![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
52 Cards in this Set
- Front
- Back
|
Doing an awake CEA. Patient becomes confused & combative after carotid clamped and opened. Priority is...
a) tell surgeon to release clamp b) tell surgeon to place shunt c) induce GA d) give midazolam |
B
From OHA: Attentive monitoring of the patient is vital, particularly during crossclamping. If neurological deficit develops, a shunt should be inserted immediately, although you may have to use considerable tact/skill to reassure the patient, maintaining the airway whilst the shunt is being inserted. Recovery should be rapid once the shunt is in place—if it is not, convert to general anaesthesia. |
|
|
You intubate a young male patient for a left thoracotomy with a 39FG Robert Shaw tube. When you inflate both cuffs and ventilate the bronchial lumen you get left sided ventilation. When you attempt to ventilate the tracheal lumen the pressures are very high and you get no air entry. Yet when you deflate both cuffs you can ventilate the patient through the tracheal lumen. The most appropriate step to take next is:
A. Change to a 41FG tube B. Change to a 37FG tube C. Deflate both cuffs and insert further cm and recheck D. Deflate both cuffs and withdraw a few cm and recheck E. Pull ETT out and start again. |
C
From wiki: If you can ventilate BOTH lungs when cuffs are down (assume that is what they mean when they say you can ventilate the patient) then, when the bronchial cuff is inflated, it must be blocking the passage of air via the tracheal lumen, ie bronchial cuff is at the carina and tube needs to go in further. |
|
|
A patient comes to see you in clinic for a pneumonectomy for SCLS. His spirometry shows an FEV1 of 2.5L (>40% predicted). What do you advise about his fitness for surgery?
A. He is not fit for the procedure B. He is fit for the procedure C. He needs referral for formal exercise testing D. He needs a blood gas |
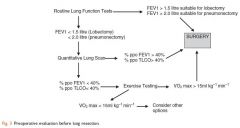
B
|
|
|
On bypass, for mitral stenosis repair immediately after cardioplegia the following happens:
MAP to 25 SvO2 80% CVP1 Next step in management: A) metaraminol B) give volume C) increase pump flows D) adrenaline infusion E) |
B
This scenario is common, it is all about finding the right balance in circulating volume, pump flow and vascular tone. I tend more towards volume and pump flow first before using drugs |
|
|
Redo CABG following median sternotomy surgeon states he has accidentally cut a vein graft, immediately followed by ST elevation on ECG and VF, next action.
A) External defibrillation 200J (Biphasic) B) Heparin This scenario is common, it is all about finding the right balance in circulating volume, pump flow and vascular tone. I tend more towards volume and pump flow first before using drugs IV then femoral cutdowns for bypass C) Hand ventilate with 100% oxygen D) GTN infusion E) metaraminol |
A > B – Follow ACLS
From Wiki: Spoke to a cardiac anaesthetist about this MCQ - he thinks that defibrillation is unlikely to be effective as the reason why you're in VF is you've suddenly rendered a part of the heart completely ischaemic. Yes, the chance of arrhythmias is higher given this is a redo and we always put pads on, but in this specific instance he thinks crashing onto bypass is more likely to save the day. It'll be interesting to see what the actual question says. |
|
|
Mitral valve replacement for Mitral stenosis. Pulmonary artery catheter in situ. Following separation from bypass, copious frank haemoptysis via ETT. Next step in management"
A) Insert double lumen tube B) Go back on bypass C) Give protamine D) Deflate and pull back PAC E) Perform fibreoptic bronchoscopy |
B
From Journal of Cardiothoracic and Vascular Anesthesia, Vol.15, Issue 3, Pg 377-380: Massive tracheobronchial hemorrhage during weaning from CPB is a rare but well-known and feared complication because of the high mortality rate. The largest number of reported cases have involved PA perforation from a PA catheter. The authors present 2 cases that illustrate there are other causes (this is presumed because there is no mention of the use of a PA catheter in either patient). These cases point out that there are general principles of management that apply whatever the cause of airway hemorrhage during CPB. First, these patients usually die from hypoxemia, not from hypovolemia, if the underlying cause of the hemorrhage is not diagnosed and treated. Second, oxygenation can be assured by resumption of CPB, and the anesthesiologist and surgeon must resist the temptation to wean rapidly and reverse the anticoagulation in the hope that this will stop the hemorrhage... If the patient is being weaned from CPB and extensive bleeding through the endotracheal tube is seen, the patient should be returned to CPB. This approach allows 2 maneuvers to occur: (1) determine site and mechanism of airway injury, and (2) initiate additional maneuvers that reduce the soilage of the lung by blood. Certain unique aspects of the management of PA perforation are subsequently discussed |
|
|
Young man on the ward post ORIF # tib/fib. On morphine PCA, high demands/bolus given ratio, used 40mg morphine in last 2 hours (or something else high). Is a bit drowsy but has severe constant leg pain. Next step in management
A. admit to intensive care B. increase bolus dose morphine PCA C. decrease lockout interval of PCA D. organise urgent orthopaedic review E. give more morphine until comfortable (or something else rubbish) |
D
Exclude compartment syndrome |
|
|
Patient with IV in right arm, has mediastinal mass and SVC compression undergoing mediastinal biopsy, suddenly uncontrolled surgical bleeding in mediastinum. Next step in management prior to thoractomy:
A. insert femoral cannulae and place on bypass B. insert IV in left arm C. insert IV into foot D. insert jugular CVC |
C
OHA: • Insert a 14 or 16G cannula in lower leg vein after induction (see below). • There is the potential for massive haemorrhage from the great vessels—the risk is increased in patients with SVC obstruction (hence the cannula in the leg): may require immediate median sternotomy. |
|
|
ASA grading was introduced to
A. predict intraop anaesthetic risk B. Predict intraop surgical and anaesthetic risk C. Standardise the physical status classification of patients D. Predict periop anaesthetic risk E. Predict periop anaesthetic and surgical risk |
C
ASA "In attempting to standardize and define what has heretofore been considered 'Operative Risk', it was found that the term ... could not be used. It was felt that for the purposes of the anesthesia record and for any future evaluation of anesthetic agents or surgical procedures, it would be best to classify and grade the patient in relation to his physical status only." |
|
|
Why does a proseal LMA provide a better airway seal?
A. More stable position due to oesophageal tube B. Doral cuff pushes ventral cuff...? C. Presence of oesophageal lumen D. Higher cuff pressure E. ? |
B
LMA Website: The LMA-ProSeal has a second dorsal cuff. This pushes the mask anteriorly to provide a better seal around the glottic aperture and helps to anchor the device in place |
|
|
Which of the following is the most frequent complication after use of LMA?
A. dysphagia B. dysarthria C. sore throat D. hoarse voice E. dry mouth |
E
Laryngeal Mask Anesthesia: Principles and Practice, 2nd Edn • Dry mouth 62-64% • Sore throat 13% • Dysphagia 11.5% • Dysarthria 5.3% |
|
|
What is true regarding arterial pressure transducer systems
A. Underdamping overestimates systolic BP B. Underdamping underestimates MAP C. Compliant tubing? |
A
|
|
|
Features of eaton lambert include all EXCEPT...
a) Associated with SCLC b) improvement with exercise c) defect in ACh release from motor end plate d) dry mouth e) Fatigue with exercise |
E
• A - False, i.e. is a feature. • B - False, i.e. is a feature. OHA, 2nd. ed. p. 250: "muscle weakness is improved by exercise" • C - False, i.e. is a feature. • D - False, i.e. is a feature. • E - True, i.e. is NOT a feature. OHA, 2nd. ed. p. 250: "muscle weakness is improved by exercise" |
|
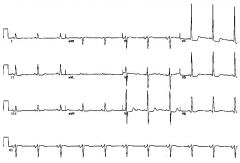
60 year old vascular patient. ECG given.
Showed large positive R waves in lateral leads, large negative S waves in anterior leads. ST depression laterally ie LVH with strain; bicuspid p waves A. LVH with strain B. Enlarged RA C. Lateral ischaemia D. LBBB E. L posterior hemiblock |
A
|
|
|
Pulsus paradoxus is:
A. Reduced BP on inspiration unlike normal (ie normally increased on insp) B. Reduced BP on inspiration exaggerated from normal C. Reduced BP on expiration unlike normal D. Reduced BP on expiration exaggerated from normal E. ? |
B
Miller's, 7th ed.: Pulsus paradoxus is an exaggerated inspiratory fall in systolic arterial pressure that exceeds 10 to 12 mm Hg during quiet breathing (see Fig. 40-16B).The term is confusing because a small inspiratory reduction in blood pressure is a normal phenomenon and pulsus paradoxus is not truly paradoxical, but rather an exaggeration of the normal inspiratory decline in blood pressure |
|
|
What antibiotics are required for bacterial endocarditis prophylaxis in a woman with MV prolapse for cholecystectomy.
A. None B. gentamicin C. ampicillin and gentamicin D. ampicillin E. cephazolin |
A
|
|
|
Male 60’s sudden onset of chest pain , L arm weakness and hoarse voice, ECG is unchanged from old (T inversion laterally), CXR normal, BP135/80, Pulse 110/min. Next step in management:
A)Aspirin B)SNP infusion C)GTN infusion D)Metoprolol E)Heparin |
D
Not a classical presentation of ischaemic chest pain, fits better with aortic dissection. From Emedicine on Aortic Dissection: • Patients with acute aortic dissection present with the sudden onset of severe and tearing chest pain, although this description is not universal... • Aortic dissection can be presumed in patients with symptoms and signs suggestive of myocardial infarction but without classic ECG findings... • Neurologic deficits are a presenting sign in up to 20% of cases... • Patients with peripheral nerve ischemia can present with numbness and tingling in the extremities, limb paresthesias, pain, or weakness... • Hoarseness from recurrent laryngeal nerve compression has also been described. • Chest radiography is the initial imaging technique and may or may not reveal any abnormality. An absence of mediastinal widening is observed in 40% of patients. Initiate medical therapy as soon as the diagnosis is considered. The goal is to decrease the blood pressure and the shearing forces of myocardial contractility in order to decrease the intimal tear and propagation of the dissection. Initiate therapy to reduce cardiac contractility. Administer drugs with negative inotropic effects, such as beta-blockers (the agents of choice); administer calcium channel blockers if beta-blockers are contraindicated. |
|
|
Plasma glucose level compared to blood glucose level
a)32% higher b)14% higher c)same d)14%lower e)32% lower |
B
|
|
|
You are called for a labour epidural. The woman is extremely distressed and in the middle of your consent process states “Just take my pain away” (The actual question stated that she refuses to listen to your repeated attempts at explaining the risks.). You:
A. Place epidural then when calmed return to advise her of risks and complications B. Explain she has to hear all the potential complications and refuse to place epidural without consent C. Take consent from partner D. Perform spinal to relieve pain, then consent her for epidural E. Go away and return when she is more cooperative |
A
From College Document P26: “1.3.2 Basic information about the proposed treatment should be provided, even if the patient requests no information. Where the patient clearly does not wish for further information, and states this wish, information should still be firmly offered and if still refused, that fact should be documented, and no further information forced on the patient." |
|
|
You are on call for a maternity hospital. Your junior registrar calls you after having inserted a labour epidural in an extremely anxious 19 yo parturient, and obtained blood in the catheter. He informs you the epidural space was found by LOR at 6cm and the catheter has been inserted to 12 cm. Your first instruction should be:
A. Flush with saline then check again for blood (NOT an option - option was just flush with saline and secure and use) B. Aspirate again for blood C. Give 3mls 2% lidnocaine with 1:200 000 adrenaline D. Pull back 2cm and check again for blood E. Remove epidural and start again |
D
|
|
|
Pre-eclamptic woman BP 180/110. Aim to drop BP to
a) 150-160 b) 140-150 c) 120-130 d) 110-120 e) 100-110 |
B
From Management of Pre-eclampsia and Eclampsia by Kate Briggs 3.2 Severe hypertension Severe hypertension is defined as systolic ≥160 mmHg or diastolic ≥ 110mmHg. Based on maternal mortality reports this degree of hypertension if left untreated is associated with an increased risk of intracerebral haemorrhage (Lewis 2007, Level IV). Reducing severe levels of hypertension decreases the risk of death (Podymow & August 2008, Level IV). Drugs that can be safely used include labetalol, nifedipine and hydralazine. There are different formulations of each of these and they change over time including availability for different routes of administration. The choice should be made on clinician familiarity and experience with a particular agent. Particular care should be taken to avoid precipitous falls in blood pressure which may induce maternal or fetal complications as a result of falling below critical perfusion thresholds. Blood pressure should be lowered to levels of SBP 140-150/DBP 90-100 at a rate of 10-20 mmHg every 10-20 minutes. Consideration should also be given to the extent of placental transfer of the administered drug and the direct effect of the agent and any metabolites. |
|
|
Option associated with highest likelihood of motor block with labour epidural analgesia:
A)Nurse initiated epidural topups B)Anaesthetist initiated epidural topups C)PCEA D)Continuous epidural infusion E)All associated with same motor block |
D
British Journal of Anaesthesia, 2002, Vol. 89, No. 3 459-465 "Patient-controlled epidural analgesia versus continuous infusion for labour analgesia: a meta-analysis" demonstrated the PCEA was associated with less motor block cf CEI |
|
|
Trauma pregnant patient (?32wks) BP 70/40, P 50, intubated in emergency department, next management step:
A)L tilt pelvis B)IV fluid bolus C)Arrange urgent caesarean section D)Vasopressor options (?Adrenaline, Metaraminol) |
A
|
|
|
Emergency caesarean section for foetal distress (and foetal acidosis on scalp probe?). what is best option to raise gastric pH preop:
A)Oral Na Citrate B)Ranitidine IV C)Ranitidine oral D)Omeprazole IV E)Omeprazole oral F)Metoclopramide 20 IV |
A
|
|
|
70 year old man having lung resection for SCC of left lung FEV1 2.3L (? % predicted), FVC 3.5L (? % predicted). Do you...
A. Accept for lobectomy or pneumonectomy B. Decline pneumonectomy, proceed to lobectomy C. Cardiopulmonary exercise testing D. Differential V/Q scan E. Decline both pneumonectomy and lobectomy |
A
|
|
|
Which distinguishes C8-T1 from an ulnar nerve lesion at elbow?
A. Paraethesia of the 5th digit B. Paraesthesia over index finger C. Flexor carpi ulnaris function D. Paraesthesia/sensory loss over medial forearm E. Adductor pollicis function |
D
Medial cutaneous nerve of forearm formed from brachial plexus; ulnar nerve supplies sensation to hand. The medial cutaneous nerve of the forearm arises from the medial cord of the brachial plexus which is prior to the formation of the ulnar nerve. |
|
|
Asking the patient to look up and in during a retrobulbar block increases the risk of injury to:
A. Inferior oblique B. Superior oblique C. optic nerve D. globe E. ophthalmic artery |
C
From “Regional anaesthesia for eye surgery” Regional Anesthesia and Pain Medicine, Vol 30, No 1 (January–February), 2005: pp 72–82: The Atkinson “up and in” position of the gaze was abandoned when Liu et al. and Unsöld et al. confirmed that it increased the risk of optic nerve injury |
|
|
A man presents for an ankle fusion. Which of the following combinations will provide the best block:
A. Sciatic nerve B. Common peroneal and saphenous C. Tibial and saphenous D. ?Sural and tibial E. Ankle block |
A
Need to block sciatic and saphenous nerves |
|
|
Stellate ganglion block associated with all except:
A. Ptosis B. Meiosis C. Sweating D. Facial flushing E. Nasal stuffiness |
C
What's not in a Horner's? Sweating... C. You get anhydrosis as sweating is sympathetically mediated |
|
|
Spinal anaesthesia, T3 level
A. bradycardia due to unapposed vagus B. autonomic response more if lever higher C. ? |
A
|
|
|
18yo patient in a psych unit, being treated for frequent vomiting. Collapses and found unconscious.
ABG's: pH 7.22 CO2 40 PO2 100 HCO3 16 Na 138 K 4.0 Cl 105 Diagnosis is: A. anorexia nervosa B. diabetic ketoacidosis C RTA D. Normal saline administration E) Gastric outlet obstruction |
V
High anion gap metabolic acidosis with normal chloride - only one that fits is DKA. RTA, anorexia nervosa (laxative abuse) and N/S (hyperchloraemic) are associated with normal anion gap acidosis; and gastric outlet obstruction is associated with a hypokalaemic hypochloraemic metabolic alkalosis. |
|
|
60yo with history of hypertension. Presents with chest pain, hoarse voice, left arm weakness. Has lateral T-wave changes on ECG, also present on an old ECG. Heart rate 110, BP 130/80 (definitely this value), SpO2 96% or something. First drug to give:
A. aspirin B. metoprolol C. GTN D. nitroprusside E. Heparin |
B
|
|
|
Trauma patient with GCS 6 with hard collar. HR and BP unstable. What is the best way of clearing neck?
A. CT B. Cervical spine trauma series C. MRI D. Leave had collar indefinitely?? E. Clinically |
D
|
|
|
Alt 6 hour post pituitary surgery, Serum Na 153, next step in management
a)Dext 5% b)Normal saline c)DDAVP cant remember other options |
C
|
|
|
Neonate if febrile with rash and periodic breathing. which is likely ABG?
a) metab acidosis resp acidosis b) metab acidosis compensated c) resp acidosis d) alkalosis e) alkalosis |
?A - not sure what this ones about
|
|
|
2 month old systolic murmur heard at apex no change with posture, now on 5th centile for weight after being on 30th at birth, mother states has difficulty feeding. Peripheral pulses reduced femoral more than upper body. Most likely cause:
A. HOCM B. VSD C. PDA D. venous hum E. ASD |
C
Talley + O'Connor 3rd Ed. PDA - collapsing pulse with sharp upstroke from ejection of large volume of blood into empty aorta during systole, low diastolic pressure due to rapid decompression of aorta, hyperkinetic apex, single S2 if large or even reversed splitting of S2, continous loud "machinary murmur at 1st LIC space. sometimes associated with flow murmur through left heart eg. mitral mid diastolic murmur. |
|
|
4 yr old presents for elective surgery, otherwise fit healthy, murmur at left sternal edge on auscultation heard in systole and diastole, disappears on lying down. Most likely cause:
A. HOCM B. VSD C. PDA D. venous hum E. ASD |
Talley&O'connor 3rd Ed p79-83 and wikipaedia
Venous Hum - systolic + diastolic components, not really a murmur. Benign medical condition where 20% of the blood flow travels to the brain and back to the heart. Due to the large amount of blood it can move quite fast causing the vein walls to vibrate which can create a humming noise to be heard by the patient. The murmur disappears when the patient is in the supine position. |
|
|
18/12 old undergoing routine SV GA under LMA. Sudden onset SVT with HR 220 BP 84/60 ETCO2 32 SpO2 98.Management:
A. Adenosine 100mcg B. DCR 2J/kg C. DCR 4J/kg D. Amiodarone 5mg/kg E. CPR |
A
Assuming A is supposed to be 100mcg/kg From APLS guideline Management of SVT in a child: • Attempt valsalva maneuvers as able by child, ie; forceful cough, cold packs on face and neck, or blow through a straw • Establish IV/IO NS. Do not withhold IO if unable to start IV promptly and child is unstable • If unable to maintain airway, consider endotracheal Intubation • If child is rapidly deteriorating perform immediate synchronized cardioversion at 0.5J/kg. Consider pain management or sedation • If time allows may try Adenosine first at 0.1mg/kg IV or IO, being sure to administer rapidly and follow with a rapid fluid flush. During administration, record a rhythm strip. • Consider Amiodarone. |
|
|
What is the appropriate LMA size for an 8kg child:
A. 1 B. 1.5 C. 2 D. 2.5 E. 3 |
B
LMA sizes (Drug Doses Frank Shann Book) <5kg = 1 5-10kg = 1.5 10-20kg = 2 20-30kg = 2.5 30-50kg = 3.0 50-70kg = 4.0 70-100kg = 5.0 100kg = 6 |
|
|
Neonate born to known drug abusing mother brought to emergency department by grandmother, unwell lethargic, slightly jaundiced, ABG shows following:
pH 7.52 Na 135 Cl 87 K 3 pCO2 38 Which of the following is the Diagnosis? A) Septicaemia B) Hepatitis C) Pyloric stenosis D) Pneumonia E) Opioid withdrawl |
C
|
|
|
15kg child found fitting on paeds ward ?24h ?48h postop while on infusion of 60ml/h ½ NS + Dextrose. Now intubated. Na is 119, next management step:
A) frusemide B) hypertonic saline C) Normal saline at 20ml/hr D) Water restrict E) Phenytoin |
B
Symptomatic hyponatraemia = hypertonic saline. From OHA p.180: Acute symptomatic hyponatraemia. Aim to raise serum Na by 2mmol/hr until symptom resolve. Complete correction is unnecessary, although not unsafe. Infuse hypertonic saline (3% NaCl) at a rate of 1.2-2.4ml/kg/hr through a large vein... If there are severe neurological symptoms, eg seizure, coma, 3%NaCl may be infused at 4-6ml/kg/hr. Electrolyte should be carefully monitored. |
|
|
A man on PCA controlled with 2 mg morphine bolus is having a lot of pruritus. You decide to switch him to fentanyl. Which dose is the most appropriate bolus to be equi-analgesic with morphine 2mg:
A. 10mcg B. 20mcg C. 40mcg D. 60mcg E. 80mcg |
C
A bit of a tricky question - a straight conversion would be 20mcg. However, according to APMSE, the optimal dose of a morphine PCA is 10mcg, while fentanyl might be 30 or 40mcg. So while from a efficacy point of view the equivalent dose would be 20mcg, clearly clinically it is not. Nearly all morphine PCAs start 1 mg but I can't remember the last time I've seen a fentanyl PCA at 10mcg (except in little old ladies)... Votes? Though in the APMSE it does make the point that the higher doses of fentanyl were infused over 10mins, possibly altering the effect of that dose. It also asks about the equi-analgesic dose as opposed to the most effective dose, if this isn't splitting hairs too much. |
|
|
A patient with chronic pain using morphine PCA after lower limb orthopaedic surgery. Daily usage of IV morphine works out at about 400mg/day. What dose of oral methadone would you start him on to replace the morphine?
A. 60mg/day B. 120mg/day C. 400mg/day D. 600mg/day E: 1200mg/day |
A
Methadone replacement depends on dose of oral morphine Daily Dose : Conversion Ratio : <100mg 3:1 100 - 300mg 5:1 300 - 600mg 10:1 600mg - 800mg 12:1 800mg - 1000mg 15:1 >1000mg 20:1 400mg IV = 1200mg oral. 20:1 conversion so 60mg of methadone per day = A |
|
|
For muscle relaxant,placing the nerve stimulator to stimulate FPB (Flexor pollicis brevis) compared to Abductor pollicis brevis is likely to
A. show a slower recovery to NMB B. show the same recovery C. show a faster recovery to NMB Cannot remember other options |
B
From Wiki Was this supposed to be flexor hallicus brevis? That would make a lot more sense as when you stimulate the ulnar nerve both APB and FPB can be stimulated but no one actually monitors FPB. On the other hand FHB would make sense as you may not have access to the arm (or can't see it). There are lots of papers comparing FHB and APB including this review (Monitoring neuromuscular block: an update Anaesthesia Volume 64, Issue s1, Pages 82-89) which says the two sites are clinically equivalent |
|
|
Aneursym clipping, Best monitor of depth of block during this is
A. TOFR B. TOFC B. DBS C. PTC |
C
|
|
|
Closed circuit anaesthesia with 70%N2O,70kg man (low flow i think) what is the uptake of N2O after 90 mins anaesthesia:
A. less than 50ml/min B. 100ml/min C. 200ml/min D. 500ml/min E. 1000 ml/min |
B
Severinghaus equation (Miller 87) – uptake = solubility x CO x A-V difference x proportion of inspired gas mix. Old question - uptake is 1000 divided by the square root of the time administered in minutes |
|
|
Rapid infusion of mannitol IV initially causes:
A. Raised ICP B. Reduced CBF C. Reduced K D. Reduced Na E. ? |
A
The physical bolus of Mannitol causes an initially transient increase, then decreases as interstitial water is drawn out |
|
|
Granisitron, which is incorrect:
A) Decreased serotonin release B) Metabolism by carbamoyl ?... C) 5HT3 antagonism |
Maybe B? - metabolism involves N-demethylation and aromatic ring oxidation followed by conjugation, nothing to do with carbamoyl something
|
|
|
Who has got minimum effect on ICP at 1 MAC
a)isoflurane b)sevoflurane c)desflurane d)enflurane e)halothane |
B
|
|
|
An ABG showing a raised anion gap. Which of the following would explain this ABG?
A. Salicylate poisoning B. DKA C. Lactic acidosis D. 6L of normal saline (or did this option belong to another Q?) |
A, B, C
Is this supposed to be a which does not question? |
|
|
Young woman with subarachnoid haemorrhage, hyponatraemia and increased urinary sodium (did not specify if high sodium concentration or total amount lost). What is likely cause?
A. cerebral salt wasting syndrome B. SIADH C. HHH therapy D. Excess NS administration E. diabetes insipidus |
B
CEACCP 2008 CSWS is usually caused by brain injury/trauma or cerebral lesion, tumor, or hematoma. CSWS is a diagnosis of exclusion and may be difficult to distinguish from the syndrome of inappropriate antidiuretic hormone (SIADH), which develops under similar circumstances and also presents with hyponatremia. The main clinical difference is that of total fluid status of the patient: CSWS leads to a relative or overt hypovolemia whereas SIADH is consistent with a normal to hypervolemic range. Random urine sodium concentrations tend to be lower than 100 mEq/L in CSWS and greater in SIADH. If blood-sodium levels increase when fluids are restricted, SIADH is more likely. The biochemical criteria for CSWS are: (i) low or normal serum sodium (ii) high or normal serum osmolality (iii) high or normal urine osmolality (iv) increased haematocrit, urea, bicarbonate, and albumin as a consequence of hypovolaemia. However, these criteria are often inconclusive. In CSWS, total daily urine sodium excretion is greater than intake, whereas it is usually equal to intake in SIADH, that is, overall sodium balance is negative in CSWS and generally neutral in SIADH. |
|
|
Which of the following can be used to describe the spread of non-parametric data?
A. standard deviation B. interquartile range C. confidence interval D. standard error E. variance coefficient |
B
Continuing Education in Anaesthesia, Critical Care & Pain | Volume 7 Number 4 2007 " The interquartile range (IQR) is often quoted when referring to interval data that is not normally distributed." |

