis. 3. Ischemia of a small area of the kidney is often clinically silent. 4. An example of an acute infarct is shown on slide 110: notice the collapsed, contracted area of the kidney where the infarct occurred. Classic wedge shaped example is shown on slide 111. |
|
|
|
Renal Diseases
|
1. Congenital Diseases
2. Renal Neoplasms 3. Obstructive Diseases 4. Nephrolithiasis |
|
|
|
Congenital Diseases
|
1. Anomalies: Agenesis, Hypoplasia, Ectopic, Horseshoe, Bifid Ureters
2. Cystic Diseases Medullary Cystic Diseases 3. Others a. Acquired cystic disease due to cystic degeneration b. Simple Cysts |
|
|
|
Quick refresher on kidney development
|
1. The nephric duct produces the ureteric bud that invades the metanephric mesenchyme (metanephric blastema), eventually forming the collecting system and the ureters.
2. The mesenchymal cells around the branches of ureteric bud are stimulated to become nephron units. 3. The nephric duct also migrates caudally to fuse with the bladder, while the newly forming kidney tissue moves cranially and rotates as the body grows. • Therefore could have a kidney and ureters develop anywhere along this ling of ascent. |
|
|
|
Horseshoe kidneys
|
1. usually only discovered as a result of exploratory surgery after a traumatic event.
|
|
|
|
Anomalies
|
1. Horseshoe kidneys
2. Also, it’s important look out for bifid ureters [115] during surgery so that a functional ureter is not accidentally clipped. 3. Also can have two renal arteries. 4. With agenesis – baby may actually make it to term because the mom’s kidneys were doing all the work. |
|
|
|
Cystic Diseases
|
1. Autosomal Dominant - adult polycystic disease
2. Autosomal Recessive- Childhood cystic disease |
|
|
|
Autosomal Dominant - adult polycystic disease
|
1. If you can palpate a patient’s kidney, it is likely they have this disease.
2. In patients with this disease, the kidneys will have small cysts at birth, which will expand slowly over decades causing grossly enlarged kidneys. 3. Patients are usually fine until later adult life when these expanding cysts start to compress the nephrons and compromise kidney function. 4. Clinically patients will present with HTN and hematuria. 5. These have a very classic gross appearance, also on seen on slide 118 (may be a good one to know.)(Rv Note: Disease remains in the population because the patients survive to reproduce.) |
|
|
|
Autosomal Recessive- Childhood cystic disease
|
1. causes cystic dysplasia.
2. less common and is catastrophic, causing a grossly malformed kidney which is mostly non functional and incompatible with long term survival 3. Also called cystic renal dysplasia |
|
|
|
Medullary Cystic Diseases
|
a. Medullary Sponge Kidney
b. Nephronophthsis |
|
|
|
Simple Cysts
|
1. these are just single thin walled translucent cysts.
2. They are usually asymptomatic unless fluid accumulation causes the kidney to bleed or rupture, causing retroperitoneal pain. 3. Easily discovered by ultrasound, but may never cause a problem. |
|
|
|
Renal Neoplasms
|
1. The cell line of most renal neoplasms is the renal ephithelium, usually renal tubular epithelium.
2. Adenoma 3. Renal Cell Carcinoma 4. Wilms Tumor (nephroblastoma 5. Transitional Cell Carcinoma |
WART
|
|
|
Adenoma
|
1. A solid mass usually less than 1-2 cm in size.
2. This is a controversial “adenoma” because they are benign when small, but if they grow bigger than about 2 cm, they have the potential to metastasize. |
|
|
|
Renal Cell Carcinoma
|
1. Carcinoma is usually at one of the poles of the kidney, not the middle.
2. Dissected, it has a “variegated” appearance with areas of necrosis and hemorrhage i. Arrow points to the venous invasion by the carcinoma- a feature atypical for other carcinomas in the body, but very typical for Renal Cell Carcinoma. This is the main route for metastatiss, and can sometimes result in the carcinoma actually causing pulmonary embolism. (hepatocellular carcinoma is also known for venous invasion)(Rv: Renal vein to IVC invasion in particular was noted.) 3. RCC may be clinically silent; a metastatic malignancy to other parts of the body is usually what brings patients in. 4. RCC is typically a slow growing tumor, so it may be possible in some cases to remove the carcinoma and save the kidney. 5. This is often called clear cell carcinoma because the cells have lots of clear cytoplasm. |
|
|
|
Wilms Tumor (nephroblastoma)
|
1. Occurs in the pediatric age range and grossly has a more homogenous appearance than RCC. Usually are eccentric (not at the kidney poles) and are often bilateral. Suspect this if you feel a mass on an abdominal exam of an infant.
2. Histologically, it has a very “embryonic” look to it – mesodermal tissue, spindle cells, and maybe some primitive nephron units. 3. Wilms tumor used to be 100% fatal. But thanks to a national registry and new aggressive chemotherapies, many children can go on to lead productive lives. |
|
|
|
Transitional Cell Carcinoma
|
1. Grossly [126] has the traditional “cauliflower” appearance. In this picture the tumor is in the collecting system.
2. Patients may present with hematuria due to cells flaking off; 3. may be cured with surgery depending on location. b. Rv note: This transitional cell CA is analogous to a CA of other locations with transitional epithelium(ie-bladder, uretur). |
|
|
|
Obstructive Diseases
|
1. Anything that can block the tubes of the kidney can cause obstructive diseases
2. Any time there is stagnant urine hanging around, this allows bacteria to ascend into the kidney causing not only inflammation of the kidney and pyelonephritis, but also an infection of the entire urinary tract system. [130] shows a kidney with a chronic infection that has been filled with pus (pyonephrosis) and has a grossly distorted urinary tract. |
|
|
|
Obstructive Diseases causes
|
1. Causes include congenital anomalies, calculi (stones), prostatic hypertrophy, neoplasms, inflammatory disorders, papillary necrosis, pregnancy and uterine prolapse, neurogenic bladder
2. With obstruction , there is no place for the urine to go so it backs up and puts pressure on the collecting system causing it to dilate. This can be seen grossly [128], but be sure not to mistake it for cysts. This appearance is indicative of chronic obstruction. It does not affect the cortex until the obstruction has been prolonged. 3. [129] A congenital urethral stricture (such as a urethral flap) is an obstruction that causes decreased fetal urine output and oligohydraminos- a decrease in amniotic fluid. This creates a back up of urine in the kidneys, which can prevent normal kidney maturation. In the picture note that the ureter is distended and dilated, and fluid has backed up into the kidney (hydronephrosis) preventing normal development. i. Rv note: Hydronephrosis denotes a long standing obstruction – see dilation through the entire system even in ureturs, filled with “water clear” urine. |
|
|
|
Nephrolithiasis
|
1. Kidney stones (or “rocks”) are very common.
2. They are usually calcified renal stones which are radio-opaque on X-ray( remember gallstones are radiolucent). 3. May can be congenital or acquired |
|
|
|
Nephrolithiasis extras
|
1. Dystrophic calcifications
2. Sound waves are not very efficient in braking up these renal stones but may work sometimes. 3. Even a 5-6 mm stone can cause excruciating pain. 4. May be a complication of pyelonephritis OR a contributing cause of pyelonephritis due to the obstruction the stone causes. 5. Most commonly renal stones are composed of calcium oxalate, magnesium ammonium phosphate, uric acid, and cysteine. 6. Urinalysis may help to determine the chemical makeup of the stone and can aid in treatment. If there are mostly acidic components to the stone, adding base to the urine may help break up or dissolve the stone. 7. Slide 132 represents a “stag-horn” stone (“looks like an elk rack”)as seen on the left hand side. LYN NT Note: Use your imagination here 8. The ureter contractions required to pass these stones is extremely painful. 9. Slide 133 shows an advanced case which has caused destruction of renal tissue. |
cmcu --> can michael call U?
|
|
|
Diseases of the Male Genital System
|
1. Penis and penile urethra
2. Testis and epididymis 3. Prostate |
|
|
|
Diseases of the Penis and Penile Urethra
|
1. Atrophy, agenesis, hyperplasia, and hypoplasia of the penis - congenital anomalies that are extremely rare
2. Epispadias and Hypospadias [32] - Two of the most common congenital anomalies 3. Disease affecting the Glans and Prepuce 4. Neoplasms of the Penis |
|
|
|
Epispadias and Hypospadias
|
1. Congenital, anomalous openings of the urethra on the penile shaft
a. Can occur anywhere along the penile shaft 2. Disease Associations a. Abnormal testicular descent (more so in epispadias) and GU malformations 3. Clinical significance a. Abnormal urination b. Infections of the glans and prepuce c. Often associated with stenosis of urethral meatus, urinary retention (and urinary stasis) and UTI’s d. Infertility caused by abnormal ejaculation depending on the location of the opening of the urethra relative to the penis NT Note: LYN made a distinction between infertility and sterility, but Dr. DeFatta used both interchangeably. The point is epi/hypospadias can cause infertility by affecting the delivery of semen but not the semen’s potency for reproduction. |
|
|
|
Epispadias
|
opening occurs on the dorsal surface of the penis
|
|
|
|
Hypospadias
|
opening occurs on ventral surface (anywhere from the coronal sulcus --> perineum)
|
|
|
|
Disease affecting the Glans and Prepuce
|
1. Phimosis
2. Balanoposthitis: 3. Syphilis |
|
|
|
Phimosis
|
1. Opening of the prepuce too small to allow normal retraction
a. Collar too tight to pull shirt over head 2. Can be caused by congenital anomaly or chronic infection (and then scarring) 3. Paraphimosis: prepuce retracted but too tight to be extended i. Once shirt is on, tight collar prevents you from taking it off 4. Treat phimosis and paraphimosis with circumcision |
|
|
|
Balanoposthitis:
|
1. Infection of the glans and prepuce [34]
a. Many causes: i. Poor local hygiene is a major contributing factor • Smegma - debris, sweat, skin oils, dirt and denuded epithelial cells • Smegma collects under prepuce and acts as an irritant, a growth medium for infection, a carcinogen, and a breeding ground for HPV ii. STD’s: Syphilis, gonorrhea, chancroid, lymphogranuloma venereum (LGV), genital herpes iii. Candidiasis noted in >35yo population 2. Presents histologically with non-specific inflammation: neutrophils, lymphocytes and even plasma cells (although plasma cells are not seen in the frequency they’re seen in with syphilis) |
|
|
|
primary syphilis
|
i. Occurs on the glans
ii. Starts with firm erythematous papule which ulcerates into hard chancre iii. Acute and Chronic inflammation present on biopsy • Plasma cell is the most prominant cell seen in ulcerated area • Plasma cells and lymphocytes underly the ulcer and form peri-vascular cuffing around the blood vessels (known as obliterative endarteritis – infection of small arterioles) |
|
|
|
Secondary syphilis
|
condyloma lata (flat macule)
|
|
|
|
Tertiary syphilis
|
gummas (granulomas) result in CNS lesions
|
|
|
|
Benign Neoplasms of the Penis
|
Condyloma Acuminatum (genital warts)
|
|
|
|
Condyloma Acuminatum (genital warts)
|
i. Benign neoplasm of squamous mucosa caused by HPV types 6 and 11
• Malignant transformation can occur (but not usually from serotypes 6 and 11) • Serotypes 16 and 18 are more associated with malignant transformation – Know this!! ii. Venereal transmission iii. Lesions on genitalia or perineum – can occur anywhere by direct contact (Condoms don’t prevent the spread of HPV) iv. Many HPV serotypes with varying degree of association • Virus can be demonstrated in tissue with special techniques (immunofluorescent staining) |
|
|
|
Condyloma Acuminatum (genital warts) - Gross appearance
|
1. Warts usually present as reddish, polypoid (sessile or pedunculated) lesions, up to several centimeters in size.
2. However, they can also be flesh colored, flat, and/or look like moles – HPV lesions can mask as many different things |
|
|
|
Condyloma Acuminatum (genital warts) - microscopic appearance
|
1. Epithelial hyperplasia with viral changes (koilocytosis) [37]
2. Dysplastic features extending to frank carcinoma can be seen 3. Koilocytosis: Enlargement of cells, shrinkage and hyperchromasia of the nucleus with a clear space around it (looks like a raisin). This is the characteristic appearance of HPV infected cells |
|
|
|
Condyloma Acuminatum (genital warts) - Clinically
|
1. Uncircumcised males are more prone to HPV infections that circumcised males due to increased mucosal surface under the foreskin and on the glans itself
2. Venereal warts look the same as a wart anywhere else on the skin – their location and etiology (HPV serotypes 6 and 11) designates them as “genital” warts 3. Once you get genital warts, “you pretty much have them,” as they are hard to eradicate. The task is to determine whether or not they will progress into more serious lesions; so they are excised, biopsied, and monitored carefully after treatment. |
|
|
|
Malignant Neoplasms of the Penis
|
1. Most are squamous cell carcinomas (SCC)
2. Most commonly associated with infection, especially HPV. i. 80% of studied cases are associated with HPV 16 or 18 infection 3. All exhibit architectural and/or cytologic features of malignancy i. Large thickening of epidermis which will invade down into soft tissue; inflammatory response; abnormal keratinocytes; alteration of basement membrane; squamous pearls 4. All can become invasive except Bowenoid Papulosis |
|
|
|
Carcinoma in situ of the penis:
|
1. Bowen Disease
2. Erythroplasia of Queyrat 3. Bowenoid papulosis |
|
|
|
Bowen Disease
|
1. Squamous cell carcinoma in situ that affects the skin surfaces of the prepuce and shaft
2. Grossly - reddish plaques, but again be aware they can have many different appearances 3. Microscopically - loss of stratification, disorderly maturation, dysplasia (large bizarre cells throughout full thickness of epithelium), chronic inflammatory response, confined above the basement membrane 4. Can transform into invasive squamous cell carcinoma in approximately 10% of patients. |
PBS
|
|
|
Erythroplasia of Queyrat
|
1. Squamous cell carcinoma in situ of the mucosal surfaces of the glans and prepuce
2. Histologically looks identical to Bowen’s, can only be distinguished by location 3. Grossly: Single, or often times multiple, reddish plaques 4. Microscopically: Indistinguishable from Bowen’s 5. Can become invasive if untreated |
PEG
|
|
|
Bowenoid papulosis
|
1. Occurs in men < 35 y/o, usually on the skin of the penile shaft, glans, or scrotum
2. Lesions are multiple, raised, flesh-colored papules found in a group or cluster 3. Histologically – similar to squamous cell carcinoma in situ (SCCa – IS). They are indistinguishable from Bowen and Erythroplasia histologically. 4. 80% result from HPV 16 5. Different from Bowen Disease in that it is found in YOUNGER patients and has MULTIPLE papular lesions that may disappear spontaneously without treatment 6. Only one of the three types of Squamous Cell Carcinoma in situ that does not become invasive (NT Note: most important thing to know about Bowenoid Papulosis). |
oid... occurs in younger... papulosis--> can be several
|
|
|
Invasive Carcinoma of the penis –
|
Squamous Cell Carcinoma
|
|
|
|
Squamous Cell Carcinoma
|
1. Uncommon in the US causing only 1% of male cancers
2 Etiology - related to exposure to carcinogens in smegma, HPV 16 and 11 and poor hygiene (poor hygiene sets up for infection, irritation, dysplasia, and carcinoma) - HPV DNA detected in 50% cases studied 3. Frequency is inversely proportional to prevalence of circumcision – less exposure to carcinogens in smegma and lower chance of HPV infection - SCC of the penis is rare among Jews (thank the mohels) |
|
|
|
Squamous Cell Carcinoma - gross appearance
|
Usually originate on glans or prepuce with variable presentation- can appear as reddish plaques, flesh colored lesions, wart or mole-like; progress to ulcerative or exophytic (cauliflower-like) lesions
|
|
|
|
Squamous Cell Carcinoma - microscopic appearance
|
1. features of squamous malignancy with invasion beneath the basement membrane.
2. Differ from condyloma accuminatum by darker cells and more inflammatory and fibrinous debris; squamous pearls |
|
|
|
Condyloma Acuminatum (genital warts) - Clinically
|
1. Uncircumcised males are more prone to HPV infections that circumcised males due to increased mucosal surface under the foreskin and on the glans itself
2. Venereal warts look the same as a wart anywhere else on the skin – their location and etiology (HPV serotypes 6 and 11) designates them as “genital” warts 3. Once you get genital warts, “you pretty much have them,” as they are hard to eradicate. The task is to determine whether or not they will progress into more serious lesions; so they are excised, biopsied, and monitored carefully after treatment. |
|
|
|
Malignant Neoplasms of the Penis
|
1. Most are squamous cell carcinomas (SCC)
2. Most commonly associated with infection, especially HPV. i. 80% of studied cases are associated with HPV 16 or 18 infection 3. All exhibit architectural and/or cytologic features of malignancy i. Large thickening of epidermis which will invade down into soft tissue; inflammatory response; abnormal keratinocytes; alteration of basement membrane; squamous pearls 4. All can become invasive except Bowenoid Papulosis |
|
|
|
Carcinoma in situ of the penis:
|
1. Bowen Disease
2. Erythroplasia of Queyrat 3. Bowenoid papulosis |
|
|
|
Bowen Disease
|
1. Squamous cell carcinoma in situ that affects the skin surfaces of the prepuce and shaft
2. Grossly - reddish plaques, but again be aware they can have many different appearances 3. Microscopically - loss of stratification, disorderly maturation, dysplasia (large bizarre cells throughout full thickness of epithelium), chronic inflammatory response, confined above the basement membrane 4. Can transform into invasive squamous cell carcinoma in approximately 10% of patients. |
|
|
|
Erythroplasia of Queyrat
|
1. Squamous cell carcinoma in situ of the mucosal surfaces of the glans and prepuce
2. Histologically looks identical to Bowen’s, can only be distinguished by location 3. Grossly: Single, or often times multiple, reddish plaques 4. Microscopically: Indistinguishable from Bowen’s 5. Can become invasive if untreated |
|
|
|
Bowenoid papulosis
|
1. Occurs in men < 35 y/o, usually on the skin of the penile shaft, glans, or scrotum
2. Lesions are multiple, raised, flesh-colored papules found in a group or cluster 3. Histologically – similar to squamous cell carcinoma in situ (SCCa – IS). They are indistinguishable from Bowen and Erythroplasia histologically. 4. 80% result from HPV 16 5. Different from Bowen Disease in that it is found in YOUNGER patients and has MULTIPLE papular lesions that may disappear spontaneously without treatment 6. Only one of the three types of Squamous Cell Carcinoma in situ that does not become invasive (NT Note: most important thing to know about Bowenoid Papulosis). |
oids are little... so found in younger patients... and multiple
|
|
|
Invasive Carcinoma of the penis –
|
Squamous Cell Carcinoma
|
|
|
|
Squamous Cell Carcinoma
|
1. Uncommon in the US causing only 1% of male cancers
2 Etiology - related to exposure to carcinogens in smegma, HPV 16 and 11 and poor hygiene (poor hygiene sets up for infection, irritation, dysplasia, and carcinoma) - HPV DNA detected in 50% cases studied 3. Frequency is inversely proportional to prevalence of circumcision – less exposure to carcinogens in smegma and lower chance of HPV infection - SCC of the penis is rare among Jews (thank the mohels) |
|
|
|
Squamous Cell Carcinoma - gross appearance
|
1. Usually originate on glans or prepuce with variable presentation-
2. can appear as reddish plaques, flesh colored lesions, wart or mole-like; 3. progress to ulcerative or exophytic (cauliflower-like) lesions |
|
|
|
Squamous Cell Carcinoma - microscopic appearance
|
1. features of squamous malignancy with invasion beneath the basement membrane.
2. Differ from condyloma accuminatum by darker cells and more inflammatory and fibrinous debris; squamous pearls |
|
|
|
Squamous Cell Carcinoma - clinical course
|
1. Slow growing (indolent), local metastasis to the inguinal & iliac nodes
2. Only make up 50% of palpable lymph nodes; other half results from benign hyperplasia 3. Widespread metastasis is an uncommon, but occasional, late feature 4. Patients usually present late in course and with a large lesion 5. Treatment: Amputation and chemotherapy 6. Prognosis is related to stage a. No node involvement: 66% 5-year survival b. Distal Lymph node involvement: 27% 5-year survival |
|
|
|
Normal Testis and Epididymis
|
1. Adults – 12-18 gm
2. Capsule composed of tunica vaginalis, tunica albuginea, and tunica vasculosa (outer to inner) |
|
|
|
Diseases of the Testis and Epididymis
|
1. Cryptorchidism
2. Inflammation of the Testis and Epididymis 3. Torsion 4. Hydrocele |
testes ITCH
|
|
|
Cryptorchidism
|
1. Incomplete testicular descent into scrotum (arrest in either of two phases of descent: abdominal phase or inguinal canal phase)
2. Etiology – congenital, with possible hormonal mechanism 3. Frequency – 1% boys aged 1 year 4. Location of testis: Can be anywhere from abdomen (only 10%) to upper inguinal canal (most common location) 5. Can be unilateral (75% cases) or bilateral (25%) 6. Can be associated with other congenital anomalies (hypospadias/epispadias) and inguinal hernias [49] 7. Abnormalities of testis can develop within 2 years of birth if not corrected a. Atrophy (often of both testes) & sterility i. Studies suggest that even if one testis fails to descended, both may show abnormalities – this suggests, again, hormonal involvement. b. Trauma – crushing within inguinal canal c. Carcinomas: 5-10 fold greater risk in undescended testes |
|
|
|
Histological examination of cryptorchidism
|
1. reveals testicular atrophy (seen also in Klinefelter’s and testicular dysgenesis)
2. Fibrosis of seminiferous tubule with loss of germ cells and a thickened basement membrane 3. Profuse packing of Leydig cells in interstitium between the tubules |
|
|
|
Cryptorchidism - treatment
|
1. Orchiopexy: placement of testis in scrotal sac and suturing of the testes into place
2. Ideally done before permanent damage begins at 2 years 3. Sterility/atrophy may still occur (50-60% still affected) 4. Some feel cancer risk reduced if orchiopexy done before 10 years of age but this is controversial |
|
|
|
Inflammation of the Testis and Epididymis
|
1. Epididymitis
2. Orchitis |
|
|
|
Epididymitis
|
1.. Inflammation of the epididymis
2. Usually infectious – bacterial, chlamydial, viral – Varies with age of patient. i. <35 yo men: Neissseria gonorrhoeae & Chlamydia trachomatis most common ii. >35 yo men: Coliforms more common (E. coli) iii. Tuberculosis - associated with disease in prostate and seminal vesicles, then later involves epididymis and, finally, testis • Presents with caseating granulomas and positive AFB stains. iv. Syphilis: Almost always begins in testis (gummatous orchitis) and later, if at all, spreads to epidydimis, and finally produces lesions on glans penis • PLASMA CELL INFLAMMATION IN SYPHILIS 3. Acute inflammatory foci in epidiymis --> microabscesses, scarring, and sterility if left untreated |
|
|
|
Orchitis
|
1. Inflammation of the testis
2. Usually infectious - bacterial, Chlamydial, viral 3. Associated with disease elsewhere in GU tract – usually UTI’s seen in older males 4. Can have abscess formation as well as acute purulent discharge 5. Mumps Orchitis: |
|
|
|
Mumps Orchitis
|
i. Swelling of the scrotal sac (5-10X) that accompanies mumps virus infection of salivary glands. Orchitis can occur anytime, from before parotid symptoms start to ~1 week after.
ii. Usually seen in older males (20-30% of mumps cases); almost never in kids iii. Usually unilateral, but can sometimes be bilateral: If bilateral, can cause atrophy & sterility due to inflammatory process iv. Histology: Warthin-Finkeldey Giant Cells – large multinucleated cells found with mumps |
|
|
|
Torsion
|
1. Twisting of the spermatic cord due to increased mobility of testicle on its pedicle
2. Usually seen in men between the ages of 15 and 30 3. Arterial inflow continues while venous outflow (pampiniform plexus) is occluded a. Severe engorgement of testis with hemorrhage, possible necrosis (venous infarction) 4. Gross: engorgement with blood and coagulation necrosis of spermatic tubules 5. Treatment: Can correct spontaneously, or may require surgical intervention that involves fixing of other testis to scrotal wall to preserve sterility. a. Surgical intervention should take place within 6 hours of symptom onset in order to save testis; orchiectomy will be performed if testis not salvable |
|
|
|
Torsion is often associated with:
|
1. Trauma or violent movement
2. Incomplete testicular descent 3. Absence of the gubernaculum testis (mesenchymal column of tissue that connects the fetal testis to the developing scrotum and that is involved in testicular descent) allows free rotation of the testis 4. Testicular atrophy (with increased mobility) |
|
|
|
Hydrocele
|
1. Abnormal accumulation of clear serous fluid within the tunica vaginalis (serosa-lined sac in scrotum)
2. Many causes: Trauma, infections, tumor, lymphatic obstruction (also causes elephantiasis), metastatic disease, cases with no obvious cause 3. Can cause extreme swelling of scrotum (5-10x normal size) 4. Diagnosis: Transillumination can be used to differentiate between hydrocele and testicular tumor a. Shine light into scrotal sac. This illuminates fluid, and allows visualization of the normal testis. 5. Treatment: Conservative measures (draining of the fluid) often; removal of sac if severe, persistent |
|
|
|
General clinical features of testicular tumors
|
1. Presentation usually as mass, often painless
a. If detected early can be palpated as mass within testis that has not spread 2. Aggressive cancers can present with metastases first a. Primary tumors often small, undetectable on physical exam |
|
|
|
Types of testicular tumors
|
1. Germ cell tumors (GCTs):
2. Stromal tumors: 3. Other rare tumors of vascular, soft tissue origin |
|
|
|
Germ cell tumors (GCTs):
|
1. comprise 95% of testicular tumors.
2. Seminomatous and non-seminomatous types 3. Arise from seminiferous tubule elements (multipotent germ cells) 4. Usually arise via in situ stage (intratubular) |
|
|
|
Stromal tumors: comprise
|
1. ~ 5% of testicular tumors.
2. Leydig and Sertoli cell types 3. Arise from specialized, hormone-producing testicular stroma |
|
|
|
Testicular germ cell tumors (GCTs)
|
1. Tend to be more aggressive
2. Arise from multipotent germ cells a. Most arise from seminiferous tubule elements, usually via an in situ stage (aka intratubular germ cell neoplasia) b. Can develop into many types of tissues which makes diagnosis difficult, especially if trying to identify the origin of a metastasis 3. Incidence: 6 per 100,000 in US a. Increasing worldwide (we are not sure why) 4. Peak ages: Primarily 15-35 years and a smaller peak in old age 5. Racial predominance in US: 5:1 white to black ratio |
white men have smaller penises and are more likely to lose their balls
|
|
|
Pathogenesis of testicular germ cell tumors
|
1. Genetic predisposition:
2. Undescended testis 3. Testicular dysgenesis |
|
|
|
Genetic predisposition of testicular germ cell tumors
|
i. Isochromosome of short arm of chromosome 12 - i(12p) - seen in >90%
NT Note: know this genetic predisposition for test ii. Racial differences iii. Familial clustering – as more first degree relatives have testicular cancer, risk for unaffected males goes up 5-10x (or more) |
|
|
|
Testicular dysgenesis
|
1. derangement of spermatic tubule development in the fetus
2. Two types: • Kleinfelter’s Syndrome (47 XXY, undescended testes, testicular atrophy common) • Testicular Feminization (spermatic cells insensitive to androgens, externally appears female, but internal blind vaginal pouch and undescended testes) 3. Can result in sterility, and predispose to testicular tumors |
|
|
|
Undescended testis
|
Higher the testis in that pathway of descent, greater the risk
|
|
|
|
Classification of testicular GCTs
|
1. Based upon World Health Organization (WHO, Histological Classification of Tumors)
2. Classification based upon cell of origin (histogenesis) i. Multipotent cells can develop along many lines & exhibit many appearances, functions, characteristics 3. Further subdivided into pure vs. mixed forms i. 60% exhibit a mixture of 2+ patterns 4. THE MOST IMPORTANT DISTINCTION for clinicians: Seminomatous vs. Nonseminomatous (NSGCT) |
|
|
|
THE MOST IMPORTANT DISTINCTION for clinicians: Seminomatous vs. Nonseminomatous (NSGCT)
|
1. This is important because determines susceptibility to radiation treatment:
• Seminomatous: Radiosensitive, better prognosis • NSGCT: Radioresistant, worse prognoses |
|
|
|
Seminomatous
|
Seminoma
|
|
|
|
Non-Seminomatous
|
1. Embryonal carcinomas
2. Yolk sac tumors 3. Choriocarcinomas 4. Teratomas 5. Mixed GCTs |
YET CM
|
|
|
Seminoma
|
1. . Most common type of GCT, >50% of GCTs
2. Peak in 30s i. Small peak in old age ii. Extremely rare in infants 3. Tend to be larger, bulkier than other germ cell tumors i. Take up more of testicular tissue, replace it, cause 5-10x increase in testicular size ii. Grow in solid cords or nests of cells. Don’t form glands. iii. Usually confined within tunica albuginea, but epididymal invasion can be seen iv. Gross: smooth surface, yellow-tan color. 4. Tend to be radiosensitive (with an important exception: anaplastic seminomas) - know this!! NT Note: Radiosensitivity is the susceptibility of cells to the harmful effects of ionizing radiation. It is not radioopacity/translucency. 5. Three histologic variants of seminomatous GCTs: i. Typical (classical) 85% ii. Anaplastic 10-15% - RADIORESISTANT iii. Spermatocytic 1-2% |
|
|
|
Typical Seminoma
|
i. Microscopically:
• Nests of uniform, large, round-to-oval cells with distinct centrally-located nuclei and lots of wispy, eosinophilic cytoplasm (“seminoma cells”). Resemble spermatocytes • Lymphocytes scattered amongst the seminoma cells, as well as throughout the stoma • Cells contain human placental lactogen (hPL) • AFP &/or hCG produced in only ~10-15% cases, not used for diagnosis ii. Other features: • Lymphocytic infiltrate very characteristic • Non-caseating granulomas often seen • Relatively low mitotic count |
|
|
|
Anaplastic Seminoma
|
i. Microscopically: Still see nests of cells, fibromuscular stoma, and lymphocytic infiltrate, but will also see:
• Greater cellular & nuclear atypia (dysplasia) • Tumor (multinucleated) giant cells • Higher mitotic count – 3+ per high-power field ii. Grossly: may see hemorrhage and/or some necrosis iii. Radioresistant (exception to the rule) |
|
|
|
Spermatocytic Seminoma
|
i. Very rare
ii. In older age: Usually >65 iii. No preceding intratubular component known • No dysplasia of intratubular germ cells that leads up to tumor (unlike classic and anaplastic seminomas) iv. Slowly growing, only rarely metastasizing v. Radiosensitive vi. Histologically: solid pattern with three cell types – Large, intermediate (predominant), and small cells (not lymphocytes) vii. Age of the patient will tip you off to this type of tumor |
slow growing because old people are slow
|
|
|
Non-Seminomatous
|
1. Embryonal Carcinoma
2. Yolk Sac Tumor 3. Choriocarcinoma 4. Teratoma 5. Mixed Germ Cell Tumors |
|
|
|
Embryonal Carcinoma
|
i. Age Peak: Young adults (20-30 years)
ii. Pure forms uncommon (3%) iii. Embryonal elements are present in 45% mixed germ cell tumors. Relatively common. iv. These tumors are much more aggressive than seminomas, and (as is true for all mixed tumors) aggressiveness depends on which components predominate v. Grossly: Smaller, variegated cut (“rough and irregular”) surface with hemorrhage & necrosis vi. Microscopic: Multiple growth patterns: glands and papillae, tubules, alveolar groups • Mosaic appearance • Cells more anaplastic than seminomas (with the exception of anaplastic seminomas) vii. Tumor markers • AFP: from syncitial trophoblasts • hCG: from yolk sac cells viii. Diagnosis keys • Age group, aggressive, AFP and hCG, glands and papillae microscopically |
|
|
|
Yolk Sac Tumor
|
i. Also called infantile embryonal carcinoma or endodermal sinus tumor
ii. Most common testicular tumor in infants & children under 3 years with a good prognosis in this age group iii. Adult form - usually a component of a mixed germ cell tumor with poor prognosis in this age group. Prognosis worse if tumor is seen in pure form. iv. Microscopically - lacelike network of tumor cells, with papillae & cords of cells having capillaries at center (endodermal sinuses) • Schiller-Duval Bodies – pathognomonic for yolk sac tumors; germ cells surrounding a central capillary, resemble a glomerulus v. Grossly – look like seminomas. Flat, smooth, tan surface vi. Tumor markers • AFP: from syncitial cell origin (more important in YST than in embryonal carcinoma) • Alpha-1-antitrypsin vii. Diagnostic Keys • AFP, alpha-1-antitrypsin, and Schiller-Duval Bodies NT Note: know this for test |
|
|
|
Choriocarcinoma
|
i. Tumor of cytotrophoblasts/ syncitiotrophoblasts
ii. Highly malignant, most aggressive of all testicular tumors, especially if pure form iii. Often presents initially with metastases to lungs and hemoptysis • Primary lesion may be very small – not picked up until has reached its metastatic site • Can differentiate (eg., chorio can change into embryonal, mixed, or teratoma) and de-differentiate (become very dysplastic) on metastasis iv. Gross: tumor will outgrow its blood supply in the testis, infarct, and form a scar (white fibrotic mass). Also see lots of hemorrhage and necrosis v. Histologically: Identical to choriocarcinomas of ovary, uterus. See large multinucleated giant cells coupled with smaller cytotrophoblastic elements vi. Usually is a component of a mixed GCT: Presence associated with worse prognosis. vii. Tumor markers: • hCG: from syncitiotrophoblasts viii. Diagnostic Keys • Initially presentation as metastases and high hCG |
|
|
|
Teratoma
|
i. Differentiation along 3 germ cell lines - ectoderm, mesoderm & endoderm
• Grossly: appear cystic/multiloculated, and are composed of a variety of components- skin, thyroid, bone, muscle, nerve/brain, gut, respiratory elements, embryonic tissues, etc ii. Any age - infancy to old age • Pure teratomas are the second most common testicular tumor in infants & children (#1 – yolk sac tumor) • In adults teratomas are usually a component of a mixed GCT • Pure teratomas in adults are considered malignant no matter what |
|
|
|
Subdivision of Teratomas
|
1. Mature teratomas
2. Immature teratomas |
|
|
|
Mature teratomas
|
1. Composed of recognizable, differentiated tissues
2. Muscle, nerve, skin, etc. 3. Typically benign tumors (but remember, in adults, treat like malignant) 4. Can have malignant transformation |
|
|
|
Immature teratomas
|
1. Composed of incompletely differentiated or primitive embryonic elements without organization
2. Fetal skin, fetal GI, fetal brain tissue, etc 3. Malignant tumors in all ages |
|
|
|
• Teratoma with malignant transformation are teratomas with clear-cut development of a malignancy from one of the elements within the teratoma
|
1. Squamous cell carcinoma of skin element
2. Papillary carcinoma of thyroid element 3. Adenocarcinoma of an intestinal element |
|
|
|
Mixed Germ Cell Tumors
|
i. 60% of GCT’s are mixed
ii. Most common mixture: teratoma + embryonal carcinoma + yolk sac tumor (14% of GCT’s) iii. Prognosis worsened by more malignant elements |
|
|
|
Spread of GCT’s
|
1. Local growth & invasion: extend to epididymis, cord
2. Metastases: i. Lymphatic: Para-aortic, pelvic nodes ii. Hematogenous: can affect lung, liver, bone, brain iii. Metastases may exhibit different tumor patterns than the primary tumor |
|
|
|
Treatment of GCTs
|
i. Surgery - radical orchiectomy,
ii. chemotherapy, iii. radiation for seminomas (except which one?? Hint: radioresistant) |
|
|
|
Staging of GCTs
|
i. Stage I - Confined to testis, epididymis, cord
ii. Stage II - Spread confined to retroperitoneal nodes and anything below diaphragm iii. Stage III - Metastases above diaphragm, outside retroperitoneal nodes |
|
|
|
Prognosis of GCTs
|
c. Survival – based on stage, type of tumor, & tumor dependent
i. Seminomatous – 70% 5 yr survival present in stage I ii. NSGCT’s – 60% 5 yr survival present in Stage II or III iii. More advanced the stage at presentation, lower the long term survivals iv. Pure choriocarcinomas present the worst prognosis |
|
|
|
Gonadal-Stromal Tumors of the Testis
|
1. Tend to be more benign and are often easy to cure
2. Arise from specialized, hormone-producing testicular stroma 3. Two subdivisions: a. From the stroma: Leydig Cell tumors b. From the sex cords: Sertoli Cell Tumors (Androblastomas) i. Picture shown in class: No hemorrhage or necrosis, doesn’t look as bad 4. Age range 20-60 on average 5. Gross: Brownish, hemorrhagic tumors usually <5 cm in diameter; look pretty benign grossly 6. Histologic: Leydig cell hyperplasia - similar to atrophic testis, but darker and more dysplastic 7. Can produce hormones - estrogen &/or androgen, depending on cell type present in tumor 8. Can present as mass or with hormonal manifestations |
|
|
|
Normal prostate
|
1. Weighs approximately 20 grams
2. Location: sits at the base of the bladder and surrounds urethra 3. Produces seminal constituents 4. Enlarges with age, and the older you get the more likely your chance of hyperplasia 5. Traditionally described as having 5 “lobes”, but they are really just regions with specific disease predilection 6. Most Important Fact On This Page (MIFOTP!)--> Normal prostatic gland has TWO layers: a basal cell layer and a columnar cell layer. Malignant prostatic gland has ONE layer: no basal cell layer. NT Note: This theme came up repeatedly throughout the rest of the lecture. Know it for the test. 7. Histology: composed of glands and fibromuscular stroma 8. More commonly described in Zones in pathology |
|
|
|
5 “lobes” of prostate
, but they are really just regions with specific disease predilection |
1. Median lobe - hyperplasia
2. Posterior lobe – adenocarcinoma, important for prostate exams |
|
|
|
Prostate Zones
|
1. Periurethral zone – area where urethra courses through prostate
2. Central zones – area surrounding ejaculatory ducts a. Often see hyperplasia 3. Peripheral zone – posterior aspect (roughly equal to posterior lobe) a. Often see adenocarcinoma 4. Transitional zone – in between central and peripheral zones |
|
|
|
Diseases of the Prostate
|
1. Infection / Inflammation
2. Prostatic Hyperplasia 3. Adenocarcinoma |
|
|
|
Infection/Inflammation
|
1. Infection / Inflammation – Most cases of prostatitis are infections that have to be diagnosed by culture. (Culture is from prostatic secretions expressed during digital rectal exam).
2. Three types: a. Acute bacterial prostatitis b. Chronic bacterial prostatitis c. Chronic abacterial prostatitis |
|
|
|
Acute bacterial prostatitis
|
1. Due to obstruction, or manipulation of the bladder or prostate (digital rectal exam, needle biopsy)
2. Organisms – Gram negative rods/coliforms (same organisms that cause UTIs) 3. Presents with perineal pain, fever and chills and with an enlarged, tender, soft-bodied prostate – don’t needle biopsy because will cause pain AND possibly sepsis when needle introduced. 4. Least hard to treat (especially if addressed early) 5. Repeated acute bacterial prostatitis can lead to: Chronic bacterial prostatitis |
|
|
|
Chronic bacterial prostatitis
|
1. Typically presents with vague symptoms of lower back pain, dysuria, & suprapubic/perineal pain
2. Often caused by recurrent UTIs. 3. Organisms - gram negative rods / coliforms |
|
|
|
Chronic abacterial prostatitis
|
1. Most common form of prostatitis today
2. Organisms implicated include Chlamydia trachomatis, Ureaplasma urealyticum, Mycoplasma hominis i. Considered “abacterial” because these organisms do not culture well and chronic prostatitis may be diagnosed without a cultured agent 3. Clinically indistinguishable from chronic bacterial prostatitis because you have the same symptoms, therefore must use digital rectal exam, fluid examination and culture i. If you see more than 10 WBCs per high power field in expressed prostatic secretions (EPS), but you repeatedly get negative urine cultures, then you need to consider the diagnosis of chronic abacterial prostatitis NT Note: Expressed prostatic secretions are the outcome of the prostatic massage. ii. Now, more DNA-based testing is available to look for the presence of Chlamydia, Ureaplasma, and Mycoplasma. 4. Antibiotic penetration of the prostate is poor due to capsule and fibromuscular stroma. The typical 7 day course of antibiotics is increased to a 30 day course to ensure bioavailability of antibiotics in the prostate. |
|
|
|
Prostatic Hyperplasia
|
1. sometimes referred to as “nodular hyperplasia” because it is nodular AND hyperplastic
2. Many clinicians refer to it as benign prostatic hyperplasia (BPH) but the use of “benign” is redundant. 3. Hyperplasia of both the glandular cells and the fibromuscular stroma in varying combinations 4. Preferentially affects the median lobe (or periurethral and central zones) a. This predilection for the periurethral and central zones explains why the urethra is compressed causing urinary obstruction and stasis 5. Normal finding in men with advancing age a. Can be present in the whole gland in very old men |
|
|
|
Prostatic Hyperplasia - Etiology
|
1. related to androgens: dihydrotestosterone (DHT)
2. Testosterone entering stromal cell is turned into DHT by 5a-reductase type 2. DHT binds to androgen receptors on the nuclear membrane to cause the nuclear production and secretion of growth factors. These growth factors leave the stromal cell and enter/activate epithelial cells. 3. DHT can also diffuse out of stromal cell without binding to intracellular receptor and cause activation of neighboring epithelial cells. 4. Testosterone can also go straight to epithelial cells to activate (although less potently than DHT) 5. Activated epithelial cells divide and become more numerous NT Note: For a much less confusing visual aid, see Robbins. |
|
|
|
Prostatic Hyperplasia
(appearance, clinical presentation, and treatment) |
1. Gross – firm nodules on cut surface (look multicystic but are actually spongy); narrow urethra [87]
2. Clinical – enlarged, firm nodular gland (difficult to distinguish BPH from tumor) 3. Microscopic – glandular increase/branching, increased fibromuscular stromal density, nodularity a. NO features of malignancy b. BPH GLANDS WILL HAVE TWO CELL LAYERS: BASAL AND COLUMNAR because it is not _________. (answer: malignant) 4. Drugs available target DHT sensitivity in prostatic cells in order to reduce glandular and stromal proliferation/activation. Also, alpha receptor antagonists relax smooth muscle to alleviate symptoms. |
|
|
|
Clinical implications of prostatic hyperplasia
|
1. Urinary outflow obstruction, which can cause UTI, hesitancy (physiologic pee-shyness), urgency (gotta go!), dribbling (didn’t make it!), frequent urination, nocturia, bladder hypertrophy, and hydroureter/nephrosis
2. No predisposition to cancer associated with BPH NT Note: know this i. Many glands with cancer also have hyperplasia, but no causative link between BPH & cancer has been found. |
|
|
|
Prostatic Adenocarcinoma
|
1. Malignancy of prostatic glandular epithelium (columnar cells become dysplastic)
2. Most common form of cancer in males (#2 is lung cancer) 3. 2nd leading cause of cancer death in males 4. Incidence in the US: 69/100,000 5. Mortality in the US: 41,000 cases/year 6. Occult (“latent”) carcinomas are even more numerous. These are microscopic foci, often found incidentally on needle biopsy and autopsy. i. Effects 20% of males in their 50s, 70% of males 70-80yo ii. No significant research supports whether or not these will become invasive and progress to metastases 7. Most (99%) men with prostate cancer are over the age of 50. 8. African American males - highest rate of adenocarcinoma of the prostate, among 24 countries keeping records. |
|
|
|
Clinical features of prostate cancer
|
1. Most common in posterior lobe which is palpated during DRE
2. Often palpated as an area of firmness 3. Nodules from BPH can mask prostate cancer 4. Involvement of the bladder and/or rectum can mask the true origin of the tumor |
|
|
|
Pathology of prostate cancer
|
1. Almost all prostate malignancies are adenocarcinomas
2. May be more palpable than visible 3. Grow as malignant glands within a fibromuscular stroma i. Differentiation varies from extremely well differentiated (Gleason grade I) to anaplastic (Gleason grade V) |
|
|
|
Prostate cancer
(appearance and etiology) |
1. Etiology is not precisely known [92]
a. Risk factors - age, race, diet (fatty foods), family history, hormonal influence (androgens?), loss of cancer suppressor genes (not p53) 2. Grossly – picture shown in class: same morphology as BPH (spongy, cystic areas) but in posterior lobe, see adenocarcinoma (small solid area 3. Microscopically a. BPH – numerous glands that are two cell layers thick b. Prostatic Intraepithelial Neoplasia (PIN) – transition zone between BPH and adenocarcinoma; precursor to cancer. c. Adenocarcinoma – dark, dysplastic glandular elements with single cell layer |
|
|
|
Grading of prostate cancer – Gleason System
|
1. There are 5 microscopic grades of tumor (I-V) based on architecture pattern and degree of differentiation
2. The 2 most predominant patterns in each prostate are reported 3. Pattern grades (1-5) are added together to give a Pattern Score 4. If only 1 pattern present, it is counted twice for the Pattern Score 5. Extent of tumor within specimen is also noted 6. Pattern Score is very closely related to tumor behavior and prognosis, and therefore also affects treatment 7. Possible Pattern Score range: 2-10 i. 2-4: low grade, good prognosis ii. 5-6: intermediate grade iii. 7: in between intermediate and bad grade iv. 8-10: poorly differentiated, bad grade; cannot be treated, cannot be cured usually associated with lethal prognosis. 8. Clinical Scenario: you, the pathologist, are perusing through a slide of prostate tissue. You notice many different patterns and grade each pattern based on architecture and degree of differentiation. You then add the two highest grades for your Pattern Score. Jenga! |
|
|
|
Gleason Grade I
|
Small, uniform, round, back to back glands
|
|
|
|
Gleason Grade II
|
More space between glands
|
|
|
|
Gleason Grade III
|
Infiltration of cells from glands at margins
|
|
|
|
Gleason Grade IV
|
Irregular masses of cells with few glands
|
|
|
|
Gleason Grade V
|
Lack of glands, sheets of cells seen instead
|
|
|
|
Clinical course of prostate cancer
|
1. . Related to Stage (spread) and Gleason Grade (differentiation)
i. Stage A1 is “incidental carcinoma.” ii. Stage A2 is also a localized form of cancer, but it either affects > 5% of the biopsy specimen or it contains foci that are a high Gleason Grade (IV +). iii. Stage B is a palpable, macroscopic tumor iv. Stage C tumors have extended through the prostatic capsule to the epididymis, scrotum, testes, bladder, or rectum NT Note: Stage C --> capsule v. Stage D is metastatic disease; typically to peri-iliac lymph nodes, axial skeleton bone NT Note: Stage D --> distant |
|
|
|
Stage A1
|
1. "incidental carcinoma.”
2. The cancer focus is microscopic and localized to a small area (< 5%) of the biopsy specimen - This suggests an indolent cancer with a benign course • This is found in > 70% of men over the age of 80 • 5 – 25% of these cases can progress to either local or distant spread, especially in younger men |
|
|
|
Stage D
|
1. metastatic disease; typically to peri-iliac lymph nodes, axial skeleton bone
2. Most testicular tumors, even Stage D, can be cured with aggressive chemotherapy, resection or radiation – with the exception of pure choriocarcinomas. 3. Also important to note: once these tumors spread, they can differentiate and de-differentiate randomly into either more malignant or more benign counterparts. |
|
|
|
Diagnosis of prostate cancer
|
1. Biopsy
2. CT - 3. X-rays 4. Serum Tumor Marker – Prostate Specific Antigen (PSA) |
|
|
|
Biopsy
|
1. transurethral is the most common method but it can also be done transrectally
2. Sextant biopsy - 6 specimens from all different zones are taken; required protocol for LSU |
|
|
|
CT
|
1. abdomen & pelvis to assess the extent of the tumor & nodal involvement
2. Lymph node metastasis is poorly visualized in CT/MRI; most are diagnosed by biopsy and autopsy |
|
|
|
X-rays
|
1. search for metastatic disease in bone
2. Osteoblastic metastases – lytic lesions |
|
|
|
PSA
|
i. Allows monitoring of diagnosed disease
ii. Used with DRE to screen for prostate cancer b. Prostate specific antigen (PSA) is a glycoprotein produced by prostatic glandular columnar epithelium. [104] i. Produced by benign and malignant cells ii. Therefore, PSA is “organ-specific” but not “cancer-specific.” • PSA directs you to the function of the prostate, but since it is produced in benign cells, cannot direct you necessarily to malignancy iii. Normal serum level is < 4 ng/ml • Can be slightly higher in advanced BPH, following DRE or other manipulations • Older men have a naturally higher PSA level (maybe up to 8 – 9 ng/ml since many elderly men have BPH) • On the other hand, some men may have serum levels under 4 ng/mL but still present with symptoms of disease. Follow changes in PSA levels every 1.5 to 2 years in these men, especially if they are young (prostate cancer is more aggressive in younger men) to distinguish symptoms that are caused by cancer vs BPH. |
|
|
|
PSA Uses
|
• Monitoring of diagnosed CA of prostate
1. Serial measurements before and following treatment and long term (watch out for increased levels following treatment – may indicate metastasis) 2. In pts with prostate CA, PSA usually increases 0.75/yr • Screen in conjunction with DRE for prostate CA • Aid to diagnosis of metastatic disease otherwise not identified 1. Very high PSA levels strongly suggestive of metastatic prostate CA (to the levels of 100 to 1000 ng/mL even) |
|
|
|
PSA histopathology
|
1. presence of PSA identifies tissue as prostatic, but can’t distinguish benign from malignant
• Must use H&E appearance to diagnose malignancy • 34BetaE12/PSA Immunostains: 34BetaE12 is specific to basal cells and E-cadherins. Therefore, it can be used to determine the presence or absence of a basal cell layer when you just can’t tell on H&E - if you see glands without this basal cell layer, consider malignancy |
|
|
|
Congenital Anomalies of the Bladder
|
A. Diverticulae
B. Exstrophy |
|
|
|
Diverticulae
|
1. A pouch like eversion or evagination of the bladder wall
2. May be congenital but are more often acquired due to persistent urethral obstruction 3. Diverticulae predispose to infection and to formation of bladder caliculi. a. Urinary stasis always increases chances of infection, and chronic infections increase chances of dysplasia. |
|
|
|
Congenital diverticula
|
caused by a failure of development of normal musculature of the bladder wall
|
|
|
|
Acquired diverticula
|
1. often associated with prostatic enlargement, causing compression of the ureter and obstruction of flow.
2. Pressure increases in the bladder and this causes enlargement. 3. This causes the bladder to enlarge and stretches the walls, leading to some thin, weaker areas which will ballon out and form diverticulae. 4. They are often multiple. |
|
|
|
Exstrophy
|
1. Due to developmental failure in the abdominal wall and the anterior bladder wall. The bladder either communicates directly with the exterior through the wall defect, or lies as an opened sac.
2. The internal surface of the mucosal lining of the bladder is exposed, so this also predisposes to infection, and dysplasia if not treated. (See Fig 21-3 in Robbins for a picture). 3. Can be surgically corrected. |
|
|
|
Inflammation of the Bladder
|
Cystitis
|
|
|
|
Cystitis
(causes) |
1. Caused by a variety of agents: infections, chemicals, chemotherapy, radiation therapy
2. Most cases of cystitis are due to bacteria, commonly gram negative rods: E. coli, Proteus, Klebsiella, and Enterobacter. 3. TB and Candida are seen causing cystitis in immune-compromised patients. Schistosomes are a frequent cause of cystitis in the Middle East. Mycoplasma and Chlamydia are also culprits in rare cases. 4. Radiation therapy and chemortherapy are often associated with hemorrhagic cystitis |
|
|
|
Cystitis
(defined) |
1. a non-specific acute or chronic inflammation;
2. it’s typically seen as hyperemia of the mucosa, with or without an exudate. |
|
|
|
Suppurative cystitis
|
there is a lot of inflammatory exudate and pus lining mucosal surface
|
|
|
|
chronic cystitis
|
1. caused by persistent infection
2. causes heaped up epithelium due to constant irritation, 3. may in some cases lead to fibrosis and scarring |
|
|
|
Follicular cystitis
|
characterized by lots of lymphocytes in the mucosa and some follicles in the subsomusa.
|
|
|
|
Eosinophilic cystitis
|
when eosinophils and giant cells are predominant
|
|
|
|
predispositions to cystitis
|
1. Urinary retention and urinary calculi predispose patients to cystitis.
2. Females are more prone to develop cystits because they have shorter ureters. 3. In males, it’s mostly seen later in life secondary to prostatic enlargement causing urinary stasis. 4. (Diabetes, foreign objects such as catheters, and immune deficiency also increases chances of cystitis- Robbins |
|
|
|
cystitis - triad of symptoms
|
1- Urinary Frequency
2- Lower Abdominal Pain localized over the bladder and 3- Dysuria – pain or burning on urination. ***There may also be systemic signs of inflammation: fever, chills, malaise etc. in severe cases. |
|
|
|
Interstitial Cystitis
|
1. A persistent painful form of chronic cystitis, associated with inflammation and fibrosis of all layers of the bladder walls.
2. More common in females, especially older femailes. 3. Clinically this condition presents with extreme suprapubic pain accompanied by frequency, urgency, and often hematuria. 4. The cause is unknown and suspected to be autoimmune. 5. Positive bacterial cultures rule out this diagnosis – it’s not caused by bacteria. 6. hunner's uclers - multifocal mucosal ulcers that can be seen grossly 7. Microscopically there are acute inflammatory cells, granulation tissue, fibrosis and maybe even giant cells. 8. Mast cells are often present too, although their function here isn’t really clear. 9. When you see these ulcers, you need to make sure to exclude carcinoma. |
HI = hunner's ulcers - interstitial cystisis
|
|
|
Malakoplakia
|
1. Another form of chronic inflammation that is seen in the bladder and is also seen elsewhere in the body, including kidney, colon, lungs, bone, prostate and epidydimus.
2. Characterized by a specific pattern of vesical inflammatory reaction with soft raised yellow plaques and infiltration of large foamy macrophages, multinucleate giant cells and some lymphocytes. a. Mineralized concretions of calcium in the macrophages are called Michaelis-Gutmann bodies and are typical of Malakoplaia; seen both in macrophages and extracellularly between cells. b. See Figure 21-4, 21-5 in the book for pictures 3. Malakoplakia is clearly related to chronic bacterial infection, most commonly E. coli and Proteus. |
|
|
|
Metaplastic Lesions of the Bladder
|
1. Cystitis Glandularis
2. Cystitis Cystica 3. Squamous Metaplasia 4. Nephrogenic Metaplasia |
|
|
|
Cystitis Glandularis and Cystitis Cystica
|
1. Brunn nests (nests of transitional epithelium that grown downward and get trapped in the lamina propria)- Common lesions of the bladder
2. The central cells in these nests then transform into Cystitis Glandularis or Cystitis Cystica 3. These two processes often coexist. 4. They are common incidental findings in normal bladders and are NOT associated with the development of cancer. 5. They usually resolve |
|
|
|
Cystitis Glandularis
|
glandular cuboidal or columnar lining of the nest
|
|
|
|
Cystitis Cystica
|
urothelium lining the nest filled with cystic spaces of clear fluid
|
|
|
|
Squamous Metaplasia
|
1. Usually occurs in response to injury, most commonly seen in extrophy.
2. Urothelium converts to squamous epithelium, and can even progress to a having a keratin lining. |
|
|
|
Nephrogenic Metaplasia
|
1. A reaction of urothelium to injury where urothelium may be replaced by cuboidal epithelium and assume a papillary growth pattern.
2. May mimic carcinomas |
|
|
|
Neoplasms of the Bladder
|
1. 95% of bladder tumors have an epithelial origin, mostly urothelium but can be squamous cell carcinoma or glandular adeoncarcinoma. Diagnostics are improving, but the incidence is also rising worldwide.
2. Urothelial Cell Tumors / Transitional Cell Tumors (urothelium = transitional cell epithelium) 1. Range from benign to aggressive and deadly. Many are multifocal by the time the patient presents, and are most commonly seen in the bladder but keep in mind they can be anywhere there is urothelium (from the renal pelvis at the kidney to the distal urethra). 2. Two distinct precursor lesions lead to invasive urothelial carcinoma: a. Non Invasive Papillary Tumors – exophytic, finger like projections (more to come below) b. Carcinoma in Situ – high grade by definition – a flat nodular lesion 3. Invasion all the way to the muscularis propria (which in the bladder is the detrusor muscle) is associated with 50% 5-year mortality rate. Generally, deeper invasion means worse prognosis. 4. The gross patterns of urothelial cell tumors may be papillary, nodular, or flat; invasive or non invasive. |
|
|
|
Papillary Tumors
|
1. Papillary lesions are red elevated lesions that can be up to 5 cm. There may be multiple separate tumors with the bladder from different origins.
2. Papillary tumors range from benign to invasive, but the majority are low grade. 3. Most papillary tumors arise from the lateral or posterior walls at the base of the bladder. |
|
|
|
Papillary Tumors (Types)
|
1. Papillomas:
2. Papillary Ureothelial Neoplasms of Low Malignant Potential – PUNLMP 3. Low grade Papillary Urothelial Carcinomas 4. High grade Papillary Urothelial Carcinomas |
|
|
|
Papillomas
|
1. Rare,
2. 1 % of bladder tumors, 3. mostly seen in young patients. 4. These are usually single and small, and are covered by urothelium that is histologically identical to normal urothelium. 5. These are typically exophytic (sticking out) but they may also be inverted and go all the way down to the lamina propria. 6. Rarely recur, easily removed. Fig 21 -8 |
|
|
|
Papillary Ureothelial Neoplasms of Low Malignant Potential – PUNLMP
|
1. Similar to papillomas, but these tend to be larger with a thicker urothelium cover and may have diffuse nuclear enlargement.
2. (these are a step up from papillomas with more dysplasia) 3. Mitotic findings are rare 4. though these may recur, they are not associated with invasion |
|
|
|
Low grade Papillary Urothelial Carcinomas
|
1. Characterized by a structurally and cytologically ordered appearance: cells maintain polarity, are evenly spaced, and look cohesive.
2. There is a minimal but definitive amount of nuclear atypia in the form of scattered hyperchromiatic nuclei, nuclear size and shape variation, and mitotic figures. 3. Low grade cancers can recur and although they can invade, its rare. 4. Usually these are not life threatening, but are hard to pick up on cytology because the cohesive cells typically aren’t shed into the urine |
|
|
|
High grade Papillary Urothelial Carcinomas
|
1. Now we see typical malignant features: non cohesive cells with loss of polarity, large hyperchromatic nuclei, weird mitotic figures, and anaplasia.
2. Higher risk of invasion through the muscular layer, and frequently these metastasize. 3. Since these cells are non cohesive, they shed into the urine and can be picked up on cytology. Fig 21 – 10 4. Generally, less than 10 % of the low grades tumors are going to be invasive, while over 80 % of high grade tumors will grow down through the muscle layer. 5. Aggressive tumors can also extend into surrounding organs and may even produce communications into the vagina or rectum via fistulas. 6. 40 % of these invasive tumors spread to the lymph nodes, and hematogenous spread can be prominent in advanced tumors. |
|
|
|
Carcinoma in Situ
|
1. Characterized by a flat urothelium lesion of cytologically malignant cells.
2. These lesions involve the full thickness down to the BM, and may also have a pagetoid spread, which is scattered malignant cells thoughout the urothelium. 3. These lack cohesiveness, so the cells can be seen in the urine. 4. Grossly it usually looks like mucosal redness or thickening, but it’s not going to present as a mass so it may be hard to tell what it is just by cystoscopy (bladder scope). 5. Commonly it’s multifocal and may extend to ureters/urethra. 6. Untreated, up to 75 % will progress to muscle invasion- highly aggressive. |
|
|
|
Invasive Urothelial Cancer
|
1. Invasive lesions develop from papillary origins or from carcinoma in situ.
2. So if detected early, it may be found as a superficial lesion or a carcinoma in situ. 3. Once they pass the lamina proproia (the basement membrane in the bladder) they are considered invasive. 4. Extent of invasion is the most predictive factor of the prognosis, so staging of bladder neoplasms is critical. 5. Grossly a tumor may look papillary, but if it’s really large then assume malignancy |
|
|
|
Pathologic Staging of Bladder Carcinoma
|
1. Ta - noninvasive, papillary
2. Tis - carcinoma in situ; non invasive, flat 3. T1 – lamina propria invasion 4. T2 – muscularis propria invasion 5. T3a - microscopic extravesicle (outside bladder) invasion 6. T3b – grossly apparent extravesicle invasion 7. T4 – invades adjacent structures |
|
|
|
Other types of Carcinomas
|
1. Squamous cell carcinomas of Bladder
2. Mixed urothelial cell carcinoma with area of squamous carcinoma 3. Adenocarcinoma of the Bladder |
|
|
|
Squamous cell carcinomas of Bladder
|
i. 3 -7 % of bladder cancers.
ii. Often associated with schistosomes |
|
|
|
Mixed urothelial cell carcinoma with area of squamous carcinoma
|
i. Usually seen as invasive and fungating;
ii. the level of differentiation can vary widely. iii. It’s rare to find a pure squamous cell or a pure papillary neoplasm; iv. most tumors are actually a mixture but named by the predominant characteristic. |
|
|
|
Adenocarcinoma of the Bladder.
|
i. Rare.
ii. Usually identical to the adenocarcinomas seen in the GI tract. iii. May arise from urachal remnants |
|
|
|
State the location, shape, size, and weight of a normal thyroid gland
|
1. 15-25gm;
2. butterfly shaped, 3. located in the neck below the thyroid cartilage & near the level of the cricoids cartilage |
|
|
|
Discuss the normal regulation of the production & release of thyroid hormones
|
1. Thyroid hormone levels are controlled by the Hypothalamo-Pituitary-Thyroid Axis; whereby TRH → TSH → T3/T4 is the mode of stim & release
2. TSH stim T3/T4 are production via Iodination of Thyroglobulin (by Thyroid Peroxidase, which also readies the Iodine into Iodide) 3. TSH stim releases of T3/4 (by cleavage from Iodinated Thyroglobulin) it than binds Thryoid binding globulin 4. It passes to cells where it works intranuclearly: binding the Thyroid Hormone receptor, which as a complex binds Thyroid Response Elements (TRE) in the genome, thereby upregulating transcription (despite it being a peptide derivative!!!) i. There is hypertrophy of tissue w/ stress, and involution when stress is removed. |
|
|
|
Explain the physiologic means by which goitrogens lead to thyroid enlargement
|
1. Goitrogens inhibit thyroid hormone release into the blood,
2. one mechanism (Iodides) prevent cleavage of throglobulin, thus Iodinated Thyroglubulin continues to be stored in the colloid, and low serum T3/T4 lead to incrd TSH, also promoting proliferation of thyroid tissue |
|
|
|
List and describe 3 broad classifications of thyroid disease
|
1. Hyperthroidism – incrd T3/T4
2. Hypothyroidism – decrd T3/T4 3. Mass Lesions |
|
|
|
State the function of contrast thyrotoxicosis and hyperthyroidism
|
1. Thyrotoxicosis is the hypermetabolic states caused by excess of T3/T4;
2. it is cuased most commonly by hyperfxn of the Thryroid gland itself, 3. thus often used interchangeably w/ Hyperthyroidism; 4. but, it may also be due to incrd release of hormone (Thyroiditis) or even extrthyroidal source (tumor); 5. thus, strictly Hyperthyroidism is only a form of Thyrotoxiciosis |
|
|
|
Thyrotoxicosis Most common causes:
|
1. Diffuse Hyperplasia (eg: Graves),
2. Hyperfxnal Multinodular Goiter, 3. Hyperfxnal Adenoma of Thyroid |
|
|
|
List and discuss the manifestations of elevated thyroid hormone
|
1. Incrd BMR, sweating, warm skin, weight loss, decrd apetitie
2. Cardiovasulcar: Palpatations, Tachy, arryth, even CHF in ptnts w/ previous CHD 3. Neuromuscular: anxious, tremor, hyperactive, proximal muscle weakness, poor concentration, insomnia 4. GI: SNS hypertsim → incr motility, diarrhea, reduced absorption 5. Ocular: exopthalmia 6. Skeletal: incrd bone resorption & osteoporosis (if chronic) 7. Lymphandenopathy 8. Thyroid Storm: abrupt onset of hyperthyroidism; febrile & tachy; occurs due to underlying disease (graves & stress); medical emergency, can die of arrythmia |
|
|
|
List 5 causes of excess thyroid hormone
|
1. Diffuse Toxic Hyperplasia (Graves)
2. Hyperfxning Multinodular Goiter 3. Hyperfxning Thyroid Adenoma 4. Hyperfxning Thyroid Carcinoma 5. Iodine-Induced Hyperthryroidism 6. Neonatal Thyrotoxiciosis assoc w/ Maternal Disease 7. TSH Secreting Pituitary Adenoma (rare; Secondary, others were primary); in this case TSH will be elevated along w/ high T3/T4; others it would be down regulated |
|
|
|
primary hyperthyroidism
|
assoc w/ incrd T3/T4 due to the thyroid
|
|
|
|
secondary hyperthyroidism.
|
assoc w/ incrd T3/T4 due to incrd upreg of thyroid, extrinsic to thyroid
|
|
|
|
Explain the usefulness of TSH as a screening test for hyperthyroidism
|
1. TSH is the best measure as it is lowered (by neg feedback) even in the very early stages of disease; this is assoc w/ an incrd T4/T3 level
2. Follow up w/ radioactive Iodine studies to determine etiology i. Graves: whole gland ii. Adenoma: certain region iii. Thyroiditis: decr uptake, it is spilling of T3/T4 not overprod that is the issue) |
|
|
|
primary hypothyroidism
|
due to failure of the Thyroid itself
|
|
|
|
secondary hypothyroidism
|
due to failure of the Pituirary to make TSH
|
|
|
|
Tertiary hypothyroidism
|
due to failure of the Hypothalamus to make TRH (Rare)
|
|
|
|
major causes of hypothyroidism
|
1. Developmental (throid dysgenesis: due to PAX-8, TFF-2, or TSH receptor mutations
2. Thyroid Hormone reistance syndrome (TR-beta mutation at tissues) 3. Abalative (Qx, Radioactive Iodine, Radiation exposure 4. Autoimmune (Hashimoto’s) 5. Iodine Defic (3rd world countries) 6. Drugs (iodides) 7. Congenital biosynthetic defect in T3/T4 synth 8. Pituitary Defect (secondary) 9. Hypothalamic defect (tertiarty) |
|
|
|
Define & give clinical features of cretinism
|
1. Cretinism is hypothyroidism that develops in infancy or early childhood;
2. may be due to iodine defic or defective synthesis (congenital enzyme defect) 3. Features include: i. impaired development of skeleton & CNS: ii. mental retardation, iii. short stature, iv. coarse fascies, v. protruding tongue, vi. umbilical hernia; vii. degree varies based on maternal levels early (normal is high) & late (normal is low) in pregnancy |
|
|
|
Define & give clinical features of myxedema
|
1. Hypothyroidism occurring in older child or adult; thus, often acquired
2. Features include slowed mental & physical activity; which may be more apparent in child & indolent in adult (long course for clinical suscpicion); other traits are opposite of those seen in Hyperthyroidism along with: edema, coarse features, deepened voice, enlarged tongue, all due to GAG & Hyaluronic Acid deposition 3. →As in Hyperthyroid, TSH levels are also important for diagnosis; it will be high in primary hypo, but low in 2ndry or 3ry |
|
|
|
List the 3 most common & clinically significant forms of thyroiditis
|
a. Hashimoto’s (Chronic Lymphocytic)
b. Subacute Granulomatous c. Subacute Lymphocytic |
|
|
|
List the typical age of onset, male:female ratio, and HLA associations of Hashimoto thyroiditis.
|
1. 45-65yrs,
2. 10:1 or even 20:1 Female:Male; 3. HLA-DR3 & HLD-DR5 |
|
|
|
Describe the association of Hashimoto thyroiditis with other autoimmune disorders
|
1. Individuals with Hashimoto’s have an incrd risk of developing other endocrine (Type I DM) & non-endocrine (SLE, Myesthinia, Sjogren) autoimmune diseases,
2. also an incrd risk of NH-L; 3. no specific link to Thyroid Neoplasms |
|
|
|
List & describe 3 autoantibodies produced by B lymphocytes in Hashimoto thyroiditis
|
a. Three mechanisms of Thryocyte Death (included Ab types)
i. CTL mediated cell death ii. CD4 mediated cytokine relase (INF-g) that activates Macros leading to cell death iii. Anithyroid Ab’s: Anti-TSH Receptor, Anti-Thyroglobulin, Anti-Thyroid Peroxidase • All three lead to Ab-Dependent Cell-mediated Cytotoxicity (ADCC) |
|
|
|
microscopic slide of Hashimoto thyroiditis
|
1. Thyroid gland w/ Lymphoid Follicles (mononuclear cells); atrophic thyroid follicles
2. Hurthle Cells – cells w/ eosinophilic granular cytoplasm 3. Fibrous variants may demonstrate broad, kelloid like fibrosis |
|
|
|
Describe the clinical course and subsequent risk of malignancy of Hashimoto thyroiditis
|
1. Hashimoto’s is characterized by gradual autoimmune destruction of the thyroid gland;
2. most common cause of hypothyroidism where Iodine intake is suffic; 3. it presents painlessly, and initially there is a Thyrotoxicosi (incrd T3/4 & decrd TSH) that eventually progresses to Euthroid, and finally hypothyroid (decrd T3/4 & incrd TSH); 4. there is incrd risk of NH-L, but no certain link to Thyroid Neoplams |
|
|
|
List the typical age of onset and male:female ratio of granulomatous thyroiditis
|
1. 30-50 yrs;
2. 3:1 or 5:1 Female:Male (again women favored) |
|
|
|
Discuss the proposed etiology of granulomatous thyroiditis
|
1. Occurs secondary to antecedent viral infection (cocksackie, mumps, measles, adenovirus), w/ a summer predelection
2. One hypothesis is that viral infection leads to release of an Ag (viral or thyroid is unclear) that leads to CTL mediated attack on thyrocytes (follicular cells); 3. this is in contrast to Auto-immune diseases due to the viral induced component |
|
|
|
State the most common cause of endogenous hyperthyroidism and give its frequency
|
1. Graves Disease is the most common cause of Endogenous Hyperthyroidism
2. It occurs in 1.5-2% of women in US; w/ incrd incidence in families |
|
|
|
List & describe the "Classic triad" of clinical findings in Graves Disease
|
a. Hyperthyroidism (leads to Hyperplasia of thyroid)
b. Opthalmopathy – Exopthalamus c. Dermatopathology – Localized & infiltrative: Pretibial Myxedema in some ptnts |
|
|
|
List the typical age of onset, Male:female ratio, and HLA associations of Graves disease.
|
1. 20-40 yrs;
2. 7:1 Female:Male; 3. HLA-B8 & HLA-DR3; 4. CTLA-4 defects have also been noted (fxn is to reduce response of Tcells to self-ag) |
|
|
|
State the underlying etiology of Graves disease
|
Various Auto-Ab may be present in the serum, most important of which is the TSH Receptor stimulating Ab
|
|
|
|
List 3 autoantibodies demonstrable in Graves disease.
|
*** Auto-Ab’s are targeted at TSH Receptors, Thyroid Peroxidase, & Thyroglobulin; but the ones that are most specific to Graves are those against TSH-R:
i. Thyroid Stimulating Immunoglobulin – stim TSH Receptor, leading to thyroid stim ii. Thyroid Growth Stimulating Immunoglobulin – also stim TSH-R, but here the result is slanted toward prolif of thyroid tissue iii. TSH-Binding Inhibitor Immunoglobulins – bind to TSH-R blocking TSH from binding, but may also stim or inhib at the TSH-R (both types may be present, may be why spont hypothyroidism is seen in Graves also) |
|
|
|
Discuss the spectrum of autoimmune diseases of the thyroid gland
|
1. The Spectrum runs from Graves (hyper) to Hasimoto’s (hypo) at the extremes;
2. in both cases a cross-over may also be demonstrated in their course (Hashitoxicosis in early hashimoto’s & bouts of hypofxn are possible in graves); 3. in either case, there is an apparent genetic link, and some families even demonstrate concurrent Graves & Hashimoto’s in individuals! 4. Both also incr risk of other autoimmune diseases (Type I DM, SLE, Addison’s, Pernicious Anemia, etc) 5. Hitologically there are similarities: intrathryoidal lymphoid infiltrate |
|
|
|
Describe the gross & microscopic features of Graves disease
|
1. >80g; smooth & soft
2. Micro demonstrates too many cells; 3. follicles are hypertrophied, w/ tall columnar epi, scalloped edge colloid, and papillary-like insertions of epithelium into the colloid due to overgrowth; as above, lymphoid infilitrate (T’s, B’s, Plasma) & even germinal centers (as in Hoshimoto’s) 4. eye balls will show edema (due to GAG’s & other mucopoly’s), lympho’s, fibrosis |
|
|
|
Describe the clinical course of Graves disease
|
1. General changes assoc w/ Thyrotoxicosis apply, but also…
2. Hyperplasia of thyroid, Opthalmopathy, Dermatopatholoy (pretibial myxedema) 3. Weakened extraocular muscles due to Exopthalmia; persists even w/ Graves treatment 4. Pretibila Myxedema: thickening, peau d’ organge, induration, slight pigmentation 5. Lab Findings: elevated T3/4 w/ low TSH; incrd & diffuse uptake of Radioactive Iodine 6. Treat w/ abalation of tissue: Qx, Propylthiouracil (a goiterogen), radioiodine to destroy |
|
|
|
Define & explain the significance of "goiter."
|
1. Enlargement of the Thyroid, the most common manifestation of thyroid disease
2. In general, it indicates an impaired synthesis of thyroid hormone (exception is Graves) i. The incrd gland mass compensates for the synthetic deficiency, maintaining Euthyroid state in most (a compensatory hypertrophy & hyperplasia) 3. The compensation may not be suffic in some people, Goitrous Hypothyroidism |
|
|
|
Compare and contrast diffuse (simple) vs. multinodular goiter.
|
1. Diffuse: the goiter formation is diffuse w/in the throid & no nodualrity; assoc Endemic or Sporadic Goiter
2. Multinodular: a. chronic cycles of hyperplasia & involution lead to irregular enlargement of the thyroid; b. arise from diffuse (simple) goiters which recur, c. thus can also be assoc w/ Endemic or Sporadic; d. are assoc w/ the largest goiters, e. and may be confused for neoplasia |
|
|
|
Explain what is meant by the term "endemic goiter."
|
1. Refers to areas where 10% of the population has a goiter related to poor availability of Iodine in the soil, water, & food (mountainous areas like: Alps, Andes, Himalayas)
2. In these areas, Goitrogenic foods (cassava, cabbage, Brussel sprouts, turnips) may exacerbate an Iodine deficiency incring prevalence; 3. due to their ability to alter thyroid hormone synth in various fashions |
|
|
|
Explain the generally accepted theory of development of multinodular goiter
|
1. Develop due to variations in responsiveness to growth factors (eg: trophic hormones, mutations in TSH response pway proteins may be involved) of follicular cells;
2. such that some may have a growth advantage and may even become autonomous (similar to thyroid Adenomas); 3. thus, there are poly & monoclonal nodules; 4. uneven growth may lead to rupture of follicles & vessels, which can create fibrosis & perpetuate a 2nd rupture |
|
|
|
State the condition that gives rise to the most extreme thyroid enlargement
|
Multinodular goiters cause the most extreme thyroid enlargement, often confused for neoplasia
|
|
|
|
Describe the clinical course of goiter
|
1. For Diffuse & Multinodular, a main problem is Mass Effect on the structures of the Neck, Thoracic Outlet, & Mediastinum
2. Most are Euthyroid; a small % of Multinodular may be Hyper or Hypothyroid i. Hyper w/out Opthalmopathology or Dermatopathology 3. In either case, TSH is high in an attempt to maintain a normal T3/4 4. Radioiodine uptake is incrd in “Hot” zones |
|
|
|
Discuss the male:female ratio and clinical significance of a solitary thyroid nodule
|
1. 4:1 Female:Male;
2. it is a palpable mass in otherwise normal thyroid 3. Possibility of neoplasia is a major concern when detected; 4. fortunately the vast majority are non-neoplastic or benign (10:1; benign:malig) |
|
|
|
State the frequency and general overall prognosis of thyroid malignancy
|
1. 1.5% of all cancers in the US (uncommon),
2. well outnumbered (10:1) by adenoms; 3. prognosis is good w/ 90% survival at 20yrs |
|
|
|
Discuss 5 clinical criteria which may provide insight into the nature of a given thyroid nodule
|
1. Solitary nodules – more likely to be neoplastic than multiple nodules
2. Nodules in young – more likely to be neoplastic than older 3. Nodules in males – more likely to be neoplastic than F(despite 4:1 nodule predom) 4. Radiation of Head & Neck – assoc w/ incrd risk 5. Hot Nodules – more likely to be benign than malignant |
|
|
|
Describe the derivation, gross, and microscopic morphology of the typical thyroid adenoma
|
1. Derivation: derived from follicular epithelium, thus aka: Follicular Adenomas
i. →A small portion may produce T3/4 autonomously, ala Multinodular Goiters 2. Gross: grey-white to yellow-brown; encapsulated; can be reminicient of Multinodular Goiter, w/ calcification, hemorrhage, fibrosis, cystic change; normally a single foci & will compress adjacent tissue (both v. Mutli Goiter) 3. Micro: distinct pattern of clonal follicular cells; NO papillary arrange (suggests malig!) |
|
|
|
Describe the clinical & radiographic features of thyroid adenomas.
|
1. Adenomas generally appear as painless on physical exam & possible sx may be dysphagis due to mass effect; possibility of Hyperfxnal or Toxic Adenoma (rare)
2. They take up less Radioactive Iodine = Cold lesions (differ from Multinodular goiter); but, not all cold nodules are adenoma (some may be malignancy, 10%) i. Fine needle aspiration & most importantly surgical specimen is important to diag |
|
|
|
Explain the significance of a "cold" vs. a "hot" thyroid nodule
|
1. Cold Nodules – takes up less Radioactive Iodine than normal tissue, common for adenoma, but 10% may be malignancy
2. Hot Nodules – takes up more Radioactive Iodine than normal tiusse, common for Multinodular Goiter, but not adenoma or malignancy |
|
|
|
Discuss the differential diagnosis of a "solitary" thyroid nodule
|
Greater chance of being a malignancy; diagnosis based on clinical picture, radio studies
|
|
|
|
List & rank by frequency the 4 major subtypes of thyroid cancer
|
1. Papillary Carcinoma – 75-85%, 1 of 3 main papillary metastasizers
2. Follicular Carcinoma – 10-20% 3. Medullary Carcinoma – 5%, cancer of the C-cells 4. Anaplastic Carcinoma – <5%; this is a small fraction that is not well diff (most are) |
|
|
|
List & rank by prognosis the 4 major subtypes of thyroid cancer
|
Worst: Anaplastic>Medullary>Follicular>Papillary
|
|
|
|
List 3 proven or suspected risk factors for cancer of the thyroid.
|
1. Genetics, Radiation Exposure, Long Standing Multinodular Goiter
2. Hashimoto’s assoc w/ Lymphomas, but no connect to follicular epithelial neoplasia yet |
|
|
|
Identify the most common form of thyroid cancer
|
Papillary Carcinoma – which fortunately is also least aggressive
|
|
|
|
List the typical age of onset and risk factors for papillary carcinoma of the thyroid
|
20-40yrs, most commonly assoc w/ exposure to Ionizing radiation
|
|
|
|
Describe the classic microscopic features of papillary carcinoma of the thyroid
|
1. Papillary appearance w/ Fibrovascular core (infiltratring or fairly well delimiting)
2. Clear to Empty look of the nuclei 3. Sammoma Bodies – concentrically calcified structures in lesion; discrim from Follicular or Medullary 4. Lymphatic invasion is common, blood vessel is not |
|
|
|
Discuss the clinical course of papillary carcinoma of the thyroid, including the presentation, scintiscan findings, & prognosis
|
1. Presentation: most are asymp thyroid nodule; may show up as metast to cervical node, but still good prog; mass effect complications if big; possible lung metast
2. Scintiscan: most are “Cold” lesions; Fine needle is also useful 3. Prognosis: 10yr survival 95%; 5-20% recur; 10-15% metast; also depends on Age (>40), extrathyroidal extension & metast |
|
|
|
List the typical age of onset and proposed risk factors for follicular carcinoma of the thyroid.
|
1. 40-50yr old women most common;
2. possibly assoc w/ Nodular Goiters in endemic iodine defic regions; 3. RAS mutations correlate Follicular Adenoma & Carcinoma |
|
|
|
Discuss the clinical course of follicular carcinoma of the thyroid, including the presentation, 2 possible scintiscan findings, & prognosis
|
1. Presentation: slowly enlarging painless nodule; rarely metast to node
2. Scintiscan: most often Cold; but better-diff hyperfxnal lesions appear Warm (rare) 3. Prognosis: 90% survival @ 10 yrs for non-invasive; 50% survival for invasive; thyroidectomy & subseqeunt radio iodine for treatment |
|
|
|
Discuss the significance of a thyroid malignancy presenting as a "hot" nodule
|
This is a hyperfxnal lesion, and thus may lead to Thyrotoxicosis (hyperthyroidism)
|
|
|
|
Identify the thyroid cancer that is a neuroendocrine tumor
|
Medullary Carcinoma, as it is derived from the parafollicular or C-cells; assoc w/ MEN2
|
|
|
|
Identify the most typical secretory product of medullary carcinoma.
|
1. Calcitonin, just as in normal C-cells; note that others are possible (VIP, SS, 5HT)
|
|
|
|
Identify the thyroid malignancy associated with Acellular Amyloid Deposits
|
Medullary Carcinoma
|
|
|
|
Identify the clinical course of medullary carcinoma
|
1. Present as mass in neck, sometimes w/ mass effect;
2. may demonstrate 1st as paraneoplastic syndrome, due to peptides it makes; 3. surprisingly Hypocalcemia is NOT common |
|
|
|
Identify the prognosis of anaplastic carcinoma of the thyroid gland.
|
No effective therapy, almost uniformly fatal, killing w/in a year due to rapid growth & compression of vital neck structures
|
|
|
|
State the most common clinically significant congenital anomaly of the thyroid gland
|
1. Thyroglossal Duct Cysts (presents as: in tongue, full tube, pyramidal lobe, etc)
|
|
|
|
Discuss the clinical significance of thyroglossal duct cysts
|
May be converted into abscess cavities, may rarely demonstrate premalignant potential
|
|
|
|
State the location, shape, size, and weight of normal parathyroid glands, and common deviations from normal.
|
1. Yellow-brown ovoid nodule, weighing 35-40mg each;
2. contain Chief cells which sense Ca & produce PTH |
|
|
|
Discuss the normal regulation of the production & release of parathyroid hormone.
|
1. The Parathyroid is thus under Indy control of any Hypothalamo- axis, FREE (ionized) Ca is sensed, when low it stimulates cleavage & release of PTH (cut from a pre-pro form, with larger active & smaller inactive fractions, of which both may be detected when determining PTH levels)
|
|
|
|
Summarize the metabolic function of parathyroid hormone in supporting serum calcium levels
|
1. PTH binds its 7-TM receptor to activate a G-protein, cAMP pway; this leads to…
i. PTH activation of Osteoclasts ii. Incr in Renal Tubular Ca reab iii. Incr in Renal Tubular Pi excretion iv. Incr in VitD activation at the kidney v. Incr in GI Ca absorption |
|
|
|
Discuss the differential diagnosis of hypercalcemia
|
1. Hyperparathyroidism is one; but most common cause of hypercalcemia is Malignancy
2. Malignancy will present w/ Sx; while Hyperparathyroidism may be silent i. Osteolytic Metast: due to activation of RANK-RANKL pway & Osteoclast axn; • Osteoprotegrin inhib the pway & may be future treatment ii. PTH Related Protein: assoc w/ non-metastatic cancer; PTHrP mimics PTH, but can’t be regulated |
|
|
|
Identify the typical clinical presentation of parathyroid tumors
|
1. Can be Hyper or Hypo fxn;
2. unlike Thyroid, tumors will create effect due to PTH level not Mass effect |
|
|
|
Define primary hyperparathyroidism, and rank 3 etiologies in order of frequency
|
1. One of the most common endocrine disorders; due to an incrd prod &/or secretion of PTH assoc w/ Parathyroid dysfxn
2. Etiology: Adenoma (75-80%) > Primary Hyperplasia (10-15%) > Carcinoma (<5%) |
|
|
|
Describe the criteria of malignancy for parathyroid carcinoma.
|
Invasion & Metastasis are the only reliable criteria; cytologic detail is unreliable
|
|
|
|
Describe the skeletal and renal lesions associated with hyperparathyroidism
|
1. Skeletal:
a. prominence of osteoclasts, they erode bone matrix esp in metaph, lead to incrd osteoblast activ & formation of new widely spaced trabeculae; b. Osteitis Fibrosa Cystica - hemorrhage & cyst formation ); c. Brown Tumor = osteoclasts, hemorrhage, giant cells 2. Renal: nephrolithiasis & nephrocalcinosis (tubule stones) due to Metastatic Calficiation (= systemically induced Ca) |
|
|
|
State the most common manifestation of primary hyperparathyroidism
|
1. An increase in the level of Serum Ionized Ca, which is often caught in blood electrolyte studies prior to any sx = Asymptomatic Hypercalemia (most common cuase)
2. By contrast, malignancy is the most common cause of clinically apparent hypercalcemia |
|
|
|
Describe the serum parathyroid hormone levels in hypercalcemia due to parathyroid disease vs hypercalcemia because of nonparathyroidal factors.
|
1. PTH is elevated in Parathyroid disease,
2. while PTH is quite low in Non-parathyroid disease (due to working neg feedback) |
|
|
|
List & discuss the traditional constellation of symptoms associated with primary hyperparathyroidism.
|
a. Painful bones, Renal Stones, Abdominal Groans, Psychic Moans
i. Bone pain & fracture due to Osteoporosis & Osteitis Fibrosa Cystica ii. Kindey stones, also in chronic may see polyuria & polydypsia iii. Constipation, nausea, peptic ulcer, pancreatitis, gallstones iv. CNS: depression, lethargy, seizure v. Nueromuscular: weakness & fatigure vi. Cardiovascular: aortic & mitral calcifications |
|
|
|
Explain the etiology of secondary hyperparathyroidism; give the most common cause of secondary hyperparathyroidism.
|
1. Anything that leads to reduction in FREE/Ionized serum Ca
2. Renal Failure is most common, which causes reduced Pi excretion, thus Pi binds free Ca, giving an appearance of low Ca to the parathyroid, & thus elevated PTH |
|
|
|
List & discuss 4 causes of hypoparathyroidism
|
a. Surgical: removal of Parathyroid tissue w/ Thryroid Qx, Malignant Neck Mass Qx, Lymph Node Qx, or too much Parathyroid tissue removed for primary Hyperpara
b. Congenital Agenesis: no glands what so ever c. Familial: lack of suffic fxnal gland tissue, assoc w/ APS1 d. Idiopathic: most likely auto-immune, AutoAb to the CASR (Ca Sensing Receptor) |
|
|
|
List and explain the etiology of the clinical manifestations of hypoparathyroidism.
|
a. Tetany – Neuromuscular irritiability due to electrolyte imbalance
b. Mental Status changes, Intracranial Manifestations (parkonsonian-like, incrd ICP), Ocular disease (calcification of lens, yes that’s right), Cardiac condution defects, dental abnormalities esp during development |
|
|
|
Give the hallmark of hypocalcemia
|
Tetany is the hallmark of hypocalcemia
|
|
|
|
Explain Chvostek sign and Trousseau sign
|
a. Chvostek sign – tapping on the facial nerve ilicits contraction of facial mm
b. Trousseau sign – carpal spasm following occlusion of forearm & hand circulation |
|
|
|
Define pseudohypoparathyroidism
|
1. Pseudohypoparathyroidism is a condition caused by resistance to the parathyroid hormone.
2. Patients have a low serum calcium and high phosphate, but the parathyroid hormone level (PTH) is appropriately high. 3. Its pathogenesis has been linked to dysfunctional G Proteins. |
|
|
|
List and describe the 3 types of signaling by extracellularly secreted molecules
|
Autocrine, Paracrine, Endocrine
|
|
|
|
List and describe 3 broad classifications of endocrine disease
|
a. Impaired synthesis or release
b. Abnormal interaction of hormone & target c. Abnormal Reponse by Target d. OR - Overproduction - Underproduction - Mass lesions |
|
|
|
State the location, shape, size, and weight of a normal pituitary gland
|
a. At the infindibulin off of the Hypothalamus, w/in the Sellae Turcia
b. 1cm & about 5gm; pumpking shaped organ |
|
|
|
Recognize a normal pituitary gland grossly and microscopically
|
Three sections (Adeno, Neuro, Intermediate)
|
|
|
|
Identify and describe the function of the 2 components of the pituitary gland
|
a. Adeno is 80% of gland, from Rathke’s pouch (oral ectoderm); it has five cell types
i. Somatotrophs(GH) ii. Lactotrophs (PRL) {both Acidophilic – red} iii. Thyrotrophs (TSH) iv. Corticotrophs (ACTH) v. Gondaotrophs (LH & FSH){all Basophilic – blue} b. Neuro is an extension of the CNS, contains Pituicytes (modified glia), secretion is from the Herring Bodies (Oxytocin & ADH, which are made in Hypothal but released here) |
|
|
|
Discuss the normal regulation of the production & release of pituitary hormones
|
a. Hypothalamus controls Trophic hormone release at the pituitary via Releasing hormones
b. GHRH (+) & SS (-) → GH c. TRH (+) → TSH d. CRH (+) → ACTH e. Dopamine (-) → PRL (only one under strictly negative control) f. GnRH (+) → LH & FSH g. ADH & Oxytocin are released at the Nuerohypophysis from Hypothal via the Hypothalamohypoyseal Tract |
|
|
|
Describe the blood supply of the anterior & posterior pituitary
|
1. Superior Hypohyseal A brings blood to the Primary Plexus,
2. Primary Plexus connects to the Secondary plexus via the Hypohyseal Portal Veins (this whole connection brings blood & releasing hormones to the Adenohypophysis), 3. Inferior Hypophyseal A provides blood to the Neurohypophysis |
|
|
|
List & rank by frequency the 4 main causes of hyperpituitarism
|
1. Adenoma in the anterior lobe
2. Hyperplasia & Carcinoma of Ant Lobe 3. Extrapituitary tumor secretion 4. Hypothalamic disorders |
|
|
|
List & rank by frequency the 4 main causes of hypopituitarism
|
a. Ischemic injury
b. Surgery or radiation c. Inflammatory rxn d. Non-fxnal Adenoma encroaching on normal tissue |
|
|
|
Discuss how a pituitary adenoma may lead too hypopituitarism
|
The Adenoma grows and compresses good tissue, leading to reduced or lost fxn
|
|
|
|
Identify the frequency of incidental pituitary adenomas at autopsy.
|
25% of routine autsopies
|
|
|
|
Identify the percentage of intracranial neoplasms that are pituitary adenomas
|
10% of intracranial neoplasms
|
|
|
|
Define the difference between pituitary microadenoma & macroadenoma.
|
1. Micro <1cm;
2. Macro >1cm |
|
|
|
List & rank by frequency the types of pituitary adenoma
|
a. Pituitary Adenomas are normally Monoconal in origin, but they still may be non-fxnal, monohormonal, plurihormonal (esp GH & PRL together, the two acidophiles)
i. Prolactinoma (20-30%) ii. GH Cell (2nd most common, ?%) iii. Null Cell (20%) = non-fxnal iv. ACTH Cell (10-15%) v. Other Plurihormonal (10%) vi. Gonadotroph Cell (5%) vii. GH/PRL Cell (5%) viii. TSH Cell (1%) |
Please give nancy a puppy. Good girls/probably tease.
|
|
|
State the microscopic criteria that distinguish a pituitary adenoma from non neoplastic anterior pituitary parenchyma.
|
Cellular Monomorphism & the lack of significant Reticulin network disting Adenomas from non-neoplastic ant pituitary parenchyma
|
|
|
|
Identify the classic visual field abnormalities associated with mass lesions in the sells turcica
|
Bitemporal Hemionopsia (lose both temporal fields)
|
|
|
|
Discuss the signs & symptoms associated with pituitary adenomas
|
Associated with:
1. incrd Hormone secretion (type specific) or 2. Mass effect (includes: visual defects, incrd ICP, HYPOpituitarism, hemorrhage assoc w/ pituitary apoplexy, etc) |
|
|
|
List 4 consequences of hyper-prolactinemia
|
1. Amenorrhea,
2. Galactorrhea, 3. Loss of Libido, & 4. Infertility |
|
|
|
Discuss prolactin regulation and give examples of situations that can disrupt normal regulation
|
1. Damage to Dopaminergic neurons in hypothal,
2. damage to pituitary stalk, 3. & Dopamine inhibitory drugs may lead to Hyperprolactinemia due to altered normal regulation |
|
|
|
Acromegally
|
1. occurs due to incrd GH following closure of the growth plates,
2. it is related to incrd growth of facial structures, hands, feet, viscera, & soft tissues |
|
|
|
Gigantism
|
1. occurs due to incrd GH before closure of the growth plates,
2. leading to incrd growth in the long bones & overall body size, but disproportionately long arms & legs |
|
|
|
Explain the pathophysiology of Nelson Syndrome
|
1. the rapid enlargement of a pituitary adenoma that occurs after the removal of both adrenal glands.
2. Removal of both adrenal glands, or bilateral adrenalectomy, is an operation for Cushing's Syndrome. 3. Removal of both adrenals eliminates production of cortisol, and the lack of cortisol's negative feedback can allow any preexisting pituitary adenoma to grow unchecked. 4. Continued growth can cause mass effects due to physical compression of brain tissue, along with increased production of adrenocorticotrophic hormone (ACTH) and melanocyte stimulating hormone (MSH). 5. The common signs and symptoms include a. muscle weakness and b. skin hyperpigmentation due to excess MSH. |
|
|
|
Define “null cell adenoma
|
1. A hormone negative tumor,
2. it does not fxn and has no specific hormonal predilection in a True example; 3. most of today’s Null cells are actually silent Gonadotrophic adenomas |
|
|
|
Explain why patients with null cell adenomas typically present with mass effects
|
b/c there is no way to know it is there until it is of the size where is causes mass effect
|
|
|
|
Give the relative frequency and typical functional status of pituitary carcinoma
|
1. Carcinomas are quite rare,
2. normally non-fxnal, and 3. vary in differentiation; evidence of metast is usually diagnostic |
|
|
|
Explain the concept of functional reserve of the anterior pituitary
|
The idea is that about 75% of the pituitary must be damaged before effects are demonstrated, as there a large degree of redundancy to handle fairly major impedance
|
|
|
|
List and discuss at least 4 causes of hypopituitarism
|
1. Tumor or Other mass lesions – compresses & damages normal pituitary
2. Surgery or Qx – damage to, or removal of pituitary leads to hypofxn 3. Pituitary Apoplexy – sudden hemorrhage, often assoc w/ pituitary adenoma; emergency 4. Ischemic Necrosis/Scheehan Syndrome – DIC, Sickle cell, Incrd ICP, shock, Sheehan Rathke cleft cyst – cyst in adenohypoph 5. Empty Sella Syndrome – anything that damages part of all of pituitary (Qx, etc) 6. Genetic Defects – rare 7. Defects in releasing hormone delivery – trauma, infection/inflammation, tumor |
|
|
|
Define Sheehan syndrome
|
1. assoc w/ necrosis following preg;
2. Hypertrophy and hyperplasia of lactotrophs during pregnancy results in the enlargement of the anterior pituitary, without a corresponding increase in blood supply. 3. Secondly, the anterior pituitary is supplied by a low pressure portal venous system.[1] 4. These vulnerabilities, when affected by major hemorrhage or hypotension during the peripartum period, can result in ischaemia of the affected pituitary regions leading to necrosis. 5. The posterior pituitary is usually not affected due to its direct arterial supply. 6. the most common ischemic cause of hypopituit; |
|
|
|
List and explain at least 5 signs or symptoms of hypopituitarism
|
***. Depends on the Hormone that is reduced:
i. GH – when in children, pituitary dwarfism or just small stature ii. GnRH → LH & FSH – amenorrhea, infertility, decrd libido, impotence (like HyperPRL) iii. TSH & ACTH – lead to Hypothyroid & Hypoadrenal, resp iv. PRL – lack of normal lactation v. MSH – lack of normal melanocyte stimulation, hypopigmentation |
|
|
|
List and give the function of the 2 products of the posterior pituitary
|
1. ADH – H2O balance (reabsorption via AQP-2 placement), as well as vasoconstriction (as it is also known as Vasopression)
2. Oxytocin – uterine contraction, milk ejection; possible assoc w/ social bond (baby-mom) |
|
|
|
Define diabetes insipidus
|
1. ADH deficiency that leads to Polyuria due to the inability of the kidney to properly reabsorb water;
2. discrim lack of prod (central) or lack of response (nephrogenic); 3. get large volumes of dilute urine, hypernatremia & incrd osmolarity which leads to Polydypsia 4. →May be due to head trauma, inflammation, tumor, surgery |
|
|
|
Define Syndrome of inappropriate antidiuretic hormone (SIADH), & give clinical manifestations.
|
1. Excess secretion of ADH leads to excess volume retention & hyponatremia
2. Leads to cerebral edema, incrd total body water, normal BV, but NO peripheral edema! |
|
|
|
List & discuss the 4 most common causes of SIADH
|
1. Ectopic ADH by malignant neoplasm (esp small cell of lung)
2. Non-neoplastic lung disease 3. Local injury to hypothal or neurohypoph |
|
|
|
State the location, shape, size, and weight of a normal adrenal gland.
|
1. Paired endocrine organ on top of the kidneys, looks like triangle
2. 4gm ( weight changes due to lipid depletion—cause weight loss-- or prolonged stress— causes hypertrophy and hyperplasia of the cortical cells which can more than double the weight) 3. gland has a cortex and a medulla 4. layers from outside to medulla(capsule, zona glomerulosa, zona fasciculata, zona reticularis, medulla)—zona fasciculata makes up 75% of the cortex |
|
|
|
List and explain 3 types of steroids produced by the adrenal cortex
|
1. glucocorticoids—which are synthesized primarily in the zona fasciculata with a small contribution from the zona reticularis
2. mineralocorticoids---the most important being aldosterone, which is generated in the zona glomerulosa 3. sex steroids (estrogens and androgens)---which are produced largely in the zona reticularis i. Extra information for completeness: what does the adrenal medulla produce: Has chromaffin cell which synthesize and secrete catecholamines(epinephrine)---allow for rapid adaptations to changes in the environment |
|
|
|
List and discuss 3 distinctive hyperadrenal syndromes
|
1. Hypercortisolism(Cushing Syndrome) ---caused by and condition that produces an elevation in glucocorticoid levels.
2. Hyperaldosteronism---chronic excess aldosterone secretion(excessive levels of aldosterone cause sodium retention and potassium excretion, with resultant hypertension and hypokalemia) 3. Adrenogenital(virilizing syndromes)---caused by excess androgens |
|
|
|
List and discuss 4 distinctive etiologies of Cushing syndrome.
|
1. Administration of exogenous glucocorticoids---most common---exogenous—Iatrogenic
2. Endogenous Cushing syndromes i. Primary hypothalamic-pituitary diseases associated with hypersecretion of ACTH ii. Hypersecretion of cortisol by an adrenal adenoma, carcinoma, or nodular hyperplasia iii. The secretion of ectopic ACTH by a nonendocrine neoplasm |
|
|
|
Primary hypothalamic-pituitary diseases associated with hypersecretion of ACTH
|
1 Most common (70-80% of cases of endogenous Cushing’s)
2. When caused by a pituitary lesion, it’s called CUSHING’S DISEASE. 3. Women>men in twenties and thirties 4. Usually, the pituitary has an ACTH-producing microadenoma 5. Another cause is corticotroph cell hyperplasia in the anterior pituitary 6. Pts have variable degrees of bilateral nodular cortical hyperplasia 7. High cortisol, high ACTH |
|
|
|
Hypersecretion of cortisol by an adrenal adenoma, carcinoma, or nodular hyperplasia
|
1. Responsible for about 10%-20% of cases of endogenous Cushing syndrome
2. It is ACTH-independent Cushing syndrome or adrenal cushing syndrome because the adrenals function autonomously 3. In unilateral neoplasm, the uninvolved adrenal cortex and that in the opposite gland undergo atrophy because of suppression of ACTH secretion 4. Primary cortical hyperplasia is uncommon; usually arise do to a secondary influence 5. Elevated levels of cortisol with Low levels of ACTH |
|
|
|
The secretion of ectopic ACTH by a nonendocrine neoplasm
|
1. Causes 10% of cushing syndrome
2. The tumors responsible are: small cell carcinoma of the lungs, carcinoid tumors, medullary carcinomas of the thyroid, and islet cell tumors of the pancreas 3. Adrenal gland undergoes bilateral cortical hyperplasia 4. Course is often rapid and bad prognosis 5. Most common in men in their 40-50 6. Elevated ACTH |
|
|
|
Discuss ACTH levels and adrenal morphology in the 4 distinctive etiologies of Cushing Syndrome
|
1. Administration of exogenous glucocorticoids
2.. Primary hypothalamic-pituitary diseases associated with hypersecretion of ACTH 3. Hypersecretion of cortisol by an adrenal adenoma, carcinoma, or nodular hyperplasia 4. The secretion of ectopic ACTH by a nonendocrine neoplasm |
|
|
|
Administration of exogenous glucocorticoids
|
i. Low ACTH production due to outside source of glucocoticoids being ingested
ii. Causes bilateral cortical atrophy due to a lack of stimulation of the zona fasciculata and reticularis by ACTH---zona glomerulosa is of normal thickness because this portion of the cortex functions independently of ACTH |
|
|
|
Primary hypothalamic-pituitary diseases associated with hypersecretion of ACTH
|
i. High cortisol, high ACTH
ii. Adrenal hyperplasia (diffuse hyperplasia) |
|
|
|
Hypersecretion of cortisol by an adrenal adenoma, carcinoma, or nodular hyperplasia
|
i. Elevated levels of cortisol with Low levels of ACTH
ii. Nodular hyperplasia |
|
|
|
The secretion of ectopic ACTH by a nonendocrine neoplasm
|
i. Elevated ACTH
ii. Adrenal hyperplasia (diffuse hyperplasia) |
|
|
|
Define Cushing disease.
|
a. Cushing's disease specifically refers to a tumor in the pituitary gland that stimulates excessive release of cortisol from the adrenal gland by releasing large amounts of ACTH
|
|
|
|
State the characteristic clinical manifestations of Cushing syndrome
|
1. Develops slowly
2. Early stages: hypertension and weight gain 3. Later stages: see central pattern of adipose tissue deposition---list under major features 4. Major Features: of the later stage i. Truncal obesity ii. moon faces iii. buffalo hump(accumulation of fat in the posterior neck and back) iv. decrease muscle mass and proximal limb weakness(hypercortisolism causes selective atrophy of fast-twitch myofibers) v. Secondary diabetes---hyperglycemia, glucosuria, and polydipsia(glucocorticoids induce gluconeogenesis and inhibit the uptake of glucose by cells) vi. Skin is thin, fragile and easily bruised(catabolic effects on proteins cause loss of collagen) vii. Skin striae(sides of lower abdomen)---“stretch marks” viii. Osteoporosis(catabolic effects on proteins cause resorption of bones) ix. Increased risk for a variety of infections(glucocorticoids suppress the immune response) x. Mental disturbances(mood swings, depression, frank psychosis) xi. Hirsutism(is defined as excessive and increased hair growth in women in locations where the occurrence of terminal hair normally is minimal or absent) xii. Menstrual abnormalities |
|
|
|
diagnosis of Cushing syndrome
|
1. Diagnosed in the lab by looking at:
i. the 24—hour urine free cortisol level, will see increase ii. loss of normal diurnal pattern of cortisol secretion 2. To determine the cause of cushing syndrome depends on: i. level of serum ACTH ii. measurement of urinary steroid excretion after administration of dexamethasone |
|
|
|
Discuss 3 general patterns of diagnosis of Cushing syndrome by ACTH measurement
|
i. Pituitary Cushing Syndrome(most common form)
ii. Ectopic ACTH secretion iii. Adrenal Tumor---causing cushing syndrome |
|
|
|
Pituitary Cushing Syndrome(most common form)
|
1. Low sexamethason dose - ACTH levels are elevated and cannot be suppressed by the administration of a low dose of dexamethasone. There will therefore be no reduction in the urinary excretion of 17-hydroxycorticosteroids.
2 high Dexamthasone dose - ACTH levels are reduced by the pituitary when a high dose of dexamethasone is injected. There will therefore be a suppression of steroid secretion in the urine. |
|
|
|
Ectopic ACTH secretion
|
1. will see elevated level of ACTH, but its secretion is completely insensitive to low or high doses of exogenous dexamethasone
|
|
|
|
Adrenal Tumor---causing cushing syndrome
|
1. ACTH level is quite low due to feedback inhibition of the pituitary
2. Also, low-dose and high-dose dexamethasone fail to suppress cortisol excretion |
|
|
|
Describe the effects of excessive production of aldosterone
|
Excessive levels of aldosterone cause sodium retention and potassium excretion, with resultant hypertension and hypokalemia
|
|
|
|
List & rank in order of frequency 2 causes of hyperaldosterone
|
Primary hyperaldosteronism
i. Caused by: a. Adrenocortical neoplasm(most common), b. Primary adrenocortical hyperplasia “idiopathic hyperaldosteronism”, c. Glucocorticoid- remediable hyperaldosteronism |
|
|
|
Define Conn syndrome
|
1. A solitary aldosterone-secreting adenoma,
2. causes 80% of the primary hyperaldosteronism, 3. seen mostly in middle aged women |
|
|
|
Secondary hyperaldosteronism
|
1. aldosterone release occurs in response to activation of the renin-angiotensin system
2. see increased levels of plasma rennin |
|
|
|
give 4 settings in which secondary hyperaldosteronism occurs
|
i. decreased renal perfusion (arteriolar nephrosclerosis, or renal artery stenosis)
ii. arterial hypovolemia and edema (CHF, cirrhosis, nephrotic syndrome) iii. pregnancy (due to estrogen-induced increases in plasma rennin substrate) |
|
|
|
clinical manifestations of primary hyperaldosteronism
|
1. Hypertension
2. Hypokalemia a. ---Both Hypertension and Hypokalemia impose a burden on the heart which may cause electrocardiographic changes and cardiac decompensation--- |
|
|
|
Hypertension
|
1. caused by sodium retention—
2. increases the total body sodium and expands the extracellular fluid volume, leading to elevation of the serum sodium concentration and an increase in intracellular sodium with increased vascular reactivity |
|
|
|
Hypokalemia
|
1. results from renal potassium wasting
2. can cause a variety of neuromuscular manifestations, including weakness, paresthesias, visual disturbances, and occasionally frank tetany |
|
|
|
Define congenital adrenal hyperplasia
|
1. CAH represents a group of autosomal-recessive, inherited metabolic errors,
2. each characterized by a deficiency or total lack of a particular enzyme involved in the biosynthesis of cortical steroids, particularly cortisol. |
|
|
|
CAH Morphology
|
1. in all cases of CAH, the adrenals are bilaterally hyperplastic,
2. sometimes expanding to 10to 15 times their normal weights because of the sustained elevation in ACTH. 3. The adrenal cortex is thickened and nodular, 4. and on cut section, the widened cortex appears brown, owing to total depletion of all lipid. 5. The proliferating cells are mostly compact, eosinophilic, lipid-depleted cells, intermixed with lipid-laden clear cells. 6. Hyperplasia of corticotroph cells is present in the anterior pituitary in most CAH patients. |
|
|
|
CAH and steroidogenesis
|
1. Steroidogenesis is then shunted to other pathways, leading to excess androgen production, which accounts for virilization.
2. Deficiency of cortisol leads to high ACTH, which can also cause adrenal hyperplasia. 3. The virilizing syndrome may also be associated with salt wasting, which can be life-threatening. |
|
|
|
21-hydroxylase deficiency
|
1. accounts for >90% of congenital adrenal hyperplasia
|
|
|
|
salt wasting syndrome
|
1. total loss of 21-hydroxylase
2. because the patient can’t convert progesterone into deoxycorticosterone into corticosterone into aldosterone and finally into mineralocorticoids, which means no mineralocorticoids. 3. This comes to light very soon after birth as acidosis, hypotension, cardiovascular collapse, and possibly death |
|
|
|
There are varying degrees of virilization
|
1. Males are generally unrecognized at birth, but the salt wasting syndrome will show up 5-15 days after birth
2. Less than total deficiency leads to simple virilizing adrenogenital syndrome without salt wasting, which presents as genital ambiguity |
|
|
|
CAH continued
|
1. Onset of clinical symptoms depends on the nature and severity of the enzyme defect.
2. It can manifest anytime from the perinatal period to adulthood. 3. This should be suspected in any newborn with ambiguous genitalia 4. Treated with glucocorticoids, and mineralocorticoids for salt-wasting syndrome |
|
|
|
Primary adrenal insufficiency
|
---(primary hypoadrenalism)
i. Loss of cortex due to: 1. CAH 2. Adrenoleukodystrophy 3. Autoimmune adrenal insufficiency 4 Infection(acquired immune deficiency syndrome, TB, fungi, acute hemorrhagic necrosis) 5. Amyloidosis, sacoidosis, hemochromatosis ii. Metabolic failure in hormone production: • Congenital adrenal hyperplasia (cortisol and aldosterone deficiency with virlization) • Drug and steroid-induced inhibition of adrenocorticotropic hormone or cortical cell function |
|
|
|
Secondary adrenal insufficiency
|
---(decreasing stimulation of the adrenals due to deficiency of ACTH)
i. Hypothalamic pituitary disease due to: • Neoplasm, inflammation(sarcoidosis,TB, pyogens, fungi) ii. Hypothalamic pituitary suppression due to: • Long-term steroid administration • Steroid-producing neoplasm’s |
|
|
|
Acute adrenal insufficiency(adrenal crisis)
|
i. Occur as a crisis in patients with chronic adrenocortical insufficiency precipitated by and form of stress that requires an immediate increase in steroid output form glands incapable of responding
ii. Can be seen in patients who receive exogenous corticosteroids, in whom rapid withdrawal of steroids or failure to increase steroid doses in response to an acute stress may precipitate and adrenal crisis: because the adrenal gland is atrophic and not producing glucocorticoid hormones iii. As result of massive adrenal hemorrhage, which destroys the adrenal cortex sufficiently to cause acute adrenocortical insufficiency(see in newborns following delivery trauma, patients on anticoagulant therapy, and some bacteremic infections---Waterhouse-Friderichsen Syndrome) |
|
|
|
Chronic adrenal insufficiency(Addison Disease)
|
i. Uncommon disorder resulting from progressive destruction of the adrenal cortex.
ii. More common in white women. iii. Four main causes (90% of Addison Disease): autoimmune adrenalitis, TB, AIDS, and Metastatic cancers iv. Addisons begins insidiously and is not seen until 90% of the cortex of both glands is destroyed and the levels of circulation glucocorticoids and mineralocorticoids are significantly decreased |
|
|
|
Four main causes of addison's disease
|
• Autoimmune adrenalitis (most common)
1. Autoimmune polyendocrine syndrome type 1 2. Autoimmune polyendocrine syndrome type 2 3. Isolated autoimmune Addison disease • Infections(TB and AIDS) • Metastatic cancers(from lung and breast) • Genetic disorders of adrenal insufficiency |
|
|
|
Addison's Disease - clinical findings - initially
|
1. progressive weakness and easy fatigability
2 Later: GI disturbances, hyperpigmentation of the skin 3. May see:hyperkalemia, hyponatremia, volume depletion, and hypotension |
|
|
|
Define adrenal crisis and Addison disease
|
a. Adrenal Crisis: is a constellation of symptoms that indicate severe adrenal insufficiency
b. Addison disease: uncommon disorder resulting from progressive destruction of the adrenal cortex |
|
|
|
Give 4 examples of etiology of acute adrenal insufficiency
|
a. Drug and steroid-induced inhibition
b. Infection c. Acute hemorrhagic necrosis d. Chronic adrenocortical insufficiency precipitated by any form of stress that requires immediate increase in steroid output from glands incapable of responding |
|
|
|
Define & discuss Waterhouse-Friderichsen syndrome.
|
1. When massive adrenal hemorrhage complicates a bacteremic infection
2. This is uncommon but is a catastrophic syndrome if results: i. an overwhelming bacterial infection(Neisseria meningitides septicemia, Pseudomonas, Haemophilus influenza) ii. rapidly progressive hypotension leading to shock iii. disseminated intravascular coagulation with widespread purpura, particularly of the skin iv. rapidly developing adrenocortical insufficiency associated with massive bilateral adrenal hemorrhage 3. Most Common in children 4. Adrenals are converted to sacs of clotted blood virtually obscuring all underlying details. |
|
|
|
Waterhouse-Friderichsen syndrome - histo and treatment
|
1. Histologically: hemorrhage starts within the medulla in relationship to thin-walled venous sinusoids, then suffuses peripherally into the cortex, often leaving islands of recognizable cortical cells (Figure 24-50 on p. 1215)
2. TX: treat promptly with antibiotics---problem: clinical course is devastatingly abrupt and without treatment within hours to a few days death will occur |
|
|
|
Discuss the concept of functional reserve of the adrenal gland
|
In chronic adrenocortical insufficiency the adrenal cortex is able to be 90% compromised before clinical manifestations appear
|
|
|
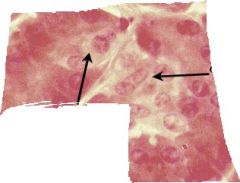
List 3 causes of chronic adrenal insufficiency
|
a. Autoimmune adrenalitis
b. Infection(TB, AIDS) c. Metastatic cancer |
|
|
|
List the 2 most common sources of metastatic cancer to the adrenal gland.
|
a. Lung
b. Breast |
|
|
|
Define secondary adrenal cortical insufficiency
|
1. Any disorder of the hypothalamus and pituitary, such as metastatic cancer, infection, infarction, or irradiation, that reduces the output of ACTH leading to a syndrome of hypoadrenalism
|
|
|
|
Give 4 settings in which secondary adrenal cortical insufficiency can occur.
|
1. Hypothalamic pituitary disease
i. Neoplasm ii. inflammation(sarcoidosis, TB, pyogens, fungi) 2. Hypothalamic pituitary suppression i. long-term steroid administration ii. Steroid-producing neoplasm’s |
|
|
|
Explain why hyperpigmentation may be a feature of primary adrenal insufficiency but not secondary adrenal insufficiency.
|
a. With secondary disease, the hyperpigmentation of primary Addison disease is lacking because melanotropic hormone levels are low
b. MSH is released by the pituitary |
|
|
|
Explain why hyponatremia & hyperkalemia may be features of primary adrenal insufficiency but not secondary adrenal insufficiency.
|
1. Secondary hypoadrenalism is characterized by deficient cortisol and androgen output but normal or near-normal aldosterone synthesis.
2. Therefore, in adrenal insufficiency secondary to pituitary malfunction, marked hyponatremia and hyperkalemia are not seen |
|
|
|
Describe the role of ACTH administration in distinguishing primary vs. secondary adrenal hypofunction.
|
1. The difference between primary and secondary adrenal hypofunction can be seen on how they respond to exogenous ACTH. Either increase plasma cortisol levels or do not increase plasma cortisol levels in response.
2. Primary disease: because of the destruction of the adrenal cortex, there is no response to exogenously administered ACTH in the form of increased plasma levels of cortisol 3. Secondary hypofunction: upon administering ACTH there is a prompt rise in plasma cortisol levels |
|
|
|
State the method of determining the functional status of an adrenal neoplasm
|
1. Determining whether an adrenal neoplasm is functional or not is based on clinical evaluation and measurement of the hormone or its metabolites in the laboratory.
2. Functional and nonfunctional adrenocortical neoplasms cannot be distinguished on the basis of morphologic features. |
|
|
|
Describe the cellular composition of the normal adrenal medulla
|
1. The adrenal medulla is developmentally, functionally, and structurally distinct from the adrenal cortex.
2. It is composed of specialized neural crest (neuroendocrine) cells, termed chromaffin cells, and their supporting (sustentacular) cells. 3. The chromaffin cells are round to oval, have prominent cytoplasmic membrane-bound granules of stored catecholamines, and are supported by a richly vascularized scant stroma of spindled and sustentacular cells. 4. These cells, so named because of their brown-black color after exposure to potassium dichromate (ex: Zenker fixative), synthesize and secrete catecholamines in response to signals from preganglionic nerve fibers in the sympathetic nervous system. |
|
|
|
State the major products of the adrenal medulla
|
1. The adrenal medulla is the major source of catecholamines (epinephrine, norepinephrine) in the body.
2. Norepinephrine functions as a local neurotransmitter, chiefly of sympathetic postganglionic neurons. Only small amounts reach the circulation. 3. Epinephrine (adrenaline) is secreted into the vascular system and interacts with α and β adrenergic receptors in various cells. 4. Because the secretory cells are part of the neuroendocrine system, they are also capable of synthesizing a variety of bioactive amines and peptides, such as histamine, serotonin, renin, chromogranin A, and neuropeptide hormones. |
|
|
|
Describe the distribution of the neuroendocrine system
|
1. Neuroendocrine cells similar to chromaffin cells are widely dispersed in an extra-adrenal system of clusters and nodules that, together with the adrenal medulla, make up the para-ganglion system.
2. These extra-adrenal paraganglia are closely associated with the autonomic nervous system and can be divided into three groups based on their anatomic distribution: (1) branchiomeric (2) intravagal, and (3) aorticosympathetic. 3. The branchiomeric and intravagal paraganglia associated with the parasympathetic system are located close to the major arteries and cranial nerves of the head and neck and include the carotid bodies. The intravagal paraganglia, as the term implies, are distributed along the vagus nerve. 4. The aorticosympathetic chain is found in association with segmental ganglia of the sympathetic system alongside the abdominal aorta. The organs of Zuckerkandl, close to the aortic bifurcation, belong to this group. |
|
|
|
Describe the 2 classes of neoplasms of the adrenal medulla
|
1. The most important diseases of the adrenal medulla are neoplasms, which include:
2. neoplasms of chromaffin cells (pheochromocytomas) and 3. neuronal neoplasms (including neuroblastomas and more mature ganglion cell tumors). |
|
|
|
Define pheochromocytoma
|
1. Pheochromocytomas are uncommon neoplasms composed of chromaffin cells, which synthesize and release catecholamines and in some instances peptide hormones.
2. These tumors are important because they (similar to aldosterone-secreting adenomas) give rise to surgically correctable forms of hypertension. 3. Although a minute percentage of hypertensive patients have an underlying pheochromocytoma, the HTN can be fatal when the tumor goes unrecognized. 4. Occasionally, one of these tumors produces other steroids or peptides and so may be associated with Cushing syndrome or some other endocrinopathy. |
|
|
|
List the most common locations of pheochromocytoma.
|
1. The best answer (based on several sources, including the textbook), seems to be the Adrenal Medulla as the term “Pheochromocytoma” refers specifically to Chromaffin tumors of the adrenal.
2. Thus, technically, a Chromaffin tumor in any other location is NOT a Pheochromocytoma, but a Paraganglionoma |
|
|
|
Pheochromocytomas usually subscribe to a convenient "rule of 10s":
|
i. 10% of pheochromocytomas arise in association with one of several familial syndromes These include the MEN-2A and MEN-2B syndromes, type I neurofibromatosis, von Hippel-Lindau syndrome, and Sturge-Weber syndrome.
ii. 10% of pheochromocytomas are extra-adrenal, occurring in sites such as the organ of Zuckerkandl and the carotid body, where these chromaffin-negative tumors are usually called paragangliomas to distinguish them from pheochromocytomas. iii. 10% of nonfamilial adrenal pheochromocytomas are bilateral iv. 10% of adrenal pheochromocytomas are biologically malignant v. 10% of adrenal pheochromocytomas arise in childhood, usually the familial subtypes, and with a strong male preponderance. The nonfamilial pheochromocytomas most often occur in adults between 40 and 60 years of age, with a slight female preponderance |
|
|
|
Describe the typical histological appearance of pheochromocytoma
|
1. The histologic pattern in pheochromocytoma is quite variable.
2. The tumors are composed of polygonal to spindle-shaped chromaffin cells or chief cells, clustered with the sustentacular cells into small nests or alveoli (zellballen) by a rich vascular network. 3. The cytoplasm has a finely granular appearance, best demonstrated with silver stains, owing to the appearance of granules containing catecholamines. 4. The nuclei are usually round to ovoid, with a stippled "salt and pepper" chromatin that is characteristic of most neuroendocrine tumors. 5. Electron microscopy reveals variable numbers of membrane-bound, electron-dense granules, representing catecholamines and sometimes other peptides. |
|
|
|
Describe the criteria for diagnosis of malignancy in pheochromocytoma
|
1. There is no single histologic feature that can reliably predict clinical behavior in pheochromocytomas.
2. Tumors with "benign" histologic features may metastasize, while bizarrely pleomorphic tumors may remain confined to the adrenal gland. 3. In fact, cellular and nuclear pleomorphism, including the presence of giant cells, and mitotic figures are often seen in benign pheochromocytomas, while cellular monotony is paradoxically associated with an aggressive behavior. Even capsular and vascular invasion may be encountered in benign lesions. 4. Therefore, the definitive diagnosis of malignancy in pheochromocytomas is based exclusively on the presence of metastases. These may involve regional lymph nodes as well as more distant sites, including liver, lung, and bone. 5. Several histologic features, such as numbers of mitoses, confluent tumor necrosis, and spindle cell morphology, have been associated with an aggressive behavior and increased risk of metastasis, but in and of itself, no single criterion is entirely reliable. |
|
|
|
State the dominant clinical feature of pheochromocytoma
|
a. The dominant clinical feature in patients with pheochromocytoma is hypertension.
b. Classically, this is described as an abrupt, precipitous elevation in blood pressure, associated with tachycardia, palpitations, headache, sweating, tremor, and a sense of apprehension. c. These episodes may also be associated with pain in the abdomen or chest, nausea, and vomiting. The paroxysms may be precipitated by emotional stress, exercise, changes in posture, and palpation in the region of the tumor. d. The elevations of pressure are induced by the sudden release of catecholamines that may acutely precipitate congestive heart failure, pulmonary edema, myocardial infarction, ventricular fibrillation, and cerebrovascular accidents. |
|
|
|
Describe the laboratory diagnosis of pheochromocytoma
|
1. The laboratory diagnosis of pheochromocytoma is based on the demonstration of increased urinary excretion of free catecholamines and their metabolites, such as vanillylmandelic acid (VMA) and metanephrines.
|
|
|
|
Paragangliomas
|
*** Pheochromocytomas that develop in paraganglia other than the adrenal medulla are often designated paragangliomas.
i. Paragangliomas may arise in any organ that contains paraganglionic tissue. ii. The carotid body tumor is a typical paraganglioma, forming a palpable mass in the neck enveloping the carotid vessels. iii. Paragangliomas are uncommon and occur about one tenth as frequently as adrenal pheochromocytomas. |
|
|
|
Chemodectomas -
|
Tumors originating in the jugulotympanic body are sometimes referred to as chemodectomas because these paraganglia sense the oxygen and carbon dioxide levels of the blood.
|
|
|
|
Summarize the features of the Multiple Endocrine Neoplasia (MEN) syndromes
|
1. The multiple endocrine neoplasia (MEN) syndromes are a group of genetically inherited diseases resulting in proliferative lesions (hyperplasia, adenomas, and carcinomas) of multiple endocrine organs.
2. Like other inherited cancer disorders, endocrine tumors arising in the context of MEN syndromes have certain distinct features that contrast with their sporadic counterparts: i. These tumors occur at a younger age than sporadic cancers. ii. They arise in multiple endocrine organs, either synchronously (at the same time) or metachronously (at different times). iii. Even in one organ, the tumors are often multifocal. iv. The tumors are usually preceded by an asymptomatic stage of endocrine hyperplasia involving the cell of origin of the tumor. For example, patients with MEN-1 syndrome develop varying degrees of islet cell hyperplasia, some of which progress to pancreatic tumors. v. These tumors are usually more aggressive and recur in a higher proportion of cases than do similar endocrine tumors that occur sporadically. |
|
|
|
State the location, shape, size, and weight of a normal pineal gland
|
1. It is a minute, pinecone-shaped organ (hence its name),
2. weighing 100 to 180 mg and lying between the superior colliculi at the base of the brain. |
|
|
|
Define pineoblastoma
|
1. Pineoblastomas are encountered mostly in the first two decades of life.
2. Appear as soft, friable, gray masses punctuated with areas of hemorrhage and necrosis. 3. They typically invade surrounding structures, such as the hypothalamus, midbrain, and lumen of the third ventricle. 4. Histologically, they are composed of masses of pleomorphic cells two to four times the diameter of an erythrocyte. Large hyperchromatic nuclei appear to occupy almost the entire cell, and mitoses are frequent. The cytology is that of primitive embryonal tumor ("small blue cell neoplasm") similar to medulloblastoma or retinoblastoma. 5. Pineoblastomas, like medulloblastomas, tend to spread via the cerebrospinal fluid. As might be expected, the enlarging mass may compress the aqueduct of Sylvius, giving rise to internal hydrocephalus and all its consequences. 6. Survival beyond 1 or 2 years is rare. |
|
|
|
Define pineocytoma
|
1. In contrast, pineocytomas occur mostly in adults and are much slower-growing than pineoblastomas.
2. They tend to be well-circumscribed, gray, or hemorrhagic masses that compress but do not infiltrate surrounding structures. 3. Histologically, the tumors may be pure pineocytomas or exhibit divergent glial, neuronal, and retinal differentiation. 4. Necrosis is unusual, and mitoses are virtually absent. 5. Particularly distinctive are the pineocytomatous pseudorosettes rimmed by rows of pineocytes. The centers of these rosettes are filled with eosinophilic cytoplasmic material representing tumor cell processes. |
|
|
|
State the hormonal product of Beta cells and the function of this hormone
|
1. Hormonal product: Insulin
2. Insulin function: Decrease circulating glucose through mitogenic and metabolic pathways |
|
|
|
State the hormonal product of Alpha cells and the function of this hormone
|
1. Hormonal product: Glucagon
2. Glucagon function: Increase circulating glucose by inducing glycogenolytic activity in the liver |
|
|
|
Define "diabetes mellitus
|
Diabetes Mellitus (DM) – a group of metabolic disorders sharing a common underlying feature of hyperglycemia
|
|
|
|
Give the world prevalence of diabetes mellitus
|
a. 140 million people suffer from diabetes worldwide
b. One of the most common noncommunicable diseases c. Expected to double by 2025 d. Highest numbers in India, China, & USA |
|
|
|
State the common feature of all forms of diabetes mellitus
|
a. Hyperglycemia
b. The long-term complications in kidneys, eyes, nerves, and blood vessels are the same, as are the principal causes of morbidity and death |
|
|
|
Define & give the prevalence of "Type 1 diabetes mellitus."
|
a. Type 1 DM – an absolute deficiency of insulin caused by an immunologically mediated destruction of β-cells
b. Prevalence: 10% of all cases of DM |
|
|
|
Define & give the prevalence of "Type 2 diabetes mellitus
|
a. Type 2 DM – a relative deficiency of insulin caused by a peripheral resistance to insulin with an inadequate secretion of insulin by β-cells
b. Prevalence: 80%-90% of all cases of DM |
|
|
|
Define & give the prevalence of "Maturity onset diabetes of the young (MODY)."
|
a. MODY – a classification of DM caused by a primary defect in β-cell function that occurs without β-cell loss, affecting either β-cell mass and/or insulin production
b. The outcome of a group of genetic defects characterized by: i. Autosomal dominant inheritance as a monogenic defect ii. Patients usually under 25 years of age iii. No obesity iv. Lack of islet cell autoantibodies and insulin resistance syndrome c. Prevalence: 2% - 5% of all cases of DM |
|
|
|
List 5 causes of secondary diabetes mellitus
|
1. Pancreatic disease
2. Drugs 3. Endocrine disease 4. Genetic disease 5. Infections |
|
|
|
Pancreatic disease
|
i. Examples: cystic fibrosis,
chronic pancreatitis, pancreatectomy, neoplasia, hemachromatosis, fibrocalculous pancreatopathy |
|
|
|
Drugs
|
glucocorticoids,
pentamidine, thiazides, α-interferon, thyroid hormone, protease inhitors, β-adrenergic agonists, nicotinic acid, phenytoin |
|
|
|
Endocrine disease
|
pheochromocytoma,
glucagonoma, Cushing syndrome, acromegaly, hyperthyroidism |
|
|
|
Genetic disease
|
hemochromatosis,
syndrome X, maturity onset diabetes of the young, mitochondrial DNA mutations, defects in proinsulin conversion, insulin gene or receptor mutations, and Down, Kleinfelter, or Turner syndromes |
|
|
|
Infections
|
Examples: mumps,
cytomegalovirus, coxsackie virus B |
|
|
|
Describe the twin concordance rate & HLA associations in type 1 diabetes mellitus
|
a. Twin concordance rate: 30%-70% among identical twins
b. Human Leukocyte Antigen (HLA) “MHC in humans” i. Type 1 DM has a complex pattern of genetic associations involving at least 20 loci ii. The primary loci associated with type 1 DM is the class II MHC (HLA) locus located on chromosome 6 iii. The main genes and alleles, on this locus, that are associated with DM are HLA-DR3, HLA-DR4, and HLA-DQB1*0302 iv. HLA-DQB1*0602 allele is considered “protective” against diabetes |
|
|
|
Type 1 DM - Clinical
|
1. Onset: <20 years
2. Normal weight 3. Markedly decreased blood insulin 4. Anti-islet cell antibodies 5. Ketoacidosis common |
|
|
|
Type 1 DM - genetics
|
1. 30–70% concordance in twins
2. Linkage to MHC Class II HLA genes |
|
|
|
Type 1 DM - pathogenesis
|
Autoimmune destruction of β-cells mediated by T cells and humoral mediators (TNF, IL-1, NO)
|
|
|
|
Type 1 DM - islet cells
|
1. Absolute insulin deficiency
2. Insulitis early 3. Marked atrophy and fibrosis 4. β-cell depletion |
|
|
|
Type 2 DM - Clinical
|
1. Onset: >30 years
2. Obese 3. Increased blood insulin (early);normal to moderate decreased insulin (late) 4. No anti-islet cell antibodies 5. Ketoacidosis rare; nonketotic hyperosmolar coma |
|
|
|
Type 2 DM - genetics
|
1. 50–90% concordance in twins
2. No HLA linkage 3. Linkage to candidate diabetogenic genes (PPARγ, calpain 10) |
|
|
|
Type 2 DM - Pathogenesis
|
1. Insulin resistance in skeletal muscle, adipose tissue and liver
2. β-cell dysfunction and relative insulin deficiency |
|
|
|
Type 2 DM - islet cells
|
1. No insulitis
2 Focal atrophy and amyloid deposition 3. Mild β-cell depletion |
|
|
|
State the stimulus that leads to insulin releas
|
↑blood glucose → glucose uptake by β-cells → ↑glucose metabolism → ↑ATP → ↓activity of ATP sensitive K+ channels on β-cells membrane → membrane depolarization → influx of Ca++ → secretion of insulin
|
|
|
|
State 5 functions of insulin
|
a. ↑ Glucose uptake into striated muscle cells and adipocytes
b. ↑ Lipogenesis in adipocytes and liver c. ↑ Glycogen synthesis in liver and striated muscle cells d. ↑ Protein synthesis in striated muscle cells e. ↓ Gluconeogenesis in liver f. ↓ Lipolysis in adipocytes |
|
|
|
Describe/explain the "glucose tolerance test."
|
1. Normal blood glucose: 70-120mg/dL
2. Patients can be diagnosed with DM with any of the follow test findings i. Random glucose > 200mg/dL, with classic signs and symptoms ii. Fasting glucose > 126 mg/dL on more than one occasion iii. Abnormal Oral Glucose Tolerance Test (OGTT) 3. Oral Glucose Tolerance Test i. Procedure a. Pt. fasts for 8-14 hours b. Draw a zero time (baseline) blood sample c. Pt. drinks a glucose solution (standard carbohydrate load) d. Draw a blood sample after 2hrs ii. Results a. Glucose < 140 mg/dL = Euglycemic (Normal) b. Glucose 140 – 200 mg/dL = Impaired Glucose Tolerance (IGT) c. Glucose > 200 mg/dL = Diabetes Mellitus |
|
|
|
List & explain 3 proposed interlocking mechanisms responsible for islet cell destruction in diabetes mellitus
|
1. T-cells react against β-cell antigens and cause cell damage
i. CD4+ T-cells of the TH1 subset cause tissue injury by activating macrophages ii. CD8+ T-cells directly kill β-cells and secrete cytokines that activate macrophages 2. Locally produced cytokines damage β-cells i. Immune reactions result in the T-cells producing IFN-γ and macrophages producing TNF and IL-1 ii. These cytokines have been shown to induce β-cell apoptosis 3. Autoantibodies against islet cells and insulin i. Autoantibodies react with a variety of β-cell antigens including glutamic acid decarboxylase (GAD) ii. These antibodies may participate in causing the disease or may be a result of T-cell-mediated cell injury and release of normally sequestered antigens |
|
|
|
Give the demographic group most frequently afflicted by Type 1 diabetes mellitus
|
a. Most commonly develops in childhood ( < 20 years old)
b. The risk is 2 to 5 times higher in the African-American, Hispanic, and Native American communities, compared to non-Hispanic whites |
|
|
|
Describe the microscopic pathology of islets in early onset Type 1 diabetes mellitus
|
Insulitis – early active stage lesion of type 1 diabetes in which the islets show cellular necrosis and lymphocytic infiltration (CD4+ and CD8+)
|
|
|
|
Describe the prevalence of autoantibodies in Type 1 diabetes mellitus
|
Autoantibodies against islet cells and insulin are detected in the blood of 70-80% of patients with type 1 DM
|
|
|
|
Discuss the role of immunosuppressive therapy in treatment of Type 1 diabetes mellitus
|
1. Cytokines have been shown to induce β-cell apoptosis in culture;
2. in mouse models of the disease, β-cell destruction can be reduced by treatment with antagonists against these cytokines |
|
|
|
Discuss the seasonal trends and viral implications in Type 1 diabetes mellitus
|
1. Seasonal trends that often correspond to the prevalence of common viral infections have long been noted in the diagnosis of new cases of DM
2. Viruses that are possibly involved include coxackieviruses of group B, measles, mumps, cytomegalovirus, rubella, and infectious mononucleosis |
|
|
|
Explain the postulated role of viruses in the development of Type 1 diabetes mellitus
|
Two mechanisms have been proposed:
i. Viral infections induce tissue damage and inflammation, leading to the release of β-cell antigens and the recruitment and activation of lymphocytes and other inflammatory leukocytes in the tissue ii. Viruses produce proteins that mimic self-antigens and the immune response to the viral protein cross-reacts with the self tissue |
|
|
|
Describe the twin concordance rate & HLA associations in type 2 diabetes mellitus
|
a. Twin concordance rate: 50-90% among identical twins
b. No HLA linkage |
|
|
|
List 2 metabolic defects that characterize type 2 diabetes mellitus
|
a. A decreased ability of peripheral tissues to respond to insulin “insulin resistance”
b. β-cell dysfunction that is manifested as inadequate insulin secretion |
|
|
|
Define insulin resistance & give 3 consequences
|
a. Insulin Resistance – resistance to the effects of insulin on glucose uptake, metabolism, or storage
b. 3 Consequences: i. Decrease uptake of glucose in striated muscle cells ii. Decrease uptake of glucose in adipocytes iii. Inability to suppress hepatic gluconeogenesis |
|
|
|
Describe the outcome of a renal transplant of a normal kidney to a diabetic patient and a transplant of a diabetic kidney to a normal recipient
|
a. Normal kidney to a diabetic patient results in possible lesions of diabetic nephropathy within 3 to 5 years after transplantation
b. Diabetic kidney to a normal recipient results in a reversal of the lesions of diabetic nephropathy |
|
|
|
Explain how the measurement of glycosylated hemoglobin can be used in the management of the diabetic patient
|
a. Glycosylated hemoglobin (HbA1c) represents the mean glucose value for the preceding 8-12 weeks
b. Measurement of HbA1c can be used to evaluate long-term glycemic control c. Not used to diagnose diabetes |
|
|
|
Define "early glycosylation products" and "irreversible advanced glycosylation products
|
a. Increased glucose levels results in the non-enzymatic glycosylation “glycation” of intracellular and extracellular proteins
b. End products of glycation are called Advanced Glycation End Products (AGEs) c. AGEs are more reactive than their precursor sugar and protein molecules, and cause tissue damage that results in: i. Increased vessel permeability to proteins ii. Increased atherogenesis |
|
|
|
Describe the prevalence of autoantibodies in Type 1 diabetes mellitus
|
Autoantibodies against islet cells and insulin are detected in the blood of 70-80% of patients with type 1 DM
|
|
|
|
Discuss the role of immunosuppressive therapy in treatment of Type 1 diabetes mellitus
|
1. Cytokines have been shown to induce β-cell apoptosis in culture;
2. in mouse models of the disease, β-cell destruction can be reduced by treatment with antagonists against these cytokines |
|
|
|
Discuss the seasonal trends and viral implications in Type 1 diabetes mellitus
|
1. Seasonal trends that often correspond to the prevalence of common viral infections have long been noted in the diagnosis of new cases of DM
2. Viruses that are possibly involved include coxackieviruses of group B, measles, mumps, cytomegalovirus, rubella, and infectious mononucleosis |
|
|
|
Explain the postulated role of viruses in the development of Type 1 diabetes mellitus
|
Two mechanisms have been proposed:
i. Viral infections induce tissue damage and inflammation, leading to the release of β-cell antigens and the recruitment and activation of lymphocytes and other inflammatory leukocytes in the tissue ii. Viruses produce proteins that mimic self-antigens and the immune response to the viral protein cross-reacts with the self tissue |
|
|
|
Describe the twin concordance rate & HLA associations in type 2 diabetes mellitus
|
a. Twin concordance rate: 50-90% among identical twins
b. No HLA linkage |
|
|
|
List 2 metabolic defects that characterize type 2 diabetes mellitus
|
a. A decreased ability of peripheral tissues to respond to insulin “insulin resistance”
b. β-cell dysfunction that is manifested as inadequate insulin secretion |
|
|
|
Define insulin resistance & give 3 consequences
|
a. Insulin Resistance – resistance to the effects of insulin on glucose uptake, metabolism, or storage
b. 3 Consequences: i. Decrease uptake of glucose in striated muscle cells ii. Decrease uptake of glucose in adipocytes iii. Inability to suppress hepatic gluconeogenesis |
|
|
|
Describe the outcome of a renal transplant of a normal kidney to a diabetic patient and a transplant of a diabetic kidney to a normal recipient
|
a. Normal kidney to a diabetic patient results in possible lesions of diabetic nephropathy within 3 to 5 years after transplantation
b. Diabetic kidney to a normal recipient results in a reversal of the lesions of diabetic nephropathy |
|
|
|
Explain how the measurement of glycosylated hemoglobin can be used in the management of the diabetic patient
|
a. Glycosylated hemoglobin (HbA1c) represents the mean glucose value for the preceding 8-12 weeks
b. Measurement of HbA1c can be used to evaluate long-term glycemic control c. Not used to diagnose diabetes |
|
|
|
Define "early glycosylation products" and "irreversible advanced glycosylation products
|
a. Increased glucose levels results in the non-enzymatic glycosylation “glycation” of intracellular and extracellular proteins
b. End products of glycation are called Advanced Glycation End Products (AGEs) c. AGEs are more reactive than their precursor sugar and protein molecules, and cause tissue damage that results in: i. Increased vessel permeability to proteins ii. Increased atherogenesis |
|
|
|
Explain the pathophysiology of sorbitol accumulation in cataract formation, neuropathy, and retinopathy.
|
a. Hyperglycemia leads to an increase in intracellular glucose in nerves, lenses, kidneys, and blood vessels
b. The increased glucose within these cells is metabolized by aldose reductase to produce sorbitol c. Sorbitol draws water into tissue causing damage resulting in cataracts, neuropathy, and retinopathy d. Peripheral neuropathy results from osmotic damage of Schwan cells producing demyelination e. Retinopathy results from osmotic damage to pericytes producing microaneurysms of retinal vessels |
|
|
|
Describe the pancreatic histopathology in type 1 diabetes mellitus.
|
1. chronic autoimmune attack on Beta cells.
2. Classic manifestations occur after 90% of the Beta cells are destroyed. 3. Islet destruction is caused primarily by T lymphocytes reacting against as yet poorly defined Beta cell antigens (this manifests as insulitis). 4. Autoantibodies against islet cells and insulin can be seen in 70-80% of patients. 5. It has been said that a virus can cause Type 1 DM. |
|
|
|
Describe the pancreatic histopathology in type 2 diabetes mellitus.
|
1. Lack of end organ response to insulin can lead to paradoxical hyperglycemia and hyperinsulinemia.
2. A positive feedback loop results where more insulin production leads to more insulin resistance. 3. With decreased insulin receptors on adipocytes and muscle cells, the pancreas compensates by increasing insulin output. 4. This down regulates insulin receptors and accentuates hyperglycemia. (2000 NTS) 5. Obesity and genetic predisposition both play a part |
|
|
|
List & describe 5 vascular lesions associated with diabetes mellitus
|
a. Macrovascular lesions (accelerated atherosclerosis): myocardial infarction, stroke, and lower extremity gangrene
b. Microvascular lesions: diabetic retinopathy, nephropathy, neuropathy |
|
|
|
State the main cause of death in diabetic patients.
|
Myocardial infarction caused by atherosclerosis of the coronary arteries
|
|
|
|
List & describe 3 renal lesions associated with diabetes mellitus
|
a. Glomerular lesions: capillary basement membrane thickening, diffuse mesangial sclerosis, and nodular glomerulosclerosis
b. Renal vascular lesions: atherosclerosis and arteriolosclerosis w/ hypertension c. Pyelonephritis, including necrotizing papillitis: acute or chronic inflammation that usually begins in the interstitial tissue and then spreads to affect the tubules |
|
|
|
Explain the effects of deranged insulin function of glucose, fat & protein metabolism
|
Polyuria, polydipsia, polyphagia, and with extreme derangement, ketoacidosis
|
|
|
|
Explain the pathophysiology of the association of polyuria and diabetes mellitus
|
1. Deficiency of insulin in Type 1 DM as well as lack of response from insulin in Type 2 DM causes hyperglycemia which exceeds the renal threshold for reabsorption and glycosuria.
2. The glycosuria induces an osmotic dieresis and thus polyuria |
|
|
|
Explain the pathophysiology of the association of polydypsia and diabetes mellitus.
|
The polyuria from above as well as the hyperglycemia which is pulling water from the cells into the extracellular space triggers the osmoreceptors of the thirst centers of the brain to activate.
|
|
|
|
Explain the pathophysiology of the association of weight loss and diabetes mellitus.
|
The decrease in insulin or insulin response in either DM will promote catabolism of proteins and fats to create glucose since the brain thinks there is no glucose available from the environment.
|
|
|
|
List & discuss the classic triad of signs associated with diabetes mellitus.
|
1. Polyuria (above),
2. polydipsia (above), 3. and polyphagia (explained by weight loss and body thinking that glucose is not available for energy) |
|
|
|
List 2 disorders associated with increased appetite and weight loss
|
1. Diabetes and
2. hyperthyroidism |
|
|
|
Define ketoacidosis.
|
1. Due to severe insulin deficiency coupled with absolute or relative increased glucagon.
2. The insulin deficiency stimulates lipoprotein lipase which increases levels of free fatty acids(FFA). 3. FFA is eventually converted into ketone bodies by the liver which increases acidosis. |
|
|
|
Define hyperosmolar nonketotic coma.
|
1. Typically in Type 2 DM.
2. The reason it is nonketotic is because presumably there are higher portal vein insulin levels in Type 2 DM. 3. However, we still have hyperglycemia which will still induce diuresis and coma. WIKI SAYS 1. Nonketotic coma is usually precipitated by an infection,[2] myocardial infarction, stroke or another acute illness. 2. A relative insulin deficiency leads to a serum glucose that is usually higher than 33 mmol/l (600 mg/dl), and a resulting serum osmolarity that is greater than 350 mOsm. This leads to polyuria (an osmotic diuresis), which, in turn, leads to volume depletion and hemoconcentration that causes a further increase in blood glucose level. 3. Ketosis is absent because the presence of some insulin inhibits lipolysis, unlike diabetic ketoacidosis. |
|
|
|
List at least 8 complications of longstanding diabetes mellitus, type 1 or 2.
|
1. Cataracts,
2. glaucoma, 3. retinal microaneurysms, 4. peripheral neuropathy, 5. nephropathy, 6. atherosclerosis, 7. UTI, 8. mucormycosis |
|
|
|
List and rank in order of frequency 5 causes of death in type 1 diabetes mellitus
|
MI is the most common form of death but there is no “list” in the textbook
|
|
|
|
Describe the constellation of lesions known as "diabetic nephropathy
|
Same as above on renal lesions
WIKI says 1. also known as Kimmelstiel-Wilson syndrome and intercapillary glomerulonephritis, 2. is a progressive kidney disease caused by angiopathy of capillaries in the kidney glomeruli. 3. It is characterized by nephrotic syndrome and nodular glomerulosclerosis |
|
|
|
Describe the lesions of nodular glomerulosclerosis
|
1. Glomerular lesion made distinctive by a ball-like deposits of a laminated matrix situated in the periphery of the glomerulus AKA Kimmelstiel-Wilson lesion.
2. Can look like focal segmental glomerulosclerosis but FSGS is segmental and adherent to the parietal layer of Bowman’s capsule. This adherence not seen with DM. Protein casts, thickened basement membranes of arterioles and tubules may be evident though notspecific to DM (2000 NTS) |
|
|
|
Describe the clinical course of patients with diabetic nephropathy.
|
It is a leading cause of end-stage renal disease and kidney failure which will lead to dialysis
|
|
|
|
Describe the role of glucose control in the prevention of diabetic glomerulosclerosis.
|
1. If glucose is controlled then formation of advanced glycation end products (AGEs) will not happen.
2. AGEs is the reason you get a matrix cross-linking on the GBM which can trap proteins leading to a thickened basement membrane. |
|
|
|
Describe the morbidity associated with dysfunction of the autonomic nervous system in diabetics
|
a. Cardiac arrhythmias due to autonomic neuropathy (Goljan)
b. ANS neuropathy leads to bowel dysfunction, impotence, bladder dysfunction, etc. (2000 NTS) c. Bladder dysfunction: Urine stasis --> ascending UTI --> pyelonephritis, necrotizing papillitis (2000 NTS) |
|
|
|
State 3 leading causes of blindness in the U.S.
|
a. Diabetic retinopathy is 4th most common.
b. The other top 3 are i.cataracts, ii. glaucoma, iii. age related macular degeneration (NIH website 2002 data) |
|
|
|
List 2 groups of changes seen in diabetic retinopathy
|
a. Nonproliferative and
b. proliferative |
|
|
|
Define "nonproliferative retinopathy."
|
1. Structural and functional abnormalities of angiogenesis located within the retina (confined beneath the internal limiting membrane of the retina)
|
|
|
|
Define "proliferative retinopathy."
|
Appearance of new vessels that sprout from existing vessels
|
|
|
|
List 3 features of nonproliferative retinopathy
|
1. Microaneurysms,
2. macular edema, 3. hemorrhagic exudates, and 4. micro-occlusion can also be classified under this. |
|
|
|
List the 2 main features of proliferative retinopathy
|
1. Best to look at figure 29-17 “middle picture” in the book on page 1437.
2. Neovascular blood vessels grow along the “potential space” between the posterior hyaloids and internal limiting membrane. 3. It is not called retinal neovascularization clinically or pathologically unless the newly formed vessels breach the internal limiting membrane. |
|
|
|
Describe the clinical course of proliferative retinopathy
|
1. So imagine these new blood vessels accumulating in this potential space and all of a sudden decide to rupture.
2. This would cause a posterior vitreous detachment and you could have massive hemorrhaging in that potential space. 3. If there is a wrinkle in the retina and part of the potential space decides to remain stuck, this may induce a traction retinal detachment. 4. Best to look at figure 29-17 page 1437 bottom picture. 5. This causes a potential space between the retinal pigment epithelium and the rods & cones. |
|
|
|
Traumatic Brain Injury
|
A. The major cause of traumatic brain injuries is falls (28%).
1. Some of the other causes include motor vehicle accidents (20%), ‘struck by…’ injuries, assault, suicide, and others. B. Magnitude and distribution depend on: 1. Shape of object causing the trauma 2. Force of impact 3. Whether the head is in motion at the time of impact C. Most traumatic brain injuries involve closed head injuries without fractures. |
|
|
|
Types of Skull Fractures
|
1. Linear
2. Displaced 3. Diastatic 4. Basilar Skull Fracture [ |
|
|
|
Linear
|
a. Seen in falls
b. Commonly occur when one is struck by a broad flat object; the force of impact is applied over a large surface area, which causes a linear fracture. |
|
|
|
Displaced
|
a. Creates contusions and lacerations of the brain parenchyma.
b. The distance the cranium is displaced is greater than the thickness of the bone |
|
|
|
Diastatic
|
a. This fracture occurs along suture lines, and has a sawtooth appearance.
b. Common in younger patients whose intersutural ossification is less well-developed. c. Rare to see in adults b/c their sutures are fully ossified. |
|
|
|
Basilar Skull Fracture
|
1. Orbital Roof Fractures
2. Hinge Fractures [ 3. Ring Fracture |
|
|
|
Orbital Roof Fractures
|
Produce periorbital ecchymoses, which are clinically visualized as spectacle hemorrhages (raccoon eyes).
|
|
|
|
Hinge Fractures
|
i. Extend across the base of the skull → most often in the anteriormost region of the petrous part of the temporal bone.
ii. Almost always fatal |
|
|
|
Ring Fracture
|
i. Circular or ovoid rings of fractured bone at base of skull that encircles the foramen magnum.
ii. Seen in cases where: • The vertebral column is forced superiorly (like if you fall and land on your feet) • The head is hyperextended • Impaction iii. Injuries to the chin indicate severe hyperextension. (this was mentioned 2x) |
|
|
|
External Evidence of Basilar Skull Fractures
|
1. Battle Sign
2. Spectacle Hemorrhages/Racoon Eyes 3. Hemotympanum 4. CSF Discharge from Nose or Ear |
|
|
|
Battle Sign
|
i. An olive-green to purple discoloration in the mastoid region (posterior to the ear).
ii. The battle sign indicates a basilar skull fracture through the petrous ridge with bleeding into the mastoid air cells and surrounding tissue. |
|
|
|
Spectacle Hemorrhages/Racoon Eyes
|
Bleeding around and/or within the periorbital fat that dissects into the nearby soft tissues
|
|
|
|
Hemotympanum
|
i. Due to basilar skull fracture which extends through the petrous ridge and middle ear.
ii. This may cause blood and CSF to leak from the ear. |
|
|
|
CSF Discharge from Nose or Ear
|
i. CSF Rhinorrhea: leakage of CSF out of your nose. Usually, but not exclusively, the ethmoid cribriform plate is fractured.
ii. CSF Otorrhea: leakage of CSF from ear, via a combination of ruptured tympanic membrane and nearby basilar skull fracture. iii. ‘Ring’ or ‘halo’ sign is used to determine if the discharge contains CSF. • CSF will pool peripherally while the blood will accumulate in the center. |
|
|
|
Direct Parenchymal Injury
|
1. Lacerations
2. Contusions 3. Remote (old) Contusions 4. Hyperextension injuries |
|
|
|
Lacerations
|
Due to penetration by an object with tearing of brain parenchyma
|
|
|
|
Contusions
|
1. Transmission of kinetic energy to the brain.
2. The crests of the gyri are most susceptible with sulci less vulnerable. 3. The most common sites are: i. Frontal lobe ii. Temporal lobe • These two correspond to most frequent sites of direct impact and most roughened areas of the skull, which is why they are the most commonly involved in brain contusions. 4. Less frequently may occur over the occipital lobes, brainstem, or cerebellum. i. Unless adjacent to skull fracture (fracture contusion) (the ppt says unless, but she said that they usually occur adjacent to a fracture). |
|
|
|
Types of Contusions
|
a. Types are based on location and point of impact
b. Coup c. Contracoup |
|
|
|
Coup
|
i. Contusions occur at the point of contact.
ii. Due to direct force b/t brain and skull at site of impact. iii. The skull is immobile at the time of impact. iv. This would be like getting hit in the head with a bat. |
|
|
|
Contracoup
|
i. Contusions occur opposite the site of impact.
ii. Due to brain striking opposite inner surface after sudden deceleration. iii. Head is mobile at time of impact. |
|
|
|
Morphology of Contusions
|
1. Determined via coronal section
i. They tend to be wedge shaped with a broad base at the surface centered at the point of impact. The hemorrhages at the surface are perpendicular to the brain surface. [23] 2. Early sign of contusion: i. Edema and pericapillary hemorrhage are noted. 3. < 24 hours: i. Extravasation into deep white matter parenchyma & subarachnoid space. ii. Neuronal changes • Nuclear pyknosis • Cytoplasmic eosiniphilia • Cellular disintegration • Axonal swellings (near or distant) iii. Inflammatory response 4. One major difference b/t a contusion and an infarct is that the infarct will not involve disruption of the surface of the brain parenchyma while the contusion will. |
|
|
|
Remote (old) Contusions
|
a. Characteristic macroscopic appearance
i. Depressed, retracted, yellowish brown patches ii. Involve crests of gyri most commonly located at the sites of contracoup lesions (inferior frontal, temporal and occipital poles). b. The term plaque jaune is applied to these lesions. c. They are foci for seizures if there is a really bad contusion that fails to completely heal. |
|
|
|
Hyperextension injuries
|
a. Due to sudden impact like automobile accidents.
b. May cause pontomedullary tears or transection c. Usually results in rapid death. d. Again, chin injuries are common to find in hyperextension injuries. e. The colored arrows on the picture point to hemorrhages near tears. |
|
|
|
Diffuse Axonal Injury
(Generally) |
1. Widespread structural damage to axons due to rotational and acceleration/deceleration forces.
a. The damage is due to sheer stress on the midline caused when the hemispheres rotate in opposite directions. 2. Impact is not necessary for diffuse axonal injuries (DAI). |
|
|
|
Diffuse Axonal Injury
(clinically) |
1. Cerebral concussion is thought to be a mild form of DAI without permanent pathology.
2. Patients with severe DAI become unconscious immediately after the injury. a. They may either remain comatose or go into a persistent vegetative state. |
|
|
|
Diffuse Axonal Injury
(What she said was important) |
1. Damage is most severe in midline structures b/c the two hemispheres rotate in opposite directions.
2. The most susceptible areas (deep centroaxial white matter regions): a. Corpus callosum b. Posterior limb of the internal capsules c. Cerebellar peduncles |
|
|
|
Diffuse Axonal Injury
(Microscopically) |
1. Look for axonal swellings
2. They are particularly common in the parasagittal parts of the brain: the corpus callosum, internal capsule, and the brainstem. 3. Detected with H & E and silver stains 15 hours after the injury. Note that if the patient dies earlier than 15 hours after the incident, these findings will not be seen in autopsy. 4. Beta Amyloid Precursor Protein (BAPP) is an immunostain produced by neurons as a reaction to injury that appears 2-3 hours after the injury. i. This is a good stain when you suspect DIA. |
|
|
|
Diffuse Axonal Injury
(Remote Changes) |
1. Axonal swellings may persist for years.
2. Distal to the swellings, axons and myelin degenerate and gliosis (scarring) develops over time. a. Notice in the picture that the entire brain parenchyma surrounding the lateral ventricles has undergone gliosis. 3. Decrease of white matter volume, atrophy of the corpus callosum, and dilatation of the lateral ventricles are common remote changes. |
|
|
|
Traumatic Vascular Injury
|
1. Epidural Hematoma
2. Subdural Hematoma 3. Subarachnoid Hemorrhage 4. Intracerebral Hematoma |
|
|
|
Epidural Hematoma
|
1. → blood accumulates b/t dura and skull (above the dura).
2. Seen in 2.7% to 4% of traumatic brain injuries (TBI) and has an overall mortality rate of 10%. 3. Fractures are present in 70%-90% of epidural hematomas (they are very common). 4. Develop most commonly with fractures of the squamous portions the temporal bone (mainly) and parietal bones (70%-80%); these are some of the weakest areas of the cranium. i. Commonly results from a blow to the side of the head 5. Usually the result of a tear in the MIDDLE MENINGEAL ARTERY; since this is an arterial tear, the symptoms will usually occur quickly. (NT: Don’t be confused. As you will find out in 2 or 3 lines the ‘lucid interval’ only occurs in <20% of patients, so both of these statements can be true as symptoms will result quickly in 80% of cases.) i. Less commonly, can be due to tears of the diploic veins or dural sinuses. 5. Classic Presentation: involves a lucid interval b/t the initial trauma and subsequent neurological deterioration (only seen in <20%). 6. The patient may experience loss of consciousness, severe headache, vomiting and seizures. |
|
|
|
Subdural Hematoma
|
1. → blood accumulates b/t the arachnoid and dura mater (underneath the dura)
***[46] This is another important one*** 2. Caused by rupture of the bridging (emissary) veins, which run from the arachnoid to the dura. i. Travel from surface of cerebral convexities and empty into the superior sagittal sinus. ii. Especially numerous along the superior sagittal sinus. iii. Prone to tearing along their course through the subdural space; especially in the elderly b/c the brain atrophies with age, pulling away from the cranium and stretching these veins making them easier to rupture. |
|
|
|
Facts about Subdural Hematomas
|
1. 12% to 29% of severe TBI
2. Mortality rate of 40%-60%. 3. May occur with mild or trivial head trauma. 4. Manifests within the first 48 hours after injury. 5. Most common over lateral aspects of cerebral hemispheres, usually around the temporal/parietal areas. 6. Bilateral in 10% of cases. 7. Pressure exerted on adjacent brain b/c the bleed is subdural 8. Non-localizing signs result from the fact that swelling occurs more diffusely than in an epidural hematoma. 9. Headache and confusion are common. |
|
|
|
Organization of Subdural Hematoma
|
Macroscopic (gross) findings:
i. 5-6 days: fibroblast growth causes the blood clot to be loosely attached to the dura. ii. 10-20 days: loose fibrous membrane is formed b/t the dura and the clot (outer membrane) iii. Fibrous tissue then grows around the edges of the hematoma and along its inner surface (inner membrane), encapsulating it completely. iv. Maturation of connective tissue results, after several weeks or months, in formation of a sac with tough fibrous walls (chronic subdural hematoma). The problem here is they may continue to bleed. Any stress on the scar tissue can cause the vessels to leak. |
|
|
|
Subarachnoid Hemorrhage
|
1. Most frequent traumatic brain lesion.
2. Results from rupture of corticomeningeal vessels and from hemorrhagic contusions of the brain. 3. Usually diffuse and does not exert localized pressure. 4. Hemoglobin released from RBCs in the subarachnoid space may trigger vascular spasm. 5. Fibrosis of the arachnoid membrane and the subarachnoid space may impair CSF circulation and lead to hydrocephalus. |
|
|
|
Intracerebral Hematoma
|
1. Often multiple
2. Most important risk factor is hypertension, which causes bleeds in predictable areas (more in later lectures). 3. More commonly in the frontal and temporal white matter. 4. Due to rupture of intrinsic vessels as a result of angular rotation of the brain. |
|
|
|
The effects of head trauma
|
1. Increased intracranial pressure
2. Neurological dysfunction and death can occur due to: 3. Intracranial pressure is caused by: |
|
|
|
Neurological dysfunction and death can occur due to
|
1. The brain injury itself
2. Prolonged coma with its complications. 3. Infections from open wounds or basilar skull fractures. 4. Hydrocephalus from subarachnoid hemorrhage. 5. And, most importantly, increased intracranial pressure. An increase of intracranial pressure above 40-50 mmHg will collapse brain capillaries and result in global ischemia. |
|
|
|
Intracranial pressure is caused by:
|
a. Mass effect → the added mass of epidural, subdural, and intracranial hematomas or tumors.
b. Cerebral edema, which can be due to [60] i. Vasogenic edema- the . ii. Cytotoxic edema- iii. Cerebral edema |
|
|
|
Vasogenic edema
|
1. the accumulation of water in interstitial CNS spaces due to increased vascular permeability.
2. Involves white matter more severely. 3. Extends along optic nerves (papilledema) causing blurring of vision. 4. On fundoscopic exam, the disk margins will be blurred. |
|
|
|
Cytotoxic edema
|
accumulation of water within injured cells
|
|
|
|
Cerebral edema
|
characterized by flattening of the gyri and narrowing of the sulci
|
|
|
|
Herniations
(General) |
1. The cranial cavity is partitioned by the tentorium
cerebelli and falx cerebri. 2. When a part of the brain is compressed by an extrinsic lesion or mass effect (ie. a subdural hematoma), it is displaced (ie. edema) from one cranial compartment to another. |
|
|
|
Four major herniations
|
1. Subfalcine Herniation
2. Uncal (transtentorial) herniation 3. Cerebellar tonsillar herniation [ 4. Central herniation (not mentioned, for completeness |
|
|
|
Subfalcine Herniation
|
i. Displacement of cingulated gyrus from one hemisphere to the other, under the falx cerebri.
ii. It may compress the pericallosal arteries, causing an infarct and/or hemorrhage in their distribution. |
|
|
|
Uncal (transtentorial) herniation
|
i. Herniation of the medial temporal lobe from the middle into the posterior fossa, across the tentorial opening.
ii. Compresses the ipsilateral oculomotor nerve, causing a fixed and dilated pupil, and collapses the ipsilateral posterior cerebellar artery, causing an infarct in its distribution. iii. Secondary brainstem hemorrhages due to caudal displacement of the brainstem and stretching of its vessels causing a variety of hemorrhagic lesions in the midbrain and pons. |
|
|
|
Cerebellar tonsillar herniation
|
i. Pressure on the posterior fossa contents from above or from within compresses the pons.
ii. Displacement of the cerebellar tonsils into the foramen magnum. iii. Compression of the pons and medulla damages vital centers for respiration and cardiac function, resulting in cardiorespiratory arrest. |
|
|
|
Spinal Cord Trauma
|
1. The majority of spinal cord trauma is due to motor vehicle accidents (MVAs; 50%).
2. Some other causes are acts of violence, falls, sports, and diseases. 3. The spinal cord is normally protected within the vertebral canal. [73] 4. With displacement of the vertebral column, the level of the injury determines the neurological manifestations. a. Thoracic vertebra and below: paraplegia b. Cervical vertebra: quadriplegia c. Above C-4: paralysis of diaphragm (respiratory compromise) 5. Hemorrhage, necrosis, and axonal swelling in surrounding white matter all occur at the level of the injury. 6. The lesion tapers above and below the level of the lesion. This is termed the “Cone of Necrosis.” |
|
|
|
Spinal Cord Contusion
|
1. Cord sections of long white matter tracts above and below the traumatic site.
a. Secondary ascending Wallerian degeneration b. Secondary descending Wallerian degeneration c. This just means that the axons in both directions degenerate |
|
|
|
Spinal Cord Trauma
|
Long term: cystic changes (as the lesion starts to heal) and gliosis
|
|
|
|
CNS infection
|
1. These infections have a very high mortality and morbidity
2. May present as Acute, Sub-Acute, or Chronic infections 3. Clinical findings a. Determined by the i. Anatomic site of involvement ii. Infecting pathogen iii. Host response • Infection in different parts of the brain present with different symptoms b. Inflammation and edema secondary to infection can cause symptoms • Host response to infection • Confined space does not like to be lessened 4. Effects of inflammation and edema on CNS require prompt diagnosis and appropriate therapy to minimize consequences |
|
|
|
Routes for entry of infection to enter CNS
|
1. Hematogenous spread (very common) –
a. arterial is most common; b. also have retrograde venous 2. Direct implantation (CNS trauma or iatrogenic) a. Post-traumatic b. Iatrogenic (rare post LP) 3. Local extension (impacted tooth or infected sinus) 4. Peripheral nerves • Certain viruses affect the peripheral nerves (rabies, herpes) that can spread to CNS |
|
|
|
Layers of protection for the brain
|
a. Skull
b. Meninges – three layers of tissue covering the brain and spinal cord i. Dura-outer most layer of meninges. “tough mother” ii. Arachnoid-pressed against inner surface of the dura. iii. Pia-on the surface of brain. “delicate mother” |
|
|
|
Spaces
|
a. Epidural space-surrounds the dural sac and contains epidural fat
b. Subarachnoid space-between arachnoid and pia mater and contains cerebrospinal fluid |
|
|
|
Meningitis
|
- infection involving the coverings of the CNS
|
|
|
|
Encephalitis
|
infection involving the brain parenchyma
|
|
|
|
Myelitis
|
infection involves the spinal cord
|
|
|
|
meningoencephalitis
|
infection involving the brain covering and parenchyma
|
|
|
|
meningoensephalomyelitis
|
all are infected
|
|
|
|
Classifications
|
1. Where is infection? (ex. meningitis)
2. What are the causes? (acute, chronic, sub-acute) 3. What are the organisms that cause that infection? (ex. meningococcus) |
|
|
|
Meningitis
|
1. Classification is based on characteristics of inflammatory exudates and clinical evolution of the disease
2. Infectious – bacterial a. (acute pyogenic), b. viral (aseptic), c. or chronic (TB, spirochetal, or cyptococcal) 3. Chemical – irritant introduced into subarachnoid space |
|
|
|
Bacterial Meningitis (Acute pyogenic)
|
1. Patients presents with stiff neck (meningismus), fever, headache, photophobia, and obtundation (reduced alertness).
2. Diagnosis: suspicious clinical symptoms, LP, and blood cultures. i. LP shows increased PMNs, increased proteins, increased pressure and decreased glucose. 3. Grossly, would see congested vessels with some hemorrhaging and cloudy, yellow-white pus 4. Common causes by age: i. < 3 months of age - E. Coli, Group B strep ii. 3 months to 50 yo – N. meningitides, Pneumococcus iii. > 50 yo - Listeria, Pneumococcus |
|
|
|
Viral (Aseptic) Meningitis
|
1. Aseptic is a misnomer – this is not without cause, we just cannot usually ID the cause
2. Clinical course is less fulminant than pyogenic meningitis 3. LP shows increased lymphocytes, moderate increase in protein, normal glucose. 4. Usually self-limited clinical course 5. Treatment is limited-treat symptoms |
|
|
|
Chronic Meningitis-TB, fungal, chemical agents
|
1. Patient presents with milder headache, malaise, vomiting, and confusion.
2. CSF - Pleiocytosis (moderate increase in leukocytes in CSF, predominantly mononuclear cells), increase in protein, small decrease in glucose RV Note: When used correctly, pleiocytosis actually refers to an increase in lymphocytes, but the term is often used incorrectly to refer to an increase in leukocytes. 3. Gelatinous or fibrinous exudates, usually at the base of the brain encasing cranial nerves |
|
|
|
Tuberculous Meningitis in immunocompetent
(Patterns of involvement) |
1. Diffuse Meningoencephalitis
2. Dense adhesive arachnoiditis 3. Obliterative endarteritis 4. Tuberculoma- |
|
|
|
Diffuse Meningoencephalitis
|
1. most common pattern seen;
2. increase in chronic inflammation (lymphocytes, macs, and plasma cells) 3. with granulomata (often with caseous necrosis and giant cells) |
|
|
|
Dense, fibrous adhesive arachnoiditis
|
may develop at the base of brain & causes obstruction of CNS and possible hydrocephalus
|
|
|
|
Obliterative endarteritis
|
inflammatory infiltrate in vessel wall with intimal thickening producing occlusion of the arteries and infarction of underlying brain
|
|
|
|
Tuberculoma-
|
1. usually single (may be multiple), well circumscribed, intraparenchymal mass may be associated with meningitis
2 Central core of caseous necrosis 3 surrounded by tuberculous granuloma |
|
|
|
Tuberculous Meningitis in immunocompromised (AIDS)
|
i. May show less host response & may not show typical granulomatous inflammation
ii. More prone to infection with intracellular mycobacterium – M. avium-intraceullulare 1. May show sheets of foamy looking macrophages filled with organisms and minimal granulomatous reaction |
|
|
|
Neurosyphylis (Treponema pallidum)
|
1. CNS involvement is seen in tertiary syphilis
a. Seen in 10% of patients with untreated infection 2. Patterns a. Meningovascular neurosyphylis- chronic meningitis containing “gummas.” b. Paretic neurosyphylis c. Tabes dorsalis |
|
|
|
Meningovascular neurosyphylis
|
1. chronic meningitis containing “gummas.”
2. Chronic meningitis involves base of brain and sometimes cerebral convexities and spinal leptomeninges 3. Obliterative endarteritis – perivascular plasma cell infiltrate 4. Gummas-plasma cell rich mass lesions in the meninges that may extend into the brain parenchyma |
|
|
|
Paretic neurosyphylis
|
1. parenchymal brain damage in frontal lobe which results in dementia
2. Secondary to T. pallidum invasion |
|
|
|
Tabes dorsalis
|
i. Damage by spirochetes to sensory nerves in the dorsal roots
ii. Loss of both axons and myelin in dorsal roots iii. Pallor and atrophy of dorsal columns of spinal cord iv. Produces impaired position sense and ataxia v. Nor organisms demonstrable in spinal cord vi. results in impaired position sense and ataxia. (This is classic for neurosyphilis.) vii. cannot demonstrate organisms in the spinal cord |
|
|
|
Parenchymal infections or lesions
|
1. Bacterial Abscess
2. Viral encephalitis |
|
|
|
Bacterial Abscess
|
1. Discrete parenchymal lesions with central liquefactive necrosis and surrounding fibrous capsule
a. Arise by i. Direct implantation of organisms ii. Local extension from adjacent foci (mastoiditis, sinusitis) iii. Hematogenous spread – primary site in heart, lungs, or post-tooth extraction 2. Abscess- neutrophils (acute inflammation) surrounded by fibrous capsule 3. Causes- trauma, local extension (mastoiditis, sinusitis), hematogenous spread (endocarditis, lung infection, or post tooth extraction) 4. CSF- Increased opening pressure, high WBCs and proteins, normal glucose i. Increased pressure can be more serious than the abscess-- it can lead to herniation and death. |
|
|
|
Viral encephalitis
|
1. Parenchymal brain infection usually associated with meningial inflammation (meningoencephalitis)
2. Characterized by a. perivascular and parenchymal mononuclear cells (lymphocytes, plasma cells, and macrophages), b. formation of microglial nodules (microglial cells are macrophage system of CNS), c. and neurophagia (a dying neuron surrounded by microglial cells) 3. Histologically, may see viral inclusions in nuclei i. May characterize virus by morphology or immunohistochemistry 4. Caused by Arboviruses, equine encephalitis, HSV1, HSV2, Varicella Zoster, CMV, West Nile virus, Rabies, HIV, JC polyoma virus |
|
|
|
HIV virus
|
1. Neurologic symptoms in 60% of AIDS patients
2. Patterns of direct brain injury i. Aseptic HIV-1Meningitis ii. HIV-1 meningoencephalitis i. Vacuolar Myelopathy |
|
|
|
Aseptic HIV-1Meningitis
|
1. occurs within a few weeks of initial infection
2. 10% of patients within 1 to 2 weeks of seroconversion 3. Lymphocytic meningitis |
|
|
|
HIV-1 meningoencephalitis
|
1. Sub-acute Encephalitis –
a. insidious dementia 2. and widely distributed microglial nodules containing giant cells |
|
|
|
Vacuolar Myelopathy
|
1. Spinal cord disorder
2. 20-30% AIDS patients in US 3. Pathology similar to subacute combined degeneration, however serum lelves of vitamin B12 are normal |
|
|
|
JC Polyomavirus (PML = Progressive Multifocal Leukoencephalopathy)
|
1. No clinical disease associated with primary infection (65% normal individuals are exposed by age 14)
2. Clinical disease presents along with reactivation of virus in immunocompromised. 3. Virus infects oligodendrocytes (may see viral inclusions in oligodendrocytes) 4. See extensive multifocal demylenation throughout CNS 5. Virus infected astrocytes can be confused for tumor cells 6. CT and MRI show extensive multifocal lesions in hemispheric or cerebellar white matter |
|
|
|
Rabies
|
1. Severe encephalitis transmitted by bite of rabid animal
2. Edema and vascular congestion 3. Negri Bodies diagnostic of rabies i. cytoplasmic round to oval, eosiniophilic inclusions found in the pyramidal neuron of the hippocampus and Purkinje cells of the cerebellum ii. rabies virus detected within negri bodies by immunohistochemical and ultrastructural studies |
|
|
|
Fungal disease in the CNS
|
1. Primarily in the immunocompromised
2. Patterns a. Chronic meningitis Vasculitis Direct parenchymal invasion 3. Crytococcal Meningitis 4. Candida- seen with silver stain 5. Mucor - no septa 6. Candida usually produces multiple microabscesses 7. Most fungi invade the brain by hematogenous dissemination, 8. but can also have invasion by direct extension a. (especially in diabetics with ketoacidosis = almost always mucor) |
|
|
|
Vasculitis
|
1. common with mucor and aspergillus (both have affinity for invasion of blood vessel walls) but also seen with candida
2. Cause thrombosis that produce hemorrhagic infarcts that subsequently become septic from in growth of causative fungus |
|
|
|
Direct parenchymal invasion
|
i. often coexists with meningitis;
ii. most common brain invasions caused by Candida and Cryptococcus iii. most fungi invade brain by hematogenous dissemination |
|
|
|
Other causes of CNS infections
|
1. protozoa,
2. malaria, 3. Richetsia, 4. Toxoplasmosis, 5. and entameoba |
|
|
|
Toxoplasmosis
|
a. Common in HIV patients and fetus upon maternal infection
b. Parenchymal abscess with surrounding vessels showing intimal proliferation |
|
|
|
Amoeba infections (2 significant species)
|
a. Naegleria (may see this, Dr. Lipscomb has) – rapidly fatal necrotizing encephalitis; free living in soil and fresh warm water; inhaled into the nose and goes directly to brain
b. Acanthamoeba- chronic granulomatous menigoencephalits; free living in soil, fresh water, and salt water; usually spread by hematogenous route |
|
|
|
Transmissible Spongiform; Encephalopathies (Prion Disease)…
|
1. Family of rare progressive neurodegenerative diseases that affect both humans and animals
2. Prion diseases cause spongiform changes in the brain with neuronal loss and lack of inflammation 3. A normal transmissible protein that can induce abnormal folding of other proteins 4. Creutzfeldt-jakob disease (one of the more common ones that pathologists see) a. Uniformly fatal in about 7 months b. Rare, aggressive dementia with peak incidence in 70s c. Mostly sporadic, but familial forms exist d. Spongiform, degenerative changes in the brain e. Pathologist must use different sanitation and sterilization techniques to obtain samples for research |
|
|
|
Degenerative diseases affecting the cerebral cortex
|
1. All cause dementia—progressive loss of cognitive function independent of the state of attention
2. Dementia is not part of normal aging and is always pathologic 3. Dementia is cognitive decline 4. May also involve subcortical structures |
|
|
|
Causes of dementia
|
1. Alzheimer disease
2. Frontotemporal Dementias 3. Frontotemporal Dementias w/Parkinsonism linked to chromosome 17 (FTD(P)-17) 4. Pick Disease and Diffuse Lewy Body Disease 5. Progressive Supranuclear Palsy (PSP) 6. Corticobasal degeneration (CBD) 7. Frontotemporal Dementias w/o Tau pathology 8. Vascular (multi-infarct) dementia |
|
|
|
Degenerative disease of basal ganglia and brainstem
|
1. Parkinson disease
2. Huntington disease 3. Multiple system atrophy |
|
|
|
Spinocerebellar degenerations (spinocerebellar ataxias)
|
1. Friedreich ataxia
2. Ataxia-telangiectasia |
|
|
|
Degenerative diseases affecting motor neurons
|
1. Amyotrophic lateral sclerosis
2. Bulbospinal atrophy 3. Spinal muscle atrophy |
|
|
|
CNS degenerative diseases: common ground
|
1. These inclusion are usually cytotoxic protein aggregates that cannot be processed in the cell
a. Protein aggregates may or may not relate to mutations of gene coding for these proteins 2. These inclusions are resistant to normal cellular mechanisms of degradation 3. Inclusions may be diagnostic hallmarks a. Clinically, may be able to make a diagnosis upon history and physical b. Ultimately the diagnosis is confirmed by brain biopsy and ID of these inclusions |
|
|
|
Alzheimer Disease (AD)
|
1. Most common cause of dementia in the elderly
2. Rarely symptomatic before age 50 (except in Down Syndrome patients) 3. Clinical presentation a. Insidious impairment of higher intellectual function w/alterations in mood and behavior b. Progressive disorientation c. Progressive memory loss (usually short term memory loss) d. Progressive aphasia 4. Most cases are sporadic, although 5-10% are familial mutations in the presenilin genes for γ-secretase a. Associated in beta amyloid processing 5. There’s also association to inheritance of the ε4 allele at the ApoE4 gene a. About 30% of people w/AD have inherited this allele b. Doesn’t mean that everyone who has this allele will present w/AD, though 6. Almost all Trisomy 21 patients who survive beyond 45yrs present w/pathologic changes identical to AD a. Clinical: progressive decline in cognition that ultimately leads to signs identical to AD b. Beta amyloid gene is on chromosome 21 |
|
|
|
Alzheimer disease-Gross
|
1. Cortical atrophy
a. Widening of cerebral sulci and narrowing of gyri most pronounced in the frontal, temporal, and parietal lobes (rather ominous by the time advanced clinical signs/symptoms occur) i. Slide 9 (Robbins Fig 28.34): in the picture provided you notice that the sulci are no longer almost touching and gyri are no longer abutting one another 2. Hydrocephalus ex vacuo pattern (can easily ID on CT of brain, especially towards ends of disease) a. Parenchymal loss in the brain causes compensatory ventricular enlargement |
|
|
|
Alzheimer disease-Microscopic
|
1. Neuritic (senile) plaques
2. Neurofibrillary tangles 3. Amyloid deposition, including amyloid angiopathy 4. Keep in mind: all may be present to lesser extend in the brain of elderly nondemented individuals |
|
|
|
Neuritic (senile) plaques
|
a. Neurites are dendritic and axonal processes that grow out of nerves as they grow and develop in the brain (NT note: do not confuse w/neuritis-inflammation of neurons)
b. These neuritic plaques are dystrophic neurites (malformed neurites) i. This abnormal malformation relates to the deposition to paired helical filaments, synaptic vesicles and abnormal mitochondria found within these neurites, which typically have a central amyloid core ii. Central amyloid core • Can be stained by Congo red • Primarily composed of Aβ: a peptide derived from amyloid precursor protein (APP) 1. APP is a transmembrane protein w/potential cleavage site for 3 distinct enzymes (α-, β- and γ-secretase) • There are two main types of Aβ, which differ in length by two amino acids [12] 1. Aβ40 (cerebral amyloid angiopathy) 2. Aβ42 (seen in these senile plaques) c. Slide 13 (Robbins Fig 28.35): neuritic plaque w/rim of dystrophic neurites surrounding amyloid core i. One of the microscopic findings (from biopsy) that is used to diagnose AD • Usually seen at autopsy, in association w/clinical findings d. Diffuse plaques may not have a central amyloid core e. Can be anywhere, but are usually in the hippocampus, amygdala, and neocortex |
|
|
|
Neurofibrillary tangles (NFTs)
|
1. Intracytoplasmic
2. Filament-like bundles that are flame or globose-shaped 3. Stain dramatically with silver stain (slide 17, Robbins Fig 28.35, (D) showing NFT present w/in neuronal cytoplasm ) 4. Commonly found in cortical neurons or pyramidal cells of the hippocampus, amygdala, basal forebrain, and raphe nuclei 5. Insoluble and remain long after the death of the neuron 6. Composition: i. Made mostly of paired helical filaments, which are made of hyperphosphorylated Tau protein (an axonal microtubule-binding protein that has numerous sites for potential phosphorylation) • (NT note: the tangles are NOT a mutation sequelae, they are due to abnormal phosphorylation of Tau protein) ii. There are some other components, including straight filaments, ubiquitin and MAP2 (NT note: Dr Zieske didn’t focus on these in representation of Alzheimer Disease) |
|
|
|
Basic pathologic process occurring in nonfamilial and familial AD
|
1. When APP is cleaved by α-secretase --> subsequent cleavage by γ-secretase does NOT yield Aβ
2. When APP is cleaved by β-secretase --> subsequent cleavage by γ-secretase results in production of Aβ --> which can then aggregate and form fibrils a. The aggregates can be found in the plaques or in vasculature (causing cerebral amyloid angiopathy) |
|
|
|
Cerebral amyloid angiopathy (CAA)
|
1. Causes cerebral blood vessels become brittle
a. HTN can also cause weakening of these vessels 2. Usually accompanies AD (although can be present w/o AD) 3. Vascular amyloid: Aβ40 4. Predisposes you to spontaneous cerebral bleeds 5. Congo red (+) a. Slide 21 (Robbins Fig 28.35) shows a stain of cerebral cortex, with amyloid deposition in the BVs and the amyloid core of a neuritic plaque (NT note: Congo red doesn’t discriminate b/w the two—plaque and vasculature—it stains both, so must ID whether looking at a BV or a plaque.) i. NT note: classic board question: under plane polarized light of Congo red stain, the amyloid turns apple green birefringence. (So, CAA is also called “congophilic angiopathy” for that reason.) |
|
|
|
Alzheimer Disease-Diagnosis
|
1. Diagnosed mainly by clinical findings and pathologic findings
2. Frequency estimates a. Neuritic (senile) plaque b. Neurofibrillary tangles |
|
|
|
Alzheimer Disease-Evolution
|
1. Morphologic indicators
a. Plaques b. Tangles c. Neuronal loss and gliosis 2. Pattern of progression in the brain regions mostly associated w/AD are: a. Entorhinal cortex b. Hippocampal formation c. Isocortex d. Neocortex 3. Remember, the morphologic indicators of Alzheimer’s Disease are a. Plaques b. Tangles c. Neuronal loss and gliosis |
|
|
|
CNS Degenerative Disease: Frontotemporal Dementias
|
1. Shared clinical features:
a. Progressive deterioration of language b. Changes in personality 2. Degeneration and atrophy a. Frontal lobe b. Temporal lobe 3. Different subgroups characterized by specific inclusions a. Some of these have abnormal accumulation of Tau (called “Tau-opathy”) i. The result of Tau gene mutations |
|
|
|
\Frontotemporal Dementia with Parkinsonism Linked to Chromosome 17 (FTD(P)-17)
|
1. Genetically determined
2. FTD + parkinsonian symptoms (NT note: do not confuse w/Parkinson’s Disease, simply a constellation of signs/symptoms that resemble some of those found in PD) a. Has features which are indistinguishable from idiopathic Parkinson 3. Mapped to chromosome 17 4. Tau gene mutations (“tau-opathy”) 5. Gross [26] a. Frontal atrophy b. Temporal atrophy c. Nigral degeneration 6. Microscopic a. Neuronal loss b. Gliosis, glial inclusions c. Tau-containing neurofibrillary tangles (NT note: can look for Tau with simple immunostain) |
|
|
|
Frontotemporal Dementias: Pick Disease (or, Lobar Atrophy—historic term)
|
1. Rare, distinct, progressive
2. Early onset behavioral changes 3. Alterations in personality a. Frontal lobe signs 4. Language disturbances a. Temporal lobe signs 5. “Tau-opathy” in the cases that are familial 6. Most cases are sporadic |
|
|
|
Frontotemporal Dementias: Pick Disease (or, Lobar Atrophy—historic term) - gross morphology
|
a. Atrophy of frontal and temporal lobes
i. Reduce the gyri to a thin wafer: “knife-edges” (NT note: Dr. Zieske said that they aren’t quite that sharp in biopsy…) ii. Frequently asymmetric iii. Sparing of the posterior 2/3 of the superior temporal gyrus iv. Rare parietal or occipital involvement b. Bilateral atrophy of caudate and putamen c. Slide 30: picture provided from www.alzheimer-adna.com/Images/PickBrain.jpg i. Shows a good comparison of how gyrus and sulci relate to one another abnormally and normally (NT note: you need to be able to recognize this disease from its picture for exam and boards—although rare, Dr Zieske says it always shows up on boards; will probably be given an appropriate history, a picture similar to this and maybe shown a Pick body.) |
|
|
|
Frontotemporal Dementias: Pick Disease (or, Lobar Atrophy—historic term) - microscopic morphology
|
a. Neuronal loss
i. Most severe in outer 3 layers of cortex ii. Surviving neurons may have characteristic swelling: Pick cells iii. Surviving neurons may have inclusions: Pick bodies [32] • Cytoplasmic • Round to oval • Filamentous • Weakly basophilic • Similar to neurofibrillary tangles (NFTs) seen in AD • Stain strongly w/silver methods (NT note: as did NFT’s did in AD) |
|
|
|
Frontotemporal Dementias: Pick Disease (or, Lobar Atrophy—historic term) - ultrastructure
|
a. Straight filaments
b. Vesiculated ER c. Paired helical filaments i. Immunocytochemically similar to those found in AD ii. Contain tau (NT note: need to know this. So, where have we already seen Tau? In Pick Disease, AD, and FTD—especially that associated w/chromosome 17.) d. In contrast to AD’s NFT’s, Pick bodies do NOT survive the death of their host neurons (NT note: this is rather important to the pathologist) |
|
|
|
Degenerative Diseases of Basal Ganglia and Brainstem: Parkinsonism
|
this is a set of clinical signs/symptoms that are usually due to the damage of nigrostriatal dopaminergic system, which can happen in many conditions including Parkinson Disease
1. Know the features (NT note: seen in any of the Parkinson-type disorders and classic in Parkinson Disease) a. Damage to the nigrostriatal dopaminergic system b. Diminished facial expression c. Stooped posture d. Slowness of voluntary movement e. Festinating gate (NT note: characterized as progressively shortened, accelerated steps) f. Rigidity g. Pill-rolling tremor 2. No toxic or known underlying cause 3. Pallor in the substantia nigra and locus ceruleus, due to loss of pigmented, catecholaminergic neurons |
|
|
|
Degenerative Diseases of Basal Ganglia and Brainstem: Parkinsonism
(Microscopically) |
1. can also see Lewy bodies: composed of α-synuclein filaments
2. Round, cannonball-type, eosinophilic inclusion w/clear halo surrounding it |
|
|
|
Parkinson Disease-Pathogenesis
|
1. SN dopaminergic neurons (in the striatum) degenerate
2. There is reduced striatal dopamine content 3. L-dopa: partially corrects Parkinson (NT note: patients are responsive to L-dopa for a while but it doesn’t cure them) 4. 1-methyl-4-phenyl-1,2,3-tetrahydropyridine (MPTP) (NT note: a contaminant seen in the illegal synthesis of some drugs; can cause Parkinsonism-type clinical scenarios, not Parkinson Disease) 5. Caffeine, nicotine might be somewhat protective (NT note: Dr Zieske said to not mention this to your patients that smoke, b/c they’ll use it as an excuse to continue their habit) |
|
|
|
Parkinson Disease-Pathogenesis/Outcomes
|
1. 10-15% patients develop dementia
2. Hallucinations, frontal signs 3. Dementia with Lewy Bodies (DLB) (NT note: a relatively new entity) a. Clinical features of AD and idiopathic Parkinson disease b. Lewy bodies in both substantia nigra and cortex point to DLB i. Usually due to mutations in the gene for α-synuclein ii. NT note: another example of a mutation of a protein, deposition of that protein in the form of inclusion or a body, causing toxicity to a neuron or a region of the brain, causing the neurologic signs and pathologic basis of the disease |
|
|
|
Degenerative diseases of basal ganglia and brainstem: Multiple System Atrophy
|
1. Group of disorders characterized by glial cytoplasmic inclusions (GCIs) in specific regions
a. Striatonigral degeneration b. Shy-Drager Syndrome c. Olivopontocerebellar atrophy 2. GCIs typically in cytoplasm of oligodendrocytes |
|
|
|
Multiple System Atrophy: a synucleinopathy
|
GCIs contain α-synuclein, but unlike PD, no mutations in the gene for α-synuclein
|
|
|
|
Multiple System Atrophy: a synucleinopathy - gross morphology
|
1. Cerebellum
2. Cerebellar peduncles 3. Pons (especially basis pontis) 4. Medulla (especially inferior olive) 5. Substantia nigra 6. Striatum (especially putamen) |
|
|
|
Multiple System Atrophy: a synucleinopathy -
(Microscopic morphology) |
a. Massive neuronal loss
b. Neuronal cytoplasmic inclusions of α-synuclein c. Neuronal nuclear inclusions of α-synuclein (also seen here) d. Cytoplasmic inclusions |
|
|
|
cytoplasmic inclusions
|
i. Shared diagnostic feature in this group of disorders
ii. Originally demonstrated w/silver impregnation methods iii. Can immunostaining for α-synuclein (NT note: the most prominent pathologic mechanism in this group of disorders is the mutation in α-synuclein, although there are other proteins involved in causing this group of disorders. Dr Zieske stated that he wouldn’t ask us about these others.) a. Other proteins found in these inclusions • Tau (NT note: the protein is not hyperphosphorylated in this group of disorders, in contrast w/other “Tau-opathies”) • Ubiquitin • αB-crystallin iv. 20- to 40-nm tubules v. In addition to glial cytoplasm, may also be found in a. Neuronal cytoplasm b. Neuronal, glial nuclei c. Axons d. Can actually occur in absence of neuronal loss e. Slide 46 (Image courtesy of Dr. Dennis Dickson, Mayo Clinic, Jacksonville FL, USA): synuclein positive neural and glial inclusions |
|
|
|
Multiple System Atrophy-Clinical
|
1. If the inclusions/atrophy/neuronal losses are mainly found in the…
a. Striatonigral striatum -->they’ll cause Parkinsonism i. Related to the degree of neuronal loss in SN striatum b. Nuclei of medulla, intermediolateral cell column of spinal cord --> Autonomic Dysfunction (aka, Shy-Drager Syndrome) i. Patients present w/marked orthostatic hypotension ii. Again, related to degree of neuronal loss from catecholaminergic nuclei of medulla, intermediolateral cell column of spinal cord c. Olivopontocerebellar region --> they’ll cause Ataxic/Cerebellar Disorder |
|
|
|
Huntington Disease (HD)
|
1. Autosomal dominant (NT note: so why does it perpetuate? b/c you usually don’t seen the signs until well past reproductive age)
a. ½ of offspring of an affected parent are at risk 2. Characterized by chorea, rigidity, early onset dementia a. NT note: movements starts first then progress to dementia 3. Genetics: huntingtin gene on 4p (chromosome 4; p arm) 4. Abnormal expansion in length of CAG trinucleotide repeat sequence (polyglutamine) a. NT note: again, this leads to the formation of an inclusion, which deposits in neurons and kill them 5. Disorder is usually not clinically manifest until after childbearing years |
|
|
|
Huntington Disease-Microscopic pathology
|
1. Mutant huntingtin accumulates in the nucleus of cortical neurons forming inclusion
2. Can use an antibody stain to ID them, either to huntingtin or to the polyglutamine 3. Slide 50: histology of Huntington inclusions -(NT note: accumulates in cortical neurons) 4. Slide 51 (Robbins Fig 28.38): normal hemisphere compared w/hemisphere w/HD (key feature: atrophy of the striatum and ventricular dilation) |
|
|
|
Huntington Disease-Clinical onset
|
*** these mainly occur at midlife or past reproductive age; these others are subsets of the disease)
1. Juvenile (4-19yo) 2. Early (20-34yo) 3. Midlife (35-49yo) 4. Late onset (>50yo) – most common 5. Anticipation: progressive increase in length of tandem repeat sequence as disease is passed on (so the patients fathers had a much later onset and less severe symptoms) |
|
|
|
Huntington Disease-Outcomes
|
1. Walking, swallowing become difficult
2. Psychiatric disturbances (bipolar, schizophreniform disorders) 3. Progression to severe dementia 4. Institutionalization 5. Increased risk of suicide 6. Infection: most common cause of death |
|
|
|
Spinocerebellar Ataxia – very rare
|
i. Friedreich ataxia
ii. Ataxia-telangiectasia |
|
|
|
Friedrich ataxia
|
1. Autosomal recessive
2. Gait ataxia, hand clumsiness begins in the 1st decade 3. Deep tendon reflexes markedly depressed/usually absent 4. Extensor plantar reflex (Babinski sign) 5. Impaired joint position/vibratory sense 6. Kyphoscoliosis 7. Most wheelchair bound by 5yrs of onset 8. Death by pulmonary infections/cardiac disease 9. Another example of a trinucleotide repeat: GAA trinucleotide repeat expansion results in low levels of frataxin protein (mutation makes it nonfunctional) a. Frataxin is poorly understood but is known to be needed for mitochondrial function |
|
|
|
Degenerative diseases affecting motor neurons
|
1. Amyotrophic lateral sclerosis (ALS) – motor neuron disease
2. Bulbospinal atrophy (Kennedy syndrome) 3. Spinal muscle atrophy |
|
|
|
Amyotrophic Lateral Sclerosis Aka, Lou Gehrig’s disease
|
1. Neuronal muscle atrophy (amyotrophy) due to loss of lower motor neurons in the anterior horn
a. Loss is due to demyelination 2. Marked hyperreflexia is due to loss of upper motor neurons that project in corticospinal tracts 3. male > female , slight 4. Manifests in 5th decade or later 5. 5-10% familial, autosomal dominant (NT note: remember that most of the degenerative diseases are not familial—except the one discussed w/chromosome 17—and that when they are, they’re associated w/a mutation.) a. A subset—one that been more completely documented, although there are other mutation—of familial cases is a mutation in superoxide dismutase gene SOD1 on chromosome 21 (which may cause apoptosis) 6. Thinned anterior roots of spinal cord 7. Precentral gyrus atrophic 8. Reduced anterior horn neuron density 9. Skeletal muscle atrophy (b/c of degeneration of motor neurons) 10. Slide 61 (Robbins Fig 28.39): Spinal cord showing loss of myelinated fibers (seen as a lack of stain) in corticospinal tracts. Note that the anterior roots are smaller than the posterior roots |
|
|
|
DO C 15 NOW
|
DO C 15 NOW
|
|
|
|
Arteries commonly affected by atherosclerosis and consequences
|
a. Aorta—abdominal aortic aneurysm
b. Coronary—MI, angina, sudden death c. Cerebral—infarcts d. Peripheral arteries—PVD and gangrene |
|
|
|
Normal arteries: (interior layers --> exterior layers
|
1. Endothelium,
2. intima, 3. internal elastic lamina, 4. medial smooth muscle, 5. external elastic lamina, 6. adventitia |
|
|
|
Arteriosclerosis – hardening of the arteries
|
A. 3 types:
1. Atherosclerosis 2. Monckeberg’s medial calcification 3. Arteriosclerosis |
|
|
|
Monckeberg’s medial calcification
|
1. calcification of the media
2. occurs with age beyond 50s and 60s usually in the peripheral vessels and 3. usually involve just the media and media smooth muscle and internal elastic lamina, which is part of the media |
|
|
|
Arteriosclerosis
|
1. proliferative disease which involves the smaller vessels (small arteries and arterioles);
2. usually seen in the kidneys although also seen in the heart |
|
|
|
Global distribution of atherosclerosis
|
1. more prevalent in the western world but still distributed globally
2. A life-long disease, begins in childhood, that results in atheroma (which enlarges progressively in the presence of risk factors, resulting in arterial compromise). |
|
|
|
Commonly affected arteries and their possible consequences
|
1. Aorta – abdominal aortic aneurysm
2. Coronary – MI, stable and unstable angina pectoris, and sudden death 3. Cerebral – infarcts (strokes and TIAs) 4. Peripheral arteries – PVD or gangrene |
|
|
|
Coronary artery disease (CAD)
|
1. Mortality rates in 1950: 226/100,000 people in 1950
a. Rate have fallen since 1987: almost ½ in the number of death 2. However it still remains a major cause of death among Americans 3. In 1988, 982,000 Americans died of cardiovascular disease, accounting for 45% of all deaths in the US 4. Overall deaths due to CAD mortality rates are about 500,000 and are higher in USA than in any other industrialized nations |
|
|
|
Normal human artery: - Consist of (from interior to exterior):
|
1. endothelial lining the lumen,
2. intima (consists of smooth muscle (SM) cells; although not much is present at birth), 3. internal elastic lamina, 4. medial smooth muscle, 5. external elastic lamina, 6. adventitia (consists of collagen fibers; 7. the vaso vasorum aka blood vessels are present within the collagen fibers) ***Most believe that at birth, the “new intima” starts to increase |
|
|
|
normal endothelium - its properties and functions that prevent thrombosis formation in the arteries:
|
1. Maintenance of permeability of barrier
2. Elaboration of anticoagulant 3. Elaboration of pro-thrombotic molecules (essential for coagulation) 4. Extracellular matrix (gives rise to collagen proteoglycans) 5. Modulator of blood flow (can cause constriction and vasodilatation) 6. Regulators of inflammation and immunity – a. Secretes pro-inflammatory molecules: IL-1, IL-6, IL-8 b. Secretes adhesion molecules: VCAM, ICAM, selectins 7. Regulators of cell growth – stimulates the production of certain growth factors and at the same time inhibit certain growth factors (heparin and TGF B) 8. Oxidation of LDL |
|
|
|
Smooth muscle cells,
|
1. part of arterial wall,
2. causes vasoconstriction and vasodilatation in response to normal or pharmacological stimuli 3. Responsible for synthesis of collagen, elastin, and proteoglycans 4. Elaboration of growth factors and cytokines just like the endothelium 5. They can proliferate and migrate into the intima; from contractile muscles, the synthetic smooth muscle cells form and can multiply and migrate into the endothelium in response to various stimuli |
|
|
|
Lesions:
A. Types |
1. Fatty streaks – are the first lesion that is recognized in this process; involves lipid deposit in the intima
2. Intermediate lesion – intracellular pools of lipid in arterial wall (one of the most important lesions) 3. Fibrous plaque that consists of a central necrotic core with an overlying fibrous capsule 4. Complicated plaque – lesions with hemorrhage, calcifications, ulcerations, thrombosis, and even aneurysm formation; seen in patients who have angina, MI, or sudden death |
|
|
|
lesion location
|
1. tend to occur at branch points because there is low shear; high shear areas tend to be void of lesion/plaque formation
2. This is true in the carotid bifurcation. Plaque forms in the lateral wall where there is low shear. This will eventually lead to strokes. |
|
|
|
Histologic components of plaque
|
1. Cells consist of smooth muscle cells, monocytes, macrophages, leukocytes (lymphocytes and basophils)
2. Connective tissue important for the narrowing of the vessel wall through the liberation of collagen (by smooth muscle cells), proteoglycans, and elastic fibers 3. Intra- and extracellular lipid deposits |
|
|
|
Sites of severe atherosclerosis in order of frequency:
|
1. Abdominal aorta and iliac arteries are the most common
2. Proximal coronary arteries 3. Thoracic aorta, femoral, and popliteal arteries 4. Internal carotid and basilar arteries - Notice how these include muscular as well as elastic arteries (aorta and iliac) - Atherosclerotic changes do NOT occur where the arteries divide and branch in the myocardium; but epicardial arteries are affected |
|
|
|
Type I initial lesion
|
1. Isolated macrophage foam cells
2. Growth mainly by lipid accumulation 3. from 1st decade 4. clinically silent |
|
|
|
Type II (fatty streak) lesion
|
1. Mainly intracellular and extracellular lipid deposition
2. Growth mainly by lipid accumulation 3. from 1st decade 4. clinically silent |
|
|
|
Type III (intermediate) lesion
|
1. Type II changes and small extracellular lipid pools (devoid of smooth muscle cells)
2. Growth mainly by lipid accumulation 3. from 3rd decade 4. clinically silent |
|
|
|
Type IV (atheroma) lesion
|
1. Type II changes and necrotic core (macrophages have undergone cell death, leaving pools of lipid)
2. Growth mainly by lipid accumulation 3. from 3rd decade 4. clinically silent or overt |
|
|
|
Type V (fibroatheroma) lesion
|
1. Lipid core and fibrotic layer, or multiple lipid cores and fibrotic layers, or mainly calcific, or mainly fibrotic
2. Accelerated smooth muscle and collagen increase 3. From 4th decade 4. Clincially silent or overt |
|
|
|
Type VI (complicated lesion
|
1. Rupture of the fibrous cap, hematoma-hemorrhage, thrombus
2. Thrombosis, hematoma 3. From 4th decade 4. Clincially silent or overt |
|
|
|
Framingham risk score
|
1. used to predict the risk of occurrence of first coronary event within 10 years based on risk factors
2. If less than 6, then incidence of developing coronary disease is much less; if the score is high, then a much higher chance of developing coronary disease. 3. The number of risk factors influence the risk of coronary heart disease |
|
|
|
Risk factors for atherosclerosis (Non-modifiable)
|
1. Age – increase in age --> increase in atherosclerosis
a. Death rates due to ischemic heart disease rise with each decade up to 85 years of age b. Death rates from MI decline beyond the age of 75 years 2. Male – myocardial infarction is uncommon in premenopausal women a. In the age range of 35-55, mortality is 5 times higher in males than in female i. However, rates increase in women with smoking, hypertension, and diabetes mellitus 3. Family history and genetic abnormality |
|
|
|
Risk factors for atherosclerosis (Potentially controlable)
|
1. Hyperlipidemia
2. Smoking 3. Diabetes Mellitis 4. Hypertension 5. C-reactive proteins |
|
|
|
Hyperlipidemia
|
1. high serum cholesterol or decreased HDL correlates with increased risk of atherosclerosis
2. Major plasma lipids: chylomicron, VLDL, IDL, LDL, HDL are all important in atherosclerotic changes over time 3. These are separated based on size of the lipids (chylomicrons are largest and HDL is the smallest) and the amount of cholesterol. 4. Because LDLs have the highest amount of cholesterol, it correlates very well with atherosclerotic changes. |
|
|
|
Goldstein and Brown came up with 5 types of monogenic diseases where the plasma cholesterol level increases regardless of diet due to defects in the liver LDL receptors leading to defective clearance:
|
1. The most common in the country is LDL+VLDL – 40% of this population have the frequency of atherosclerotic changes
2. Ex: Patient A with Type II homozygous hyperlipidemia – can see severe narrowing of the coronary arteries although the patient is only in his 40s |
|
|
|
Trend based on epidemiological evidence, animal studies, genetics, and therapeutic lowering of cholesterol studies
|
i. Chart showing studies done in 7different countries: the increase in serum cholesterol correlates with increased 10 year coronary death rates
ii. Framingham heart study: the higher the cholesterol the poorer the probability of survival • Researchers followed patients in Framingham, MA for 59 years and came up with the data iii. It is well known that the Japanese have lower incidence of coronary heart disease (CHD) and much lower serum cholesterol. • If they relocate to HI, then their serum cholesterol and the incidence of CHD increases since their diet changes; same thing happens when they moved to San Francisco. iv. Pathobiologic determinants of atherosclerosis in youth (PDAY) – study, in which LSU participated in, involving 15-35 year olds to map out the areas of atherosclerosis in the right coronary artery • The amount of atherosclerosis is much higher in patients with high cholesterol than low cholesterol • Same findings in the aorta (darker the area in the picture, the more the atherosclerosis) • Elevated LDL cholesterol also correlates with increased atherosclerosis • This study shows that the trend is demonstratable even at a young age v. Animal studies NT note: She went into detail regarding these studies but I just included the main point. • Rabbits with inherent hypercholesterolemia have a high tendency to develop atherosclerosis. Ordinary rabbits can be fed high cholesterol diets, leading to hypercholesterolemia, and come to the same result in a fairly short time. • Same thing can be demonstrated with mouse models. Mice that never have hypercholesterolemia never develop atherosclerotic changes. |
|
|
|
If you reduce the serum cholesterol (statins or diet control),
|
there is a decrease in CHD incidence
|
|
|
|
Smoking –
|
1. death rate from ischemic heart disease (IHD) is 70-200% higher than nonsmokers
2. Accounts for a large part of the recent increase of CHD in woman 3. The degree of coronary atherosclerosis is greater in smokers than in nonsmokers 4. Cessation of smoking in high risk men is followed by reduction in IHD 5. In the last 25 years, a 50% decline of coronary vascular disease mortality parallels the trend of reduction in smoking. 6. PDAY – in the abdominal aorta more deposition of lipids in smokers than non-smokers |
|
|
|
Diabetes Melitis
|
1. increased risk in frequency of gangrene in lower extremity and thrombosis
2. Factors that contribute to atherosclerosis: i. abnormality in lipids much higher, ii. hypertension, iii. insulin resistance, iv. glycation of protein products, v. pro-coagulant state, vi. endothelium dysfunction, vii. cell proliferation, viii. increase in the production of connective tissue |
|
|
|
Hypertension
|
do not know why it increases but they think the infiltration rate of lipoproteins in the arterial walls increases the likelihood of getting endothelial injury; this ultimately leads to lipid deposition
|
|
|
|
Guidelines today to lower the cholesterol
|
A. LDL should be less than 100 for patients at risk of heart disease; should be less than 70 for people with very high risk of heart disease – www.mayoclinic.com
B. Total cholesterol should be less than 200 C. HDL should be greater than 60 |
|
|
|
General Considerations of Neuropathology
|
1. Disorders can be either primary or secondary
2. The nervous system is a complex anatomic structure with widely distributed components 3. The nervous system has a very limited capacity to regenerate 4. The nervous system has unique structures: neurons, glial cells, myelin sheaths, etc. |
|
|
|
Primary disorders
|
1. evolve initially from the neural parenchyma or the supporting structures such as blood vessels, meninges, etc.
2. Ex: Alzheimer’s, Multiple Sclerosis, Amyotrophic Lateral Sclerosis (ALS) |
|
|
|
Secondary disorders
|
1. arise as a complication of a systemic disorder
2. Ex: hepatic encephalopathy arising from liver failure, or anoxic encephalopathy arising from transient cardiac arrest |
|
|
|
The nervous system is a complex anatomic structure with widely distributed components
|
1. Evaluation of neuropathologic disease change at autopsy requires microscopic sections taken from all of the major anatomic subdivisions of the nervous system.
2. (This is in contrast to those organs that are more uniform, such as the liver or kidneys, which require only a few histological sections for thorough examination.) |
|
|
|
The nervous system has a very limited capacity to regenerate
|
1. Axons of the CNS do not regenerate
2. There is recent evidence that neurons may be able to regenerate from stem cells that are in the hippocampus and the olfactory bulbs, but this is still under investigation 3. Axons of the PNS may regenerate 4. Selective injury |
|
|
|
Axons of the PNS may regenerate
|
there exists a potential for recovery from significant peripheral nerve damage
|
|
|
|
Selective injury
|
1. refers to the preferential occurrence of damage in certain parts of the nervous system
2. Some areas are affected more readily and/or more severely by a certain disease process (e.g., hypoxia, intoxication, metabolic disorders, neurodegenerative diseases, etc.) even though the entire nervous system was exposed to the same process 3. The basis for this selectivity is largely unknown, but it may be related to biochemical characteristics of the region, blood supply, the presence of certain types of receptors, or excess release of neurotransmitter causing excitotoxic injury. 4. If the injured neurons and axons are all functionally and anatomically related, the disorder is sometimes referred to as “systematized disease” 5. Example: Amyotrophic Lateral Sclerosis (ALS or Lou Gehrig’s disease) – a chronic, progressive, invariably fatal motor neuron disease marked by gradual degeneration of the nerve cells in the CNS that control voluntary muscle movement. (Wikipedia.com) |
|
|
|
Diagnostic Neuropathology: Staining method
|
A. Survey
B. Stains specific for individual cell components and cells |
|
|
|
Survey
|
H&E – stains nucleic acids blue. This stain is frequently used for diagnosis and evaluation. examination and diagnosis
|
|
|
|
Stains specific for individual cell components and cells
|
1. Cell body and their processes–
2. Myelin 3. Astrocytes 4. Oligodendroglia 5. Microglia |
|
|
|
Cell body and their processes
|
1. Nissl stain, Neurofilament protein (NFP), Neuron specific enolase (NSE), Synaptophysin, gold stain, and silver stain
2. Gold and silver stains are rarely used anymore. They will stain for axons or dendrites, but immunostaining is used more often today for that purpose. ***Bodian’s stain is a type of gold stain that is still used for evaluating Alzheimer’s disease patients. *** 3. Nissl staining is actually a group of stains that use basic aniline dyes to stain RNA and DNA |
|
|
|
Myelin
|
1. Intact myelin –
a. Luxol Fast Blue (LFB) stains myelin blue; b. Loyez and Weil stains myelin black. c. Absence of myelin staining indicates myelin loss. 2. Degenerating myelin in frozen section – Sudanophilic dyes. Not used so much today because samples are not long-lived. |
|
|
|
Astrocytes
|
1. Gold (Cajol Gold stain), Silver (Ortega Silver stain), Glial Fibrilary Acidic Protein (GFAP)
2. GFAP is often used for astroctyes but it is not specific for them. It will stain anything containing intermediate filaments |
|
|
|
Oligodendroglia
|
Gold, Silver, Myelin Basic Protein (MBP), Immunostaining (not addressed)
|
|
|
|
Microglia
|
Ag, LN-1, Immunostaining (not addressed)
|
|
|
|
Reactions of the nervous system to injury
|
1. Brain Edema
2. Increased Intracranial Pressure 3. Important Brain Herniations 4. Hydrocephalus |
|
|
|
Brain Edema
|
1. increase in brain volume caused by increased water and sodium in brain parenchyma (5)
2. Two types of brain edema a. Vasogenic edema b. Cytotoxic edema |
|
|
|
Vasogenic edema
|
1. most common;
2. involves damage to the cerebrovascular endothelium (aka, blood-brain barrier) 3. Occurs in association with mass lesions in the brain (tumors, hematomas, abscesses, etc.), disruptive lesions from trauma, and the later stages of cerebral infarctions associated with stroke 3. The brain surfaces (gyri) get flattened since they are being pressed against the skull. 4. The sulci are narrowed and the ventricles decrease in size. 5. The permeability of the blood brain barrier is increased. 6. In a CT or MRI images you can see contrast enhancement leaking out around lesions due to vasogenic edema |
|
|
|
Vasogenic edema (Microscopically)
|
1. you may see some pink staining homogenous fluid (edema fluid) extending out into the parenchyma (8)
2. Since vasogenic edema fluid contains serum proteins (it’s a plasma filtrate), you can use immunohistochemical stains to demonstrate its presence 3. A longitudinal section of a normal brain capillary stained this way shows localized regions with IgM that stained brown (9). Notice that the the stain is confined to the lumen of the capillary. 4. In contrast, a slide showing vasogenic edema resulting from a nearby tumor has brown-staining IgM all throughout the parenchyma because the edema fluid containing IgM has leaked through the blood-brain barrier |
|
|
|
Cytotoxic edema
|
1. less common;
2. injury to individual parenchymal cells (oligodendroglia, astrocytes, neurons, etc.) 3. Similar to vasogenic edema in that the gross appearance shows flattened gyri and narrow sulci (gross image on slide 12.) 4. Occurs during the early stages of cerebral infarction. It is also associated with water intoxication, disequilibrium syndrome, renal dialysis, and ketoacidosis 5. The cell membranes are damaged and no longer able to maintain ionic homeostasis. Water and sodium leak into the cell body. 6. There are no good histologic or immunohistochemical markers for cytotoxic edema, so it is basically a diagnosis of exclusion. i. Plasma proteins are absent from the parenchyma (it’s an ultrafiltrate.) Since cytotoxic edema is an ultrafiltrate it cannot be stained by an immunohistochemical stain like the plasma filtrate of vasogenic edema. |
|
|
|
VASOGENIC Edema
|
1. Injury = Endothelium
2. Site = White Matter 3. BBB permeability = increased 4. E.M. = ECS, Astrocytes 5. Biochemistry = Plasma filtrate (can stain) |
|
|
|
Cytotoxic edema
|
1. Injury = parenchymal cells
2. Site = gray or white matter 3. BBB permeability = no change 4. E.M. = affected cell 5. Biochemistry = ultrafiltrate (Cannot stain) |
|
|
|
Increased Intracranial Pressure
|
1. The cranial vault has a fixed volume after the cranial sutures have closed. Any added volume will increase the pressure
2. Increased volume can result from vascular congestion, edema, or space occupying lesions like abscesses, tumors and blood clots 3. As pressure increases, contents may be displaced (herniated) from one dural compartment to another |
|
|
|
Important Brain Herniations –Three Types
|
1. Uncal Herniation:
2. Cerebellar Tonsilar Herniation: 3. Cingulate Gyrus Herniation |
|
|
|
Uncal Herniation
|
1. asymmetrical, supratentorial mass lesion
2. Looking at the base of the brain you see the optic chiasm, substantia nigra, midbrain, and aqueduct. 3. There is a deep groove along the medial surface of the temporal lobe. This is the groove produced by the free edge of the tentorium. 4. The uncus and parahypocampal gyrus have herniated over the free edge, causing a displacement of the midbrain and the upper pons to the opposite side. 5. This is associated with a disturbance in the level of consciousness. 6. It can also press on the oculomotor nerve. The posterior cerebral artery is running along the groove, and it can get compressed and occluded, causing an infarct involving the calcrine cortex and some of the occipital gyri. 7. The brainstem is displaced caudally, which places stress on the vasculature and can cause brainstem hemorrhage and infarction of the calcarine area of the cortex. 8. Kernohan’s notch- If the herniation is very large, it can push the midbrain far over to the opposite side so that the opposite cerebral peduncle is pushed against the tentorium. This can result in a wedge-shaped area of necrosis in the peduncle on the opposite side of the herniation (Slides 18-20) 9. Brainstem hemorrhage (19) 10. Hemorrhage and infarction involving calcarine area (20) |
|
|
|
Cerebellar Tonsilar Herniation
|
1. posterior fossa mass lesion;
2. supratentorial midline frontal mass lesions; 3. presents with generalized increased intracranial pressure 4. Ventral surface of cerebellum involving tonsils and biventral portions of cerebellum and closely applied to upper portions of spinal cord and lower portions of midbrain. Cut surface of lower medulla is bulging indicating that there is some edema present 6. Associated with disturbances in cardio-respiratory systems and death from cardiac arrest |
|
|
|
Cingulate Gyrus Herniation
|
1. asymmetrical;
2. supratentorial mass lesion; 3. usually occurs in conjunction with uncal herniation ( 4. From the dorsal surface you can see that the cingulate gyrus is herniated across the midline. There is clockwise rotation of the corpus collosum shown in the coronal section on Slide 23 5. There are no distinctive symptoms associated with this lesion. This is generally explained by the fact that it is almost always associated with uncal herniation, and the symptoms of an uncal herniation mask those of a cingulate gyrus herniation. |
|
|
|
Hydrocephalus
|
dilatation of the ventricular system, usually as a result of obstruction somewhere within the ventricular system or the subarachnoid space
|
|
|
|
Hydrocephalus - causes
|
1. Congenital Malformation
i. Chiari Type 2 malformation – malformation of the cerebellar brainstem associated with hydrocephalus 2. Obstruction of the aqueduct, subarachnoid space, ventral system. 3. Fibrous organization due to a subarachnoid blood clot or inflammatory exudate (from previous meningitis, etc.) that lead to obstruction 4. Narrowing of cerebral aqueduct due to gliosis (26,27) 5. Blood clot from aneurysms can form clogs (24) 6. Meningeal exudates from a condition such as meningitis (28) 7. Inflammatory blockage (29) 8. In rare instances, a choroid plexus papilloma can produce excess amounts of CSF resulting in hydrocephalus (30) |
|
|
|
hydrocephalus ex vacuo
|
1. a compensatory change resulting from the loss of neural parenchyma
2. In instances of atrophy or injury resulting in parenchymal loss, the ventricles may enlarge since there is no tissue around to keep them in check. |
|
|
|
CNS Neurocellular Reactions to Injury
|
1. One or more of these changes is present in almost every pathologic state of the CNS and is indicative of parenchymal damage
2. Typically involve neurons, astrocytes, and microglia |
|
|
|
Neurons
|
1. Neurons of the cerebellar cortex demonstrate extreme variation in size and shape (36.)
2. The two large flask shaped cells are Purkinje cells |
|
|
|
Pigments normally found in neurons
|
1. Lipofuscin- Yellow-brownish granular deposits (Slide 37, H&E stain)
2. Neuromelanin- Brown pigment in the cytoplasm, greatest quantities in the neurons of the substantia nigra, locus ceruleus, and other areas that produce catecholamines i. NOT the same as skin melanin. It is a breakdown product of catecholamines and is not formed through the tyrosinase pathway. Fun fact: the substancia nigra in albinos will NOT be de-pigmented. |
|
|
|
Neuronal reaction to injury
|
1. Indicative of Cell death
2. Progressive cell injury, possibly reversible |
|
|
|
Indicative of Cell death
|
1. Eosinophilic neuronal necrosis
2. Apoptosis |
|
|
|
Eosinophilic neuronal necrosis
|
1. usually seen in association with early stage infarcts or hypoxic injuries
2. This is a common pathology seen most often in association with infarction, but can occur with other conditions 3. The normal neuron has rounded contours, fascicular nucleus and prominent nucleolus 4. The dying neuron is smaller, has a loss of nuclear detail, and the cytoplasm has a distinct eosinophilic character (“Red is dead”) |
|
|
|
Apoptosis
|
1. is programmed cell death.
2. Its role in the CNS is controversial and still under investigation. It may be the basis for some atrophic processes 3. Increased distance between cells and a loss of neural parenchyma (41) 4. In an atrophic cerebellum you can see a gross (42) and microscopic (43) volume reduction. This can be seen in the increased distance between folia and decreased cell density. |
|
|
|
Progressive cell injury, possibly reversible
|
1. Chromatolysis
2. Neurofibrillary degeneration 3. Cytoplasmic Storage 4. Inclusion bodies |
|
|
|
Chromatolysis
|
1. results from an injury near or within the neuron.
2. The cell body enlarges, contours become convex, nucleus is displaced laterally, and Nissl substance is pushed out to the periphery |
|
|
|
Neurofibrillary degeneration
|
1. also indicates cellular injury
2. Bodian silver stain of cortical neuron (45) The dark lines are dendrites; linear densities within the cytoplasm are neurofibrils, which are a composite of three types of linear protein – microtubules, neurofilaments, and microfilaments - differentiated by size (46) 3. Microtubules are 25 nanomenters in diameter; 4. neurofilaments are 10 nanometers; microfilaments are 7 nanometers. 5. This separation is not apparent at the light microscope level. 6. Neurofibrillary change is the process that results in the accumulation of neurofibrillary tangles (NFT) (47) 7. The structure of tangles can vary and in Alzheimer’s disease, they are uniformly composed of paired helical filaments (48) which are linear and make crossovers at regular intervals of 80 nanometers. 8. NFT can occur in a variety of diseases. Paired helical filaments are not specific to Alzheimer’s, but are very characteristic for the disease. Paired helical filaments are composed of structures with a diameter of 20 nanometers which are twisted around each other at 80 nanometer intervals. |
|
|
|
Cytoplasmic Storage
|
i. Congenital or Acquired enzyme deficiencies can lead to accumulation of metabolic products in the cytoplasm and damage the neuron (49)
ii. It is possible to characterize the stored material using histochemical and ultrastructural studies, thus facilitating diagnosis iii. Cortical biopsy of patient with a suspected case of Neuronal Lipid Storage Disease. (Slides 50 -52) An accumulation of PAS positive material and electron microscopy (52) which shows curvilinear bodies within the cytoplasm of the cells can help confirm the type of storage disorder. |
|
|
|
Inclusion bodies
|
1. are markers of neuronal injury can be viral or non-viral
2. Herpes simplex 3. Lewy bodies |
|
|
|
Herpes simplex
|
1. shows eosinophilic intranuclear inclusions, which are not specific to but which are always present with HSV infection (53).
2. Confirmation is obtained with an immunohistochemical stain for the herpes antigen (54). 3. HSV virions can be seen by electron microscopy (55). 4. HSV is the most common form of fatal, non-epidemic encephalitis affecting humans |
|
|
|
Lewy bodies
|
are the most common type of non-viral inclusion body and are associated with Parkinson’s disease in the substantia nigra
|
|
|
|
Astrocytes
|
1. Two types:
a. Protoplasmic Astrocytes b. Fibrous Astrocytes 2. Reactive Astrocytosis |
|
|
|
Protoplasmic Astrocytes
|
1. in the gray matter (Cajol gold stain on 58; 60)
2. Short, highly-branched processes give them a fuzzy appearance |
|
|
|
Fibrous Astrocytes
|
1. in the white matter (59)
2. Silver stain shows long, slender unbranched processes 3. Often found around blood vessels (bv can be seen running from top to bottom in the picture) |
|
|
|
Reactive Astrocytosis
|
1. refers to the sequence of changes in astrocytes that occur as a result of injury either to the cells themselves or to the surrounding parenchyma.
2. These changes can involve increase in size or number (or both) of astrocytes |
|
|
|
Primary Astrocytosis
|
refers to direct injury to the astrocytes
|
|
|
|
Secondary Astrocytosis
|
1. refers to astrocyte injury that is the result of direct injury to the surrounding parenchyma.
2. This is the most common form of astrocytosis |
|
|
|
Characteristic sequence of events in secondary Astrocytosis
|
1, Initial change involves an increase in size of the astrocyte nuclei, with visible cytoplasm around the nuclei on conventional H&E stain (62)
2. Later change involves pairs of astrocyte nuclei with the appearance of GFAP positive processes attached to the cell body (63) |
|
|
|
gemistocytic change
|
1. If the area of necrosis involves white matter or is extensive, the astrocytes continue to enlarge with the formation of more cytoplasm.
2. This is gemistocytic change and the astrocytes are now referred to as gemistocytes (64) |
|
|
|
If the necrosis is less severe or the white matter is not affected, the astrocytes involved demonstrate an enlargement of their cell bodies, but their stellate shapes are retained
|
1. As the reaction subsides there is a formation of a meshwork of slender glial processes and the area of astrocytosis takes on the appearance of a fibrillary scar with few nuclei and less prominent cell bodies (Slide 66).
2. Sometimes there are irregular beaded eosinophilic structures within the matrix of cellular processes called Rosenthal fibers (lower left corner of 67) |
|
|
|
Hepatic encephalopathy
|
1. Changes in Hepatic encephalopathy may be a form of secondary astrocytosis (Slide 68).
2. There is some increase in the size of the nucleus and formation of vesicular nuclei. 3. The chromatin is pushed to the margins of the nucleus. 4. There is no obvious increase in size of cell body or formation of astrocyte processes. 5. There may also be glycogen inclusion bodies in the cell also |
|
|
|
Microglia
|
1. A distinct population of cells widely distributed in the CNS gray and white matter (Slide 71)
2. Related to the mononuclear phagocytes and are derived from bone marrow cells (they are mesenchymal and not from neuroepithelial cells) that enter the nervous system during development – thus they are not true glial cells. 3. Microglia are normally present in their resting state and are demonstrated as small, silver-positive cells with rod-shaped nuclei and slender, branching processes. 4. They respond to parenchymal injury by a process called activation |
|
|
|
activation involves
|
1. Proliferation and cell recruitment at the site of injury
2. Formation of antigens on their surface 3. Conversion to either rod cells or phagocytes. Rods cells can be identified by their elongated cigar shaped nuclei. (74;75) 4. Secretion of cytokines 5. Release of cytotoxic substances |
|
|
|
Proliferation and cell recruitment at the site of injury
|
i. Microglial cells are seen surrounding a dying neuron. The phagocytosis of neurons is called Neuronophagia.
ii. A collection of microglia is sometimes referred to as a glial nodule (don’t get confused… this refers to microglia, not glial cells) (72) iii. As the phagocytosis continues, the microglia begin to look like macrophages (73 & 74) |
|
|
|
Characteristics of CNS tumors
|
1. Primary CNS tumors rarely metastasize outside of the CNS
a. Metastases, if they occur at all, follow surgery. 2. Malignant tumors of the CNS show rapid growth and invasiveness 3. Tumors in the CNS behave like mass lesions because they are growing in a cavity with rigid walls. Presents as a. Increased intracranial pressure and brain herniations leading to headaches and visual disturbances b. One mechanism of ICP is hydrocephalus due to a tumor blocking CSF flow in the ventricular system or compression of the subarachnoid space. 4. The rate of growth and the location of the tumor (not the type of tumor) influence the signs and symptoms associated with it. 5. 85% of CNS tumors are intracranial whereas 15% are intraspinal |
|
|
|
Primary CNS tumors
A. Annual Incidence |
1. 1.5% of new cancer cases
2. 2.2% of all cancer deaths 3. Accounts for 22% of all cancer deaths in those <15 years of age 4. Five year survival is 15-30% a. Quality of life is often poor due to radiation therapy and the tumor’s effects on the CNS. |
|
|
|
Tumor Classification
A. Classified by: |
1. Cell of origin (ex: glioma)
2. Tissue of origin (ex: meningioma) 3. Organ of origin (ex: bronchogenic metastatic carcinoma to the CNS) |
|
|
|
Four main types of CNS tumors account for 85% of all CNS tumors
|
1. Glioma (LYN: gliomas include glioblastomas, astrocytomas, oligodendrogliomas, and ependymomas)
2. Meningioma 3. Nerve Sheath 4. Metastatic |
Gee Mom, Never Mind
|
|
|
Intracranial vs. Intraspinal percentages of the tumor types differ
|
Intracranial - Intraspinal
1. Glioma 50% 2. Meningioma 15% 3. Miscellaneous 15% 4. Nerve Sheath 10% 5. Metastatic 10% Intraspinal 1. Nerve Sheath 26% 2. Metastatic 25% 3. Meningioma 23% 4.Miscellaneous 26% 5. Glioma 10% |
|
|
|
5 most common CNS Neuroepithelial (Glioma) tumors, making up 95% of the total
|
1. Glioblastoma 40% (usually occurs in >40 years of age)
2. Astrocytoma 35% (children) 3. Medulloblastoma 12% (children) 4. Ependymoma 4% (younger adults) 5. Oligodendroglioma 4% (younger adults) |
GAME Over
|
|
|
Intracranial Tumors: Adults
|
1. Supratentorial 70%
2. Infratentorial 30% 3. Most common: Glioblastoma, Anaplastic astrocytoma, meningioma, schwannoma |
gaams
|
|
|
Intracranial Tumors: Children
|
1. Supratentorial: 30%
2. Infratentorial: 70% 3. Most common: medulloblastoma, astrocytoma, cranio-pharyngioma, glioblastoma |
cam g
|
|
|
Intraspinal tumor locations:
|
A. Adults: location is a valuable clue to the histology
B. Children: spinal cord tumors are rare so there are no reliable statistics 1. Include gliomas, schwannomas, meningiomas, metastases, dermoids, teratomas, lipomas |
|
|
|
Intraspinal tumor locations: Adults
|
1. Intramedullary (within the substance of the spinal cord):
a. Almost always a glioma (ependymoma and astrocytoma are most common) b. Very rarely a metastasis 2. Intradural Extramedullary: probably a meningioma or a schwannoma 3. Extradural Extramedullary: probably a metastasis or lymphoma |
|
|
|
Slowly growing tumors of the CNS include most
|
1. meningiomas,
2. schwannomas, and 3. cerebellar astrocytomas 4. The term ‘Slowly growing’ is preferable to calling them ‘benign’ because the tumor may be growing in a area where they are not resectable or may involve vital structures and their continued presence can cause considerable morbidity and death. So, benign is not necessarily an appropriate term |
|
|
|
Malignant tumors (rapidly growing) include of CNS
|
1. glioblastoma,
2. anaplastic astrocytoma, and 3. medulloblastoma |
|
|
|
Etiology of CNS tumors: Very little is conclusively known
|
1. Experimentally, it has been shown that some viruses and chemical carcinogens can induce tumors in animals that resemble tumors that occur in humans
a. The relationship of the carcinogens to other risk factors is unknown 2. Known risk factors and their CNS tumors a. Therapeutic radiation to the head- b. Immunodeficient states- c. Certain genetic disorders- |
|
|
|
Therapeutic radiation to the head
|
1. meningiomas,
2. intracranial fibrosarcomas, 3. and some gliomas |
ME... I feel good
|
|
|
Immunodeficient states
|
primary CNS lymphomas
|
|
|
|
Certain genetic disorders-
|
1. Neurofibromatosis type I (NFI),
2. Von Hippel-Lindau disease, 3. syndromes- gliomas |
|
|
|
Meningioma
(Cytogenetic characteristics and molecular biology of CNS tumors) |
1. Loss of chromosome 22
|
|
|
|
Schwannoma
(Cytogenetic characteristics and molecular biology of CNS tumors) |
1. Loss of chromosome 22
2. Deletion of 22q |
|
|
|
Malignant glioma
(Cytogenetic characteristics and molecular biology of CNS tumors) |
1. Loss of chromosome 10
2. Deletion of 9p 3. DMS (LYN: DMS is a compound that forms composites with nucleic acid. Cytogenetic studies using this chemical suggest that it detects gene amplification) 4. Amplification of the EGFR (epithelial growth factor receptor) 5. N-myc amplification 6. Gli |
|
|
|
Medulloblastoma
(Cytogenetic characteristics and molecular biology of CNS tumors) |
1. Isochromosome 17q
2. DMS 3. C-myc |
|
|
|
1p19q codeletion
|
1. occurring in oligodendroglioma tumors signifies a favorable prognosis.
2. Eventually, these tumors will recur, but the immediate prognosis is much more favorable in most instances associated with the codeletion. |
|
|
|
Brain Metastases
|
A. Found in 20% of autopsied cancer patients
1. Of these <30% are solitary metastasis to the brain; ergo, >70% are multiple metastatic masses. 2. Cerebrum is the most common site 3. Most common primary tumors that metastasize to the brain a. Lung (59%) b. Breast (17%) c. Melanoma (3%) d. Gastrointestinal and genitourinary tract cancers B. Median survival of individuals with brain metastases undergoing radiation therapy is 18 weeks C. Death occurs due to recurrence of CNS metastasis in 30-50% of cases, due to systemic progression of the disease in 50-70% of cases |
|
|
|
Glioblastoma-gross appearance
|
a. Most commonly found in individuals <50 years old and in the cerebral hemisphere
b. Yellow areas represent zones of necrosis, while brown areas represent zones of hemorrhage. c. Extensively infiltrative (demarcated appearing areas are illusions): borders are poorly defined |
|
|
|
Glioblastoma-microscopic appearance
|
1. highly cellular with cells resembling astrocytes (LYN: usually GFAP positive)
2. Two diagnostic features distinguish it from anaplastic astrocytomas: i. [18] presence of necrosis sometimes associated with a row of radiating tumor cells called the ‘pseudopallisade’ ii. [19] presence of vascular hyperplasia 3. LYN: glioblastomas= astrocytomas + necrosis + vascular proliferation |
|
|
|
It is important to distinguish glioblastomas from anaplastic astrocytomas because, while both are malignant, the prognosis is very different. In an adult with the best available treatment
|
1. Glioblastoma has a 10-12 month median survival (shorter in individuals >50 y.o.)
2. Anaplastic astrocytoma has a 2-3 year median survival |
|
|
|
Astrocytoma
1. [20-23] Gross |
a. Usually less aggressive than glioblastomas (infiltrate and displace structures rather than destroy them)
b. Devoid of hemorrhage and necrosis, but cystic degeneration may be found within the tumor substance c. Infiltrate and displace structures rather than destroy them d. Most common site: cerebrum. Also found in the brainstem, cerebellum, and spinal cord |
|
|
|
Astrocytoma
2. Microscopically |
a. Can be well-differentiated (cellular constituents have a closer resemblance to astrocytes) which correspond to WHO Grade II tumors
b. Poorly differentiated (Anaplastic astrocytomas) correspond to WHO Grade III, which have a worse prognosis than Grade II astrocytomas and a little better prognosis than glioblastomas c. Composed of cells that resemble fibrillary and protoplasmic astrocytes d. With few exceptions, most of these astrocytomas are diffusely infiltrating i. [26] can see the cells infiltrating the cortex adjacent to the main body of the tumor ii. There is no real cure for diffusely infiltrating astrocytomas due to their infiltration into normal brain substances e. [27] higher magnification of a neuron cell surrounded by tumor cells f. [28] example of anaplastic tumor cells: variation in size and shape of nuclei, presence of mitotic figures, and increased cell density |
|
|
|
Medulloblastoma
1. [30] Gross |
a. Usually involves the cerebellum
b. Usually occurs in the midline or less commonly in the hemispheres c. Has a dual incidence peak: children 5-10 y.o. and then again between the ages of 20-30 y.o. |
|
|
|
Medullosblastoma
2. Microscopic |
1. Highly cellular tumor [31] composed of poorly differentiated cells that occasionally are arranged in a circular fashion around a central focus, forming “Homer Wright rosettes” [32].
2. Considered to indicate evidence of potential neuronal differentiation in these tumors. 3. Five year survival rate is about 80%. Unfortunately, it is accompanied by severe neurological problems. |
|
|
|
Ependymoma
|
1. [33] Gross: usually arise from cells lining the ventricles or central canal of the spinal cord
2. Microscopic a. [34] most characteristic microscopic feature is the radiating arrangement of tumor cells around blood vessels, forming ‘pseudo-rosettes’ or ‘perivascular rosettes’ b. [35] occasionally structures that resemble ependymal tubules may be seen within the tumor i. Red cells are an artifact |
|
|
|
Choroid plexus papilloma
|
a. Papillary arranged tumors that occur in the choroid plexus of the ventricles
i. Most frequent in the lateral, 4th ventricle, and 3rd ventricle ii. Most common in children <10 y.o. iii. Ependymomas and choroid plexus papillomas are considered to be slow-growing tumors, but there are not good prognostic markers for the tumors as of yet. |
|
|
|
Oligodendroglioma
|
1. Occur primarily in the cerebrum of 30-50 y.o. adults
2. *** This is the type of tumor likely to have the 1p19q codeletion that is associated with a more favorable outcome. 3. Microscopic a. [37] composed of well-differentiated cells with optically clear cytoplasm and uniform small-round nuclei (LYN: fried egg appearance) i. Blood vessels are plentiful in a ‘chicken-wire’ pattern b. [38] 70-80% are calcified which is helpful for ID via radiological imaging |
|
|
|
hematogenous metastasis
|
1. Occur characteristically in the cerebrum at the junction of the gray and white matter or in deeper portions of basal ganglia [39].
i. This location is where the blood vessels start to narrow and the tumor emboli progression is arrested. 2. The tumors than proliferate at this site. 3. [40] In the cerebellum, the metastases occur at the junction between the superior and inferior circulation for the same reason 4. Microscopic: i. sharp demarcation - [41] Most brain metastases have sharp demarcation between the tumor and the adjacent parenchyma. This characteristic was used before immunostaining to determine if undifferentiated tumors were primary or metastatic. |
|
|
|
extrinsic CNS tumors
|
A. Meningioma
B. Nerve sheath tumors |
|
|
|
Meningioma
1. Gross |
a. the tumor is in the frontal lobe attached to the dura (temporal/parietal-located lesion is a secondary compression injury)
i. Characteristically located parasagitally over the cerebral convexity, the base of the brain on the olfactory groove near the optic chiasm, the posterior fossa, or in the spinal cord b. Usually not invasive but can cause a concavity leading to a mass effect on the brain c. [43] rarely, a meningioma may arise from the ventricular system d. Usually slow growing and not aggressive |
|
|
|
Meningioma
2. Microscopic |
a. Many varieties, most of which have no particular prognostic significance. However, it is important to recognize a meningioma so as not to mistake it for another type of tumor
b. Usually arises from a meningothelial cell cluster of the arachnoid that becomes secondarily attached to the dura i. [44] leptomeningioma c. [45] Well differentiated uniform cells that may arrange themselves in concentric layers called ‘whorls’ which undergo degeneration with the formation of calcium deposits (forming Psammoma bodies – not necessarily present in all meningiomas) 3. LYN: from Robbins ‘Meningiomas are predominantly benign tumors of adults…[and] are rounded masses with a well defined dural base that compress underlying brain but are easily separated from it.’ |
|
|
|
Nerve sheath tumors
|
Two types: schwannomas and neurofibromas
|
|
|
|
Schwannomas
|
a. Most common type of nerve sheath tumor within the CNS, arising most frequently from the vestibular branch of CN VIII [47] lying in the cerebello-pontine angle and causing compression of brainstem and adjacent nerve roots.
b. Does not have the same association with NFI and II that neurofibromas have unless both CN VIIIs are affected. In that instance, it is associated with NF II c. Produce an eccentric enlargement d. Encapsulated e. [48] microscopic i. Two types of tumor tissue: Compact and loose mesh, both of which are composed of Schwann cells ii. The compact areas are referred to as Antoni A iii. Loose mesh areas are Antoni B |
|
|
|
Neurofibromas
|
a. Arise within peripheral nerves but may extend into the CNS through infiltration of nerve roots.
b. Microscopic [49]: show a cylindrical enlargement of affected nerve i. [50] Tumor cells in the periphery, surviving axons and myelin sheath central ii. [51] accumulation of large numbers of spindle shaped tumor Schwann cells in an area of a neurofibroma c. Not encapsulated d. Composed of a diffuse proliferation of fibroblasts and Schwann cells (form myelin around peripheral nerve axons) e. May be associated with Neurofibromatosis I and NF II |
|
|
|
Tumors involving the 3rd ventricular area
|
A. Cranial pharyngioma
B. Pituitary adenoma (arising from cells of the anterior pituitary gland) |
|
|
|
Cranial pharyngioma
|
1. Most common in children and young adults <20 y.o.
2. Slow-growing, but difficult to resect due to their location 3. Gross: a. Arises from cells in the region of the stalk of the pituitary b. [52] The tumor has pushed through the floor and embedded itself in the 3rd ventricle 4. Microscopic: a. [53] epithelial cell trabeculae surrounding areas of cystic degeneration and containing foci of calcifications are characteristic of these tumors |
|
|
|
Pituitary adenoma (arising from cells of the anterior pituitary gland)
|
1. Symptoms of these tumors can be related to the type of hormones secreted as well as optic nerve compression causing field defects.
2. Treatment is generally successful 3. Classification is based on the hormone secreted by the tumor a. “Null cell” or undifferentiated adenoma which secrete nothing (most common) b. Prolactin-secreting c. GH secreting d. ACTH secreting 4. [54] Gross a. This tumor was detected at autopsy, but today they are detected much earlier 5. Microscopic a. [55] diffuse proliferation of cells or b. [56] formation of papillary structures around blood vessels in a sinusoidal pattern. |
|
|
|
Cerebrovascular diseases
|
A. A group of disorders that develop as a result of:
1. Lesions in the blood vessels that supply the brain 2. Systemic circulatory disorders 3. Bleeding disorders |
|
|
|
Two important characteristic lesions
|
1. Ischemic parenchymal necrosis
2. Hemorrhage |
|
|
|
Ischemic parenchymal necrosis
|
a. Evolves when the blood supply to a region is insufficient to meet its metabolic needs over a sustained period of times (about 5-10 minutes in the CNS)
b. May be due to vascular occlusion or significant decrease in perfusion pressure as a result of systemic problems such as transient cardiac arrest, severe hypotension, or cardiac arrhythmias |
|
|
|
Hemorrhage
|
a. Consequence of either congenital or acquired lesions in the blood vessels that supply the brain or bleeding disorders
|
|
|
|
Two types of ischemic necrosis in the CNS
|
A. Global: associated with perfusion problems (multiple parts of brain are affected)
B. Focal: associated with obstructive vascular disease (single or focal area of brain is affected) |
|
|
|
Global ischemic necrosis (GROSSLY)
|
1. In global ischemic encephalopathy, the lesions are located/accentuated in the distal perfusion beds of the major cerebral arteries.
2. Hemorrhagic areas affecting cortex [4] 3. Additional lesions in the terminal perfusion bed affecting corpus striatum [4] 4. Lesions in the distal perfusion beds in the cerebellum [5] 5. Sommer’s sector: a strip of hippocampal cortex immediately adjacent to the lumen of the temporal horn of the lateral ventricle [6] |
|
|
|
Global Ischemic Necrosis
(Microscopically) |
1. Changes vary according to the severity and extent of the ischemia.
2. Neurons are the most vulnerable cells (to ischemia), and they will undergo eosinophilic necrosis after complete ischemia lasting 5- 10 minutes in a normothermic adult [7] 3. The neurons in the 3rd and 5th cortical layers are affected first and most severely, producing a lesion that is referred to as laminar necrosis [8] i. Laminar necrosis appears as decreased cell density (pallor of staining and reduced number of cells) in the 3rd and 5th layers of the cerebral cortex. 4. In very severe ischemia, all of the neurons in the cortex are affected. In these cases, laminar necrosis is not seen [9] |
|
|
|
Focal Ischemic Necrosis
|
1. An infarct is an area of focal ischemic necrosis that usually develops in association with atherosclerosis in major vessels accompanied by either thrombotic or embolic occlusion.
a. Thrombus in the basilar artery that developed on an atherosclerotic plaque [10] 2. The changes associated with infarction follow a temporal sequence. a. Grossly: Initially the affected part of the brain is swollen and soft [11] 3. Embolic infarcts are often hemorrhagic [12]. |
|
|
|
Embolic infarcts are often hemorrhagic [12]. Here’s why:
|
a. Initially, the embolus occludes a vessel causing the infarction as well as damage to the occluded vessel.
b. The embolus then fragments, opening the damaged vessel up to blood flow. The fragments travel downstream. c. Blood flowing through the affected vessel leaks out into the parenchyma forming petechial hemorrhages. |
|
|
|
Focal Ischemic Necrosis (Microscopically)
|
1. Eosinophilic neuronal necrosis can be detected with conventional staining as soon as six hours after the onset of the infarct. [13] (NT note: Figure 28-13 in Robbins says it best)
2. Perivascular accumulation of red blood cells are present in the regions of hemorrhagic infarction. [14] 3. During the first 2-3 days, neutrophils begin to infiltrate the infracted area, peaking around 48-72 hours (hm… looks like the same timeframe to me), before they disappear. 4. By the end of the first week, an astrocytic reaction is evident, seen as large bodied astrocytes and lipid phagocytes removing necrotic debris. i. LYN: Astrocytosis – the reaction of astrocytes to paranchymal injury. It is similar to the healing process of paranchymal injury in other tissues – the damaged tissue is cleaned up by macrophages and there is subsequent proliferation of fibroblasts to create scar tissue except in astrocytosis, there are astrocytes in place of fibroblasts. It is important to note that there is an absence of mitotic figures. 5. After 2-3 weeks, the cut surface of the infarct will have a number of small cavities [18] 6. After 3-4 months, there are no further changes in the lesion. i. LYN: Microscopically at 4 months there is a loss of paranchymal tissue resulting in the formation of cavitary leisions traversed by gliovascular trabeculae – thin walled blood vessels ensheathed by glial processes. 7. Sections of the parenchyma of older infarcts often contain cavities that are partially filled with phagocytes and gliovascular trabeculae – blood vessels that course across the lumen of the cavity that are ensheathed by astrocytes [20]. The cavities are surrounded by an astrocytic reaction. [21] |
|
|
|
two distinctive types of cerebral infarction to know
|
1. Lacunar Infarcts &
2. Venous Infarcts |
|
|
|
Lacunar infarcts
|
1. Associated with “small vessel disease” caused by systemic hypertension or diabetes mellitus.
a. LYN: Lipohyalinosis – descriptive term that refers to the fact that the media of the vessel is replaced by hyalinized tissue which results in an increase in basement membrane material as well as eccentric thickening of the intima and presence of foamy macrophages within the intima. Lipohyalinosis occurs in HTN and is associated with lacunar infarcts. 2. Circumscribed cavitary lesions less than 1.5 cm in diameter. 3. Found most often in the basal ganglia, thalamus, and corpus striatum 4. Group of infarcts involving the putamen and the thalamus [23] 5. Also found in the striate portion of the pons [24] and subcortical white matter [25] 6. Occur as a result of obstructive lesions affecting the parenchymal arteries, meaning those arteries that lie within the substance of the brain. a. Example showing an artery with intimal thickening resulting in reduction of the lumen diameter. [26] |
|
|
|
Venous infarcts
|
1. Hemorrhagic
2. Develop as a result of occlusion of a dural venous sinus or occlusion of a major cerebral vein. 3. Aseptic venous thrombosis is associated with coagulation disorders, dehydration, and CHF 4. Septic thrombophlebitis which may be associated with infections of the face, bony sinuses, dura, or meninges. 5. Example showing cross sections of the superior saggital sinus: the lumen is occluded by an acute thrombus that induced areas of bilateral hemorrhagic infarction that lie within the territory drained by the superior saggital sinus. [27] a. These infarcts are hemorrhagic because the obstruction occurred on the venous side of the circulation; arterial blood continued to be pumped in to the area (capillaries), but it could not get out. [28] b. Initially the vessels became congested resulting in stasis and damage to the endothelium and then eventually blood leaks out into the surrounding parenchyma. |
|
|
|
Nontraumatic intracranial hemorrhages
|
Hemorrhagic lesions associated with cerebrovascular disease.
|
|
|
|
Common causes of nontraumatic intracranial hemorrhage
|
1. Systemic hypertension
2. Ruptured saccular aneurysm 3. Ruptured vascular malformation 4. Bleeding disorders |
|
|
|
the most common cause of massive fatal intracerebral hemorrhage
|
hypertension
|
|
|
|
massive fatal intracerebral hemorrhage - Occur most often (in descending order of frequency) in the
|
a. Basal ganglia[30]
b. Brain stem with extension into the 4th ventricle [31] c. Cerebellum with extension into the 4th ventricle [32] (can be mid line or lateral) |
|
|
|
Hemorrhagic lesions associated with cerebrovascular disease
|
A. cause a number of problems. In addition to disrupting the tissue,
b. they also behave as mass lesions, causing increased intracranial pressure and herniation of different parts of the brain. c. These hemorrhages often extend into the ventricular system. Blood then finds its way out of the ventricles and into the subarachnoid space. D. Smaller, nonlethal hemorrhages can occur in hypertension at various sites, most often in the subcortical white matter. 1. Example showing small hemorrhage in the subthalamic nucleus |
|
|
|
vascular basis for these massive hemorrhages is still being debated, but the two leading candidates are:
|
1. Fibrinoid necrosis of the blood vessel wall.
2. Rupture of small microaneu`rysms called Miliary Aneurysms of Charcot [34] |
|
|
|
Fibrinoid necrosis of the blood vessel wall
|
The wall of the blood vessel undergoes necrosis with deposition of fibrin in the media
|
|
|
|
Rupture of small microaneu`rysms called Miliary Aneurysms of Charcot
|
a. Aside: Charcot was a late 19th century French neurologist who first described these lesions.
b. Example of thrombosed miliary aneurysm of Charcot |
|
|
|
the most common cause of nontraumatic subarachnoid hemorrhage
|
1. Ruptured saccular aneurysm
|
|
|
|
Important characteristics of saccular aneurysms
|
1. 90% occur on the anterior half of the Circle of Willis, involving either the anterior communicating artery, at the bifurcation of the middle cerebral artery, or the junction of the posterior communicating and internal carotid arteries
2. They vary in size, but those that rupture are generally about 0.8 cm in diameter or larger. 3. Women are affected more than men 4. Symptoms develop between 35 – 65 years of age, though congenital saccular/berry aneurysms are often found incidentally at autopsy and may be symptomatic sometime after puberty (Sx are rare before puberty) 5. Pathogenesis is uncertain, though genetic factors may be involved (problems with matrix proteins, etc) 6. Bad disease: up to 70% of affected patients either die or develop profound neurologic deficit. Survivors may experience profound psychological problems related to the effects of the hemorrhage in the absence of physical disability. 7. Are often multiple and frequently bilateral (20 – 25% of cases). i. This is important in patients with suspected rupture: you must be certain that you find the one that is bleeding, so order bilateral studies. ii. Example of middle cerebral artery with multiple aneurysms, one that actually ruptured. [40] 8. Blood may also enter the brain (about 20% of cases), forming a mass lesion that can produce focal symptoms as well as herniations. |
|
|
|
less frequent cause of subarachnoid hemorrhage
|
Ruptured vascular malformations
|
|
|
|
Ruptured vascular malformations
|
1. Most commonly an arterio-venous malformation (AVM) composed of abnormal vessels. Some will resemble arteries, some will resemble veins.
a. LYN: Tangle of blood vessels that form a relatively direct connection between high pressure arteries and low pressure veins. This results in a collection of blood vessels with abnormal connections and no capillaries – extremely fragile and prone to bleeding. 2. Can occur at any site in the brain and are most common in the cerebrum and cerebellum 3. Gross examples: a. Very large unruptured AVM identified incidentally at autopsy [42] b. AVM involving the cerebellum. Can see the abnormal vascular channels on the cross section [43] 4. Microscopically: a. Composed of abnormal arteries and veins, demonstrable using special stains [44] b. Connective tissue and elastic stain showing a vessels with features of a vein (top right) and an artery (bottom left; note the internal elastic membrane), with astrocytosis in between. [45] (glial process of astrocytes are stsained using a Holzer stain) 5. There are types of vascular malformation besides AVMs but they are less frequently involved in hemorrhage. “At this stage, it’s the AVM that you want to remember.” |
|
|
|
Stroke
|
1. The lesions discussed in the context of this lecture form the pathologic basis for the clinical disorder referred to as a “stroke”
2. Frequently, the lesions themselves are referred to as strokes – this is wrong! “Stroke” is a clinical term, not a pathologic term 3. The following was provided as a workable definition of stroke: nonconvulsive neurologic deficit of rapid onset that reaches a maximum severity in hours and days. 4. Stroke is the most common form of cerebrovascular disease. 5. Brain infarcts and nontraumatic intracranial hemorrhages are the most common pathologic lesions associated with stroke. 6. 80% of strokes are associated with infarction (some form of occlusive vascular disease) 7. 10% of strokes are associated with hemorrhage as a result of hypertension 8. 10% of strokes are associated with a primary subarachnoid hemorrhage, most often rupture of a saccular aneurysm |
|
|
|
Demyelinative Diseases Characteristics
|
A. Demyelinative diseases are a group of nervous system disorders in which the myelin is injured/lost selectively as a result of either:
1. Injury to myelin sheath or to the cells that make myelin, or 2. Disturbances in the synthesis or degradation of myelin. B. They can involve the central nervous system, the peripheral nervous system, or both. C. Axons are relatively spared. 1. In rare instances, there is necrosis of all of the parenchymal elements within the lesion. |
|
|
|
Secondary Demyelination
|
A. Loss of myelin that occurs because of axonal injury or as a component of a destructive process that involves all of the tissue elements in a region is sometimes referred to as secondary demyelination
1. Ex. infarcts in the white matter 2. Diseases of this type of demyelination are not referred to as Demyelinative Disorders. |
|
|
|
IV. Principal Human Demyelinative Disorders [7]
1. These are grouped according to the pathogenesis of the myelin injury. |
A. Injury to myelin sheath:
B. Disturbed synthesis or degradation of myelin C. Injury to cells making myelin (oligodendroglia) |
|
|
|
Injury to myelin sheath:
|
1. Multiple sclerosis (MS): affects only CNS
2. Acute disseminated encephalomyelitis (ADE): affects only CNS 3. Acute hemorrhagic leukoencephalitis: affects only CNS 4. Central pontine myelinolysis (CPM): affects only CNS 5. Acute idiopathic polyneuritis (Guillain-Barre Syndrome) : affects only PNS |
|
|
|
Disturbed synthesis or degradation of myelin
|
1. Leukodystrophies
a. Some of these involved both CNS and PNS, and some only involve the CNS myelin |
|
|
|
Injury to cells making myelin (oligodendroglia)
|
1. Progressive multifocal leukoencephalopathy (PML)
a. Demyelination is confined to the CNS. |
|
|
|
Relapsing-Remitting Multiple Sclerosis (Chronic Relapsing Multiple Sclerosis)
CHARACTERISTICS |
1. The most common and important form of demyelinative disease. (80% of MS cases)
2. The etiology is unknown. a. It is suspected that immunologic, genetic, and infectious mechanisms may all be involved. 3. The onset is usually between 20 and 40 years of age. 4. Women are affected more than men (2:1) 5. The clinical course initially is characterized by remissions and exacerbations of neurological disturbances. Many times there is apparent full recovery, but some time later the symptoms flare up, often affecting another part of the nervous system. a. In the later stages, the disease becomes progressive and there is much less remissions. |
|
|
|
Gross Organs with MS Lesions:
|
1. [9] The lesions of MS can be found in all parts of the nervous systems but typically occur around blood vessels.
a. This one is located near the lateral angle of the lateral ventricle. b. The gross lesions are referred to as plaques. 2. [10] This one is immediately adjacent to the occipital horn a. The lesion is gray, sharply defined, and has a translucent quality. The cut surface of the lesion is sunken. 3. [11] These plaques can occur at any point that myelin is present including the gray matter. a. This one is within the thalamus. (NT Note: It is the gray circle within the thalamus on the left side of the slide… And just in case you’ve pushed neuro out of your brain like me, the thalami are the big blobs of grey matter on the sides of the “Y” shape in the center of the slide) i. Only the myelin sheaths within this lesion are affected. The neurons, axons, and other structures remain intact. b. At the bottom left, next to the temporal horn there is a plaque (gray crescent shape) and there is another smaller one on the opposite side. 4. These lesions are also characteristically present in: a. [12] the brainstem b. [13] the cerebellum c. [14] the spinal cord |
|
|
|
Microscopic Sections with MS Lesions
|
1. [15] This section is a portion of the cerebral spinal cord stained with LFB (for myelin).
a. This area of myelin pallor represents a large well-defined plaque in the spinal cord. i. Emphasizes the fact that peripheral myelin in MS is spared. It shows the anterior nerve roots in which the myelin is intact, but immediately adjacent to that, there is a large MS plaque with a loss of myelin. 2. [16] The optic nerves are also a characteristic location for MS plaques. 3. The next three slides are serial sections through a chronic plaque that show the histologic features. a. [17] H&E stain that shows astrocytosis. b. [18] Myelin stain show that there are NO myelin sheaths located within this lesion. c. [19] Silver stain for axons. The axons are reduced in number but are relatively preserved. |
|
|
|
Leukodystrophies [20]
A. General Characteristics |
1. Demyelination occurs because of a disturbance in the synthesis or degradation of myelin.
2. Most leukodystrophies affect children. 3. Several leukodystrophies are genetically determined (either autosomal recessive or X-linked). 4. Common neuropathologic features include: a. Diffuse loss of myelin in the cerebral hemispheres, brainstem, cerebellum, and spinal cord. b. Relative sparing of the axons. c. Diffuse fibrillary astrocytosis in the white matter. 5. The arcuate fibers, the fibers that run immediately beneath the cortex, are often spared. 6. There may be an abnormal accumulation of lipids in the central and peripheral nervous system if there is a peripheral neuropathy. 7. Some forms of leukodystrophies have both CNS and PNS involvement. (And some only affect the CNS) |
|
|
|
(Infantile) Metachromatic Leukodystrophy (MLD) [21]
1. Characteristics: |
a. MLD is the most common type of leukodystrophy.
b. Autosomal recessive c. Caused by an absence of arylsulfatase A, an enzyme that is necessary for breakdown of myelin lipids. i. This results in the accumulation of cerebroside sulfate in the white matter and elsewhere in the body. |
|
|
|
Gross Organs with MLD lesion
|
This is a brain from a child with MLD
i. Notice the thinning of the corpus callosum, secondary to the myelin and some axon loss. ii. The cortical matter is somewhat discolored. iii. The cortical ribbon, which is gray matter, for the most part appears intact. iv. The cut surface is slightly sunken because of the decreased in the amount of parenchyma. v. The ventricles are enlarged. This is an example of hydrocephalus ex-vacuo, which is compensatory enlargement of the ventricles secondary to the loss of tissue, not because of obstruction. |
|
|
|
Microscopic Sections with MLD lesions
|
1. The next few sections are through the subcortical white matter immediately adjacent to the ventricle.
2. [23] Low power of the cortex and subcortical white matter using LFB stain for myelin. i. There is extensive loss of myelin staining throughout the subcortical white matter with some preservation of the arcuate fibers. 3. [24] Higher magnification of the same area with LFB stain. i. Confirms that it is devoid of myelinated axons. 4. [25] Silver Stain of the lesion. i. Can identify some preserved axons 5. [26] Some of the leukodystrophies are associated with the accumulation of lipids in the white matter and elsewhere. |
|
|
|
Some of the leukodystrophies are associated with the accumulation of lipids in the white matter and elsewhere
|
i. MLD is an example of this type of disease in which cerebroside sulfate accumulates in the white matter and to a lesser extent in other tissues as well.
ii. These accumulations can be demonstrated with a metachromatic stain. This kind of stain looks to be one color, but if it encounters a particular type of tissue, it changes color and a different color will be apparent on the slide. iii. This slide uses acidified cresyl violet. • Normal tissue has a bluish-red-purple appearance. • The metachromatic deposits are the brown deposits in the white matter either within macrophages or extracellularly. • Demonstration of these metachromatic deposits using acidified cresyl violet is pathognomonic of infantile MLD. |
|
|
|
Before the identification of aryl sulfatase A, the diagnosis of MLD was usually confirmed on the basis of a sural nerve biopsy
|
1. sural nerve = a nerve of the lower leg)
2. The sural nerve would be stained with acidified cresyl violet to look for the metachromatic deposits on the Schwann cells and elsewhere. 3. Now, with the identification of aryl sulfatase A, the presence or absence of the enzyme is tested for in a urine test. (so a sural nerve biopsy is no longer necessary to confirm the diagnosis) |
|
|
|
Progressive Multifocal Leukoencephalopathy (PML) [27]
A. General |
1. This is an example of demyelination that develops as a result of damage to the oligodendroglia, the cells that manufacture myelin in the CNS.
2. The etiology involves the Papovaviruses, a family of DNA viruses whose name is derived from the initials of the principle subvarieties: a. Papilloma viruses b. Polyoma viruses c. Simian Vacuolating virus (SV 40) 3. The JC virus, the Simian Vacuolating virus, and the BK virus have all been isolated from human cases (of PML). a. Most often the JC polyoma virus is isolated in PML |
|
|
|
PML - Pathogenesis
|
1. The pathogenesis is thought to involve reactivation of a latent infection, mainly with the JC virus.
a. There is a prevalence of JC antibodies in 75% of adults and the reactivation occurs in association with T cell deficiencies such as lymphoproliferative disorders, immunosuppressive therapy, primary immunodeficiencies, and AIDS. b. Up until AIDS came about, PML was very rare occurrence, and there were a small number of cases in the literature. Most physicians except neurologists and neuropathologists had never even heard of PML. But AIDS has changed that. 2. It is thought that the virus enters the brain in B lymphocytes. |
|
|
|
Gross Organs with PML lesions
|
1. [29] is a coronal section of the cerebral hemispheres of a patient with PML.
a. The myelin is affected asymmetrically. The white matter of one hemisphere is affected while the white matter of the other hemisphere is intact. b. This case was not AIDS related, it was a patient with leukemia. 2. [30] A close up of the same lesion. a. The cortical ribbon overlying the lesion looks fairly intact. b. However, it is not uncommon to see a microscopic reaction of the inner cortical layers. |
|
|
|
Microscopic Slides with PML lesions
|
1. The next three slides demonstrate all of the features of primary demyelination.
a. [31] A low power magnification of a cerebral gyrus with the cortex relatively intact. i. The myelin is lost from the white matter, seen as the zone of pallor beneath the cortex. b. [32] A myelin stain thru that area which stains intact myelin black i. You can see that there are no myelinated axons present. ii. There are macrophages that have picked up some of the degraded myelin, but not intact myelin sheaths at all. c. [33] A silver stain through that same area. (silver stain is for axons) i. Shows relative preservation of the axons. |
|
|
|
PML - In addition to the myelin lesions there are 2 other cell changes to recognize
|
a. [34] Oligodendroglial nuclei enlarge and there is effacement of the chromatin pattern.
i. This change occurs because there of the infection of the nucleus with the Papovavirus itself. • [35] Electron microscopy allows the identification of the viral nucleocapsids within the nuclei. They have linear and circular arrangements and are sometimes referred to as “spaghetti and meatballs” because of the long slender nucleocapids and the compact nucleocapsids. b. [36] Formation of irregular, bizarre nuclei within astrocytes, referred to as “transformed astrocytes.” i. They look like tumor cells, but glial tumors do not develop in association with PML. • However, it is possible to put Papovaviruses in experimental animals and produce tumors. ii. Dr. Nelson said that he’s not really sure what they are supposedly “transformed” into, but he thinks that the term “transformation” here means that the viral DNA has been insinuated into the DNA of the astrocyte nucleus, although you won’t find nucleocapsids if you look at it by EM. • The DNA has simply been inserted and these bizarre nuclei are present. But it apparently has zero neoplastic potential. |
|

