![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
45 Cards in this Set
- Front
- Back
|
When hearing loss occurs following spinal anaesthesia it is usually in which of the following frequency ranges:
A 125 - 1000 Hz B 1500 - 3000 Hz C 3500 - 5500 Hz D 6000 - 10000Hz E > 11000Hz |
A
Low frequency (125-1000Hz) hearing loss. A study in Anaesth Analg 2002; 94: 1318-20 which looked at young vs old pts also quoted low frequency loss (125-500Hz) |
|
|
Each of the following drugs act at the DOP (delta receptor) EXCEPT
A diamorphine B fentanyl C morphine D naloxone E pethidine |
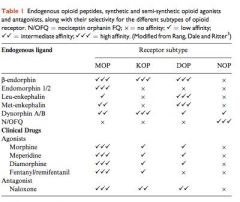
B
|
|
|
Patient burns during MRI can be associated with each of the following EXCEPT
A high intensity changing magnetic fields B looped monitoring lines ... C non ferromagnetic material in contact with the patient D cosmetics worn by the patient (which do not contain metals) E temperature monitoring with thermister probes |
D
Blue Book 2005: “Tattoos and make-up: Some tattoos and make-up contain metal pigments. These can cause image artefact or heat, causing skin discomfort, although burns have not been reported.” There are case-reports of 1st degree burns with non-ferrous permanent cosmetics (i.e. essentially cosmetic tattoos, such as eyelid line) http://www.ajronline.org/content/187/5/W556.full Doesn’t appear to be any danger from normal make-up cosmetics though. |
|
|
Preoperative assessment shows a malampati (ML) score of III and thyromental distance (TMD) of < 6cm. A grade 3 to 4 on Cormark and Lehanes is predicted. Compared to the ML score, the TMD is:
A less sensitive, less specific B less sensitive, more specific C more sensitive, less specific D more sensitive, more specific E equal sensitivity an specificity |
B
Numbers differ broadly depending which article you read, but trend is the same: Anesthesiology 2005 (103) 429-37: • TMD: sens 20%, spec 94% • Mall: sens 49%, spec 86% A&A 2005 (101) 1542-5 concurs: • TMD sens 52, spec 71; • Mall sens 70, spec 60) |
|
|
In performing an awake fibreoptic intubation it is MOST important that care is taken to avoid:
a. Causing any bleeding that will obstruct view b. Oversedation as leads to posterior pharyngeal wall collapse c. Trauma to nasal turbinates d. Touching vocal cords as will induce coughing e. Oral route as may bite the fibreoptic scope |
B
Negating the safety of AFI if the patient become over sedated |
|
|
CT reprint showing large multidoular goitre. Uppermost concerns to anaesthetist is
a. Involvement of the Right carotid artery b. Tracheal deviation to the left c. Tracheal deviation to the right d. Malignant involvement of the paratracheal nodes e. compression of upper lobe of rt.lung |
D
|
|
|
PAC seeing patient with thyroid disease. Most reassuring factor for normal thyroid function is:
A. Absence of 'hot' nodules on nuclear scan B.? C. Normal heart rate D. Normal temperature E. Absence of any antithyroid medications |
C
Probably poorly remembered question You could have absence of ‘hot nodules’ but still be hyperthyroid (eg. Grave’s, with global high uptake, but no nodule per se) Also, you could have absence of ‘hot nodules’ and be hypothyroid – which is not ‘normal thyroid function’ |
|
|
T1 injury. Patient now 4 weeks post and going to theatre for sacral pressure area debridement. Feature most unlikely to reflect autonomic dysreflexia
A. ? B. Bradycardia C. Severe hypotension D. ? E. Goose bumps below T1 level |
C
From OHA page 240 Autonomic dysreflexia is characterised by massive, disordered automonic response to stimulation below the level of the lesion. It is rare in lesions lower than T7. Incidence increases with higher lesions. It may occur within 3wk of the original injury but is unlikely to be a problem after 9 months. The dysreflexia and its effects are thought to arise because of a loss of descending inhibitory control on regenerating presynaptic fibres. Hypertension is the most common feature but is not universal. Other features include headache, flushing, pallor ( may be manifest above the level of lesion, nausea, anxiety, sweating, bradycardia and penile erection. Less commonly pupillary changes or Horner’s syndrome. Dysreflexia may be complicated by seizures, pulmonary oedema, coma or death and should be treated as a medical emergency. Stimuli to trigger Urological: bladder distension, UTI, catheter insertion; Bowel obstruction; Acute abdo; Fractures |
|
|
With regard to fire in OT
A. Mainly caused by laser surgery B. Decreased incidence since cessation of use of cyclopropane and ether C. Need fuel, ignition source and oxidizing agent D. ? E. ? |
C
Anesthesiology May 2008, 108(5): "fire triad", oxidizer, ignition source, fuel |
|
|
Visual loss post-operatively
a. more common after external ocular compression b. incidence 1 in 200,000 c. most common after spinal surgery d. incidence independent of duration of surgery e. more common after isovolaemic haemodilution |
E
• A – False, Ischaemic optic neuropathy (ION) accounts for 89% • B – False, 1:125 000 overall surgery (CEACCP) • C - Surgery is most common cause o Anesthesiology 2006; 105:652–9 The American Society of Anesthesiologists Postoperative Visual Loss Registry. Analysis of 93 Spine Surgery Cases with Postoperative Visual Loss: Spine 0.2% Cardiac 4.5% • D – False, association with surgery> 6hrs or blood loss > 1L • E – True “The cause-and-effect relationships associated with ION are uncertain, but low arterial pressure, low hematocrit, and lengthy surgical procedures are statistically associated with the phenomenon." (Miller Ch 63) |
|
|
Cause for hoarse voice after anterior spinal surgery
a. glossopharyngeal nerve palsy or lesion b. recurrent laryngeal nerve palsy or lesion c. superior laryngeal nerve or lesion d. airway oedema e. prolonged intubation |
D
|
|
|
Features most suspicious for myocardial ischaemia
a. ST depression 2mm during fem pop bypass in 60 yo man under spinal b. T wave inversion in fem pop bypass in 60yo under spinal c. 0.7mm ST elevation in fem pop bypass in 60 yo man under spinal d. SAH in young man e. 32 yo woman during LSCS |
A
Criteria for stress-induced ischemia: ≥1 mm (0.1 mV) of horizontal or down-sloping ST-segment depression in at least three consecutive beats with a stable baseline |
|
|
The Line Isolation Transformer
a. ? b. ? c. Provides low current to the line isolation monitor d. Separates earth from the OT electrical supply (similar wording) e. ? |
D
|
|
|
DC cardioversion - LEAST likely indicated for
A atrial fibrillation B atrial flutter C multifocal atrial tachycardia D paroxysmal atrial tachycardia E ventricular tachycardia |
C
Chest Jan 1998 states that MAT is "not responsive to cardioversion and that it may precipitate hypotension due the underlying sepsis or PE" |
|
|
Hypercalcaemia due to hyperparathyroidism is associated with
A an elevated GFR B prolonged QT C short PR interval D polyuria polydipsia E skeletal muscle rigidity |
D
Hypercalcaemia / hyperparathyroidism is associated with impaired renal function, shorter QTc, prolonged PR and muscular weakness. Westmead Pocket Anaesthetic Manual, 2nd. ed. / Hypercalaemia (in general): Shortened QT interval, prolonged PR and QRS intervals, T wave flattening and widening, AV nodal blocking to complete heart block. |
|
|
Suprapubic prostatectomy bleeding excessively. Need to exclude primary hyperfibrinolysis. Most useful test would be
A clot retraction time B plasma fibrinogen estimation C prothrombin time D thromboelastography E whole blood clotting time |
D
Evaluation of rotation thrombelastography for the diagnosis of hyperfibrinolysis in trauma patients Br J Anaesth 2008; 100: 792–7: Levrat- “Background. Blood loss and uncontrollable bleeding are major factors affecting survival in trauma patients. Because treatment with antifibrinolytic drugs may be effective, early detection of hyperfibrinolysis with rotation thrombelastography (ROTEMw) may be beneficial. Conclusions. ROTEMw provided rapid and accurate detection of hyperfibrinolysis in severely injured trauma patients” |
|
|
While of the following statements regarding patients with ankylosing spondylitis are FALSE
A amyloid renal infiltration is rarely seen B cardiac complications occur in <10% of cases C normovolaemia anaemia occurs in over 85% of cases D sacroileitis is an early sign of presentation E uveitis is the most common extra articular manifestation |
C
• A - TRUE. Amyloidosis is a very rare complication of ankylosing spondylitis in patients with severe, active, and long-standing disease. These patients generally have active spondylitis, active peripheral joint involvement, and an elevated erythrocyte sedimentation rate (ESR) and C-reactive protein level. This may result in renal dysfunction with proteinuria and renal insufficiency or failure.[5] (http://www.emedicine.com/MED/topic2700.htm) • B - TRUE. Cardiovascular involvement of clinical significance occurs in fewer than 10% of patients, typically those with severe long-standing disease. However, subclinical disease can be detected in many patients and may occur as an isolated clinical entity in association with HLA-B27[6] (http://www.emedicine.com/MED/topic2700.htm) • C - FALSE. Approximately 15% of patients may present with a normochromic normocytic anemia of chronic disease.[7] (http://www.emedicine.com/MED/topic2700.htm) • D - TRUE. • E - TRUE. Uveitis is the most common extra-articular manifestation, occurring in 20-30% of patients with ankylosing spondylitis. Of all patients with acute anterior uveitis, 30-50% have or will develop ankylosing spondylitis. The incidence is much higher in individuals who are HLA-B27–positive (84-90%).[8] (http://www.emedicine.com/MED/topic2700.htm) --SG 10:37, 23 Oct 2008 (EDT) |
|
|
COPD patient with pulmonary hypertension and acute RHF. Treatment
a. 100% oxygen will decrease the pulmonary artery pressure b. Sildenafil will be useful for treating RHF c. Noradrenaline is an appropriate inotrope for this patient d. ? e. ? |
B
• Seems most appropriate first measure • Evidence for use of sildenafil in acute PHTN post cardiac surgery and acute RHF from PE: o http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1276328/ o Sildenafil in acute pulmonary embolism: case report and review of literature. JICS Volume 10, Number 1, January 2009 • Noradrenaline is an appropriate vasopressor, but there are better inotropes in RHF |
|
|
Post op patient (surgery 3/7 ago). Patient dyspnoeic. V/Q scan organized which shows non segmental matched perfusion/ventilation defects. This is consistent with
a. Atelectasis b. COPD c. Pulmonary embolus d. Pneumonia e. Pulmonary infarction |
A
Ventilation perfusion scintigraphy - Emergency Medicine Clinics of North America 19(4), p957-974 A. TRUE: Non segmental, (i.e. won’t see ventilation or perfusion deficit that corresponds to particular lobar segment; both pulmonary capillaries and alveoli are compressed) matched defects B. ~false: COPD - Multiple, Segmental, peripheral, bilateral, matched C. ~false: Pulmonary embolus - Mismatched, Segmental I think (more V than Q) D. ~false: Pneumonia - Reverse mismatch, segmental I think (more Q than V) E. ~false: Pulmonary infarction - Mismatched, segmental (same as PE, more V than Q) |
|
|
A 25yo primipara with an uncomplicated pregnancy presents to delivery suite in labour at term. Her membranes spontaneously rupture soon after, and it is blood-stained. At the same time, a severe foetal bradycardia appears on the CTG. What is the most likely cause of this?
A. Placenta accreta B. Placental abruption C. Uterine rupture D. Vasa praevia E. True knot in the umbilical cord |
D
• Vasa praevia is an obstetric complication defined as "fetal vessels crossing or running in close proximity to the inner cervical os. These vessels course within the membranes (unsupported by the umbilical cord or placental tissue) and are at risk of rupture when the supporting membranes rupture." • These vessels may be torn at the time of labor, delivery or when the membranes rupture. It has a high fetal mortality because of the bleeding that follows. The blood lost is foetal not maternal blood hence the high mortality. • The classic triad are membrane rupture followed immediately by painless vaginal bleeding and fetal bradycardia |
|
|
Patient with placenta acreta. Surgical management MOST likely to save her life
A B lynch suture around the uterus for external tamponade B Rusch balloon in the uterus for internal tamponade C ligation of the internal iliac arteries D ligation of the uterine arteries E subtotal or total hysterectomy |
E
Page 731 2nd edition OHA • B-lynch suture is for uterine atony after caesarean • Balloon tamponade can be used for atony or lower segment bleeding • Arterial ligation does not appear to be that helpful due to collateral supply |
|
|
After a difficult thyroidectomy for thyroid carcinoma, a 63 year old woman develops stridor immediately following extubation. The most likely cause is
A hypocalcaemia B neck oedema C recurent laryngeal nerve palsies D tracheomalacia E vocal cord oedema |
C
|
|
|
Patient with traumatic brain injury has the following readings. Global CSF flow measured at 15ml/100gm/min while the CMRO2 is measured at 3.5ml/100gm/min. There is
A appropriate coupling of cerebral perfusion and cerebral metabolism B autoreguation of cerebral vasodilation C cerebral hypoperfusion D cerebral ischaemia E reperfusion injury |
C
From wiki: 15 ml of blood carries 0.015 X 200ml (normally about 200 ml of O2 per litre of blood) = 3 ml. Delivery ~ 3 ml/100g/min : Requirement 3.5 mL/100g/min. NB normal CBF is 750 ml/min or 50 ml/100g/min not 15 |
|
|
55 year old subarachnoid haemorrhage secondary to aneurysm. Patient is confused with a occulomotor (3rd cranial nerve) palsy, complains of a severe headache. This patient is in Hunt and Hess class:
A 0 B 1 C 2 D 3 E 4 |
D
Hunt and Hess: 1. Asymptomatic, mild headache, slight nuchal rigidity 2. Moderate to severe headache, nuchal rigidity, no neurologic deficit other than cranial nerve palsy 3. Drowsiness / confusion, mild focal neurologic deficit 4. Stupor, moderate-severe hemiparesis 5. Coma, decerebrate posturing |
|
|
Traumatic brain injury with central diabetes insipidus. Can be managed with
A democlocydine B desmopressin C fludrocortisone D fluid restriction E frusemide |
B
|
|
|
Called to ward for Postoperative thyroidectomy bleeding in ward. SpO2 92% on 6L, tachycardic and ?hypertensive and neck haematoma. What is the least appropriate management:
a. call and arrange CT scan of his neck b. call OT and arrange urgent surgery c. release staples d. increase oxygen supply |
A
|
|
|
Hypertensive female at 38 weeks gestation BP 180/110. CTG shows no foetal distress. First Hb 110 and second is 109. First plt count 90 then drops to 40. AST increases from 50 to ? 120. Most appropriate management is
a. deliver the baby b. various antihypertensive medication options c. 20mg frusemide d.? e.? |
B
This paints a picture of HELLP syndrome. Control of BP and seizure should be first priority followed by delivery of the baby |
|
|
Post bypass 3 vessel CABG. Hypotensive and ECG shows ST elevation in II, aVF CVP 15mmHg PAP 25mmHg with normal SVR and PVR. What is most likely to be seen on TOE
a. early diastolic augmented flow ct atrial systolic flow b. Inferior hypokinesis (of the left ventricle) c. RV failure and TR d. Empty left ventricle following systole e. Mitral regurgitation |
B
Given ST elevation in II, aVF, inferior ischaemia/infarct is most likely cause |
|
|
The left recurrent laryngeal nerve
A hooks around the arch of the aorta anterior to the attachment of the ligamentum arteriosum B passes under cover of the lower border of the inferior constrictor muscle before entering the larynx C supplies the cricothyroid muscle D supplies sensation to the whole of the laryngeal mucosa on the left side E contains motor fibres derived from the spinal root of the accessory nerve |
A
A. False - posterior to ligamentum arteriosum B. TRUE C. False innervates all intrinsic muscles of the larynx except the cricothyroid D. False supplies sensation to mucosa BELOW the cords (Superior laryngeal nerve above cords) E. False Vagus nerve. |
|
|
The ascending aorta
A has no branches B begins at the semilunar valve C arises from right ventricle D occupies the superior mediastinum E lies inferior to the SVC |
B
A - false: The ascending aorta gives off the left and the right coronary arteries. B - ?true: The aortic valve (like the pulmonary valve) is a semi-lunar valve C - false: left ventricle! D - false: occupies the middle mediastinum E - false: lies to the left and anterior to the SVC |
|
|
The nerve providing sensory supply to the airway muscle below (inferior to) the vocal cords is the
A phrenic nerve B posterior thyroid nerve C recurrent laryngeal nerve D superior laryngeal nerve E tracheal nerve |
C
?? perhaps they meant mucosa. Answer would be C. The recurrent laryngeal nerves provide the motor supply to the intrinsic muscles of the larynx apart from cricothyroid, as well as the sensory supply to the laryngeal mucosa inferior to the vocal cords |
|
|
Ciliary ganglion
A sympathetic from inferior cervical ganglion B located inferiorly within orbit C may be damaged during a peribulbar block D preganglionic parasympathetic supply from the supra trochlear nerve E preganglionic parasympathetic originates from the Edinger Westpal nucleus |
E
The ciliary ganglion lies near the apex of the orbit between the optic nerve and the rectus lateralis. It is a tiny structure, about 1 mm in diameter, which receives parasympathetic, sympathetic and sensory fibres. Its parasympathetic component is derived from the oculomotor nerve (III) via its branch to the inferior oblique muscle, these fibres originating in the Edinger–Westphal nucleus (see p. 242). Relay takes place in the ciliary ganglion and postganglionic fibres then pass in the short ciliary nerves, about six in number, to the eyeball, where they supply the sphincter pupillae and the ciliary muscle. Stimulation results in pupillary constriction and in accommodation of the lens. Sympathetic fibres reach the ganglion from the superior cervical ganglion via the internal carotid plexus. Sensory fibres are derived from the nasociliary branch of the ophthalmic nerve. Both the sympathetic and sensory components pass through the ciliary ganglion without synapse to reach the eye via the short ciliary nerves, where they are respectively vasoconstrictor and sensory to the globe of the eye. (Note that the majority of sympathetic dilator pupillae nerve fibres are transmitted to the eye in the long ciliary branches of the nasociliary nerve.) |
|
|
You are seeing a 60yo man in the pre-anaesthetic clinic before his right total knee replacement. He weighs 70kg and apart from his osteoarthritis is fit and well. You discuss with him the options of a general anaesthetic with multi-modality analgesia and enoxaparin postoperatively as well as the option of an epidural for both the anaesthetic and post operative pain management. What is incorrect regarding the epidural?
A. It will shorten his hospital stay and accelerate his rehabilitation B. It will give him better pain relief particularly for the CPM machine C. It will reduce his risk of myocardial ischaemia D. There will be little difference in his risk of thromboembolism. E. If he has no sedation, his risk of post-operative delirium and cognitive impairment will be reduced |
C
A- True B- True Better analgesia with all techniques of epidural anaesthesia (in particular with movement) as compared to parenteral opioids C- False( correct answer): only true for thoracic epidurals extended for more than 24hrs, not lumbar epidural for RTKJ Replacement. D- True, only difference is with graft occlusion in peripheral vascular surgery, not orthopaedics and DVT where DVT prophylaxis has been used. E- true |
|
|
Effect of Injecting 5 mL of saline into the epidural space:
A. Increase incidence of patchy block B. Decreased risk of epidural vein catheterisation C. No effect D. Increased ease of threading catheter E. ? Decreased effectiveness of block |
B
Predistention of the Epidural Space Before Catheter Insertion Reduces the Incidence of Intravascular Epidural Catheter Insertion. Ananesthesia & Analgesia - August 2007 vol. 105 no. 2 460-464 |
|
|
PDPH
A. Iv caffeine treatment used to relieve symptoms. B. Is usually frontal headache C. Bed rest for 24 hrs is beneficial D. No use if blood patch done after 48 hrs. E. Usually manifests within first 4 hrs. |
B
Post-dural puncture headache: pathogenesis, prevention, and treatment - BJA 91 (5): 718-29 (2003) • "The most frequently quoted work on the treatment of post-dural puncture headache with caffeine is that of Sechzer. He evaluated the effects of one or two 0.5 g doses of i.v. caffeine on subjects with established post-dural puncture headache. There are some statistical and methodological flaws in this study, but it was concluded that i.v. caffeine is an effective therapy for post-dural puncture headache." • " There is no clinical evidence to support the maintenance of the supine position before or after the onset of the headache as a means of treatment." • " Headache is the predominant, but not ubiquitous presenting complaint. The headache is described as severe, `searing and spreading like hot metal'. The common distribution is over the frontal and occipital areas radiating to the neck and shoulders." • " Ninety per cent of headaches will occur within 3 days of the procedure, and 66% start within the first 48 hours." |
|
|
A terrorist attack has taken place involving the nerve gas "VX". Some victims have arrived in the emergency department. The most appropriate management of this situation is to:
A. Strip them off and hose them down B. Strip them off, scrub them with a brush, and hose them down C. Leave their clothes on and hose them down D. Leave their clothes on, scrub them with a brush, and hose them down E. Take them to the resuscitation area and put in an IV |
A
Emedicine Abrading the skin by scrubbing will increase absorption of these agents as per e-medicine and CDC website states priorities are removal from hot zone, cut off clothing, wash with soap and water or hypochlorite solution. |
|
|
Another GCS question – open eyes to command, withdrawing from pain, confused conversation:
A. 8 B. 9 C. 10 D. 11 E. 7 |
D
Best Eye Response. (4) 1. No eye opening. 2. Eye opening to pain. 3. Eye opening to verbal command. 4. Eyes open spontaneously. Best Verbal Response. (5) 1. No verbal response 2. Incomprehensible sounds. 3. Inappropriate words. 4. Confused 5. Orientated Best Motor Response. (6) 1. No motor response. 2. Extension to pain. 3. Flexion to pain. 4. Withdrawal from pain. 5. Localising pain. 6. Obeys Commands. |
|
|
Young man in trauma, had been drinking,alcohol level >300. Multiple fractures. Initial lactate 10 then post fluid resus lactate 5.
a. 2nd lactate more important than first for prognosis b. initial lactate high due to alcohol c. ? d. The initial lactate result carries a mortality exceeding 20% e. ? |
A
CEACCP Phypers and Pierce 6 (3): 128. (2006). Lactate physiology in health and disease. A. Trueish. Whole body hypoxia occurring during cardiac arrest or severe hypovolaemia triggers anaerobic metabolism. Lactate concentrations directly reflect cellular hypoxia. Consequently, during in-hospital cardiac arrest and 1 h after return of spontaneous circulation, lactate concentrations are predictive of survival. B. True. Gluconeogenesis supplies NAD+ required to convert lactate to pyruvate. The supply of NAD+ is vulnerable to demands from other enzyme systems, such as alcohol dehydrogenase. This becomes significant when activated by ethanol intoxication. Apparently not significant enough to give a lactate of 10 according to other references C. – D. False. Blood lactate concentrations of >5mmol/L in patients with severe acidosis ph<7.35 or base deficit >6 carries a mortality of 80% E. – |
|
|
Patient has anterior cervical spine fusion. Most likely cause of hoarse voice
a. RLN injury b. Swelling c. ? d. ? e. ? |
B
CEACCP Hunningher and Calder 7 (3): 81. (2007). Cervical spine surgery. Some degree of airway obstruction is not uncommon after anterior cervical surgery. It is sometimes because of a haematoma, but in many cases it is because of tissue swelling. It usually presents within 6 h, but can occur later. Airway obstruction is particularly likely after combined anterior–posterior cervical surgery. There are some important diagnostic points: 1. Stridor is unusual—the obstruction is because of swollen tissue in the supra and peri-glottic regions. 2. The patients say they ‘can’t breathe’ and want to sit up. 3. Oximetry may register almost normal values until very late. 4. The presence of a drain in the neck does not prevent swelling |
|
|
A 6 month old baby is booked for an elective right inguinal hernia repair. An apropriate fasting time is
A 2 hours breast milk B 4 hours formula milk C 5 hours breast and formula milk D 6 hours solids E 8 hours solids, 4 hours all fluids |
D
RCH Fasting guidelines Children less than 6 months of age: • Please plan for the last breast feed to finish no later than 3 Hours before anaesthesia. • Please plan for a formula or cow's milk feed to finish no later than 4 Hours before anaesthesia. All other patients: • Please do not give milk drinks, food, lollies or chewing gum for 6 Hours before anaesthesia. • Please offer clear fluids up to 2 Hours before anaesthesia NOTE: this is different to the ANZCA day surgery guidelines: • limited solid food may be taken up to six hours prior to anaesthesia and clear fluids totalling not more than 200 mls per hour may be taken up to two hours prior to anaesthesia. • Children over six weeks of age, limited solid food and formula milk may be given up to six hours, breast milk may be given up to four hours and clear fluids up to two hours prior to anaesthesia. • For infants under six weeks, formula or breast milk may be given up to four hours and clear fluids up to two hours prior to anaesthesia. |
|
|
Arrest in a 10 year old. Has ventricular tachycardia after a near drowning accident. Patient is intubated and is being ventilated with 100% O2 and has IV access. A single DC monophasic shock of 60J has been given. The next step is to give
A adrenaline 10mcg/kg and DC shock 60J B adrenaline 10mcg/kg and DC shock 120J C amiodarone 5mg/kg D DC shock 60J E DC shock 120J |
E
ARC 2006 12.6 Paed Guidelines The recommended initial monophasic or biphasic shock treatment of VF or pulseless VT is a single shock of 2 joules per kilogram (J/kg) followed by 2 minutes of CPR and then by a monophasic or biphasic shock of 4J/kg 1,2,3 [Class A; LOE IV]. All subsequent shocks should be 4 J/kg 1 [Class A; LOE IV]. Current Guidelines say to go straight to 4J/kg however |
|
|
6 month old baby for VSD repair. Induced with 50% N2O, O2, sevoflurane 8%. While obtaining IV access, the patient desaturates to 85%. The manouevre to increase the O2 saturations is to
A give a fluid bolus B change from sevoflurane to isoflurane C institute CPAP D decrease the FiO2 E reduce the sevoflurane concentration |
E
C and D would potentially increase PVR and worsen shunt Not sure if a fluid bolus would improve situation with a VSD – but is 1st thing to do with a tet spell |
|
|
The active metabolite of ketamine is:
a. Hydroxyketamine b. Hydroxynorketamine c. Ketamine glucuronide d. Ketamine sulphonamide e. Norketamine |
E
Peck & Hill p112 Demethylated to active metabolite norketamine by P450 system. 30% as potent as ketamine. |
|
|
Antidepressants are not effective/recommended for
a. Chronic headache b. Chronic back pain c. Chronic pain post mastectomy d. Chronic pain post acute herpes zoster e. Trigeminal neuralgia |
B& E
Not reversal of previous conclusion - antidepressants no longer thought to help pain relief in low back pain |
|
|
NNT is the number of patient who need to be treated to prevent 1 additional bad outcome. The NNT is the reciprocal of the
A. absolute odds of a bad outcome B. absolute risk of a bad outcome C. absolute risk reduction in the bad outcome (due to the treatment) D. odds ratio of the bad outcome (due to the treatment) E. relative risk of the bad outcome (due to the treatment) |
C
|

