![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
69 Cards in this Set
- Front
- Back
|
8. Predisposing factors for the development of late-onset respiratory depression following spinal administration of opioids include
A. use of water soluble opioids B. concomitant use of ketorolac C. obesity D. hypothyroidism E. slow administration of the opioid |
A
|
|
|
"The most frequent and earliest sign of MH crisis is an unexplained, unexpected tachycardia together with an unexplained, unexpected rise (over minutes to hours) in EtCO2, the most sensitive indicator of potential MH... Tachycardia is seen in almost all patients as one of the early signs of malignant hyperthermia and may occur within 30 minutes of the induction of anaesthesia. Tachycardia probably results from an increase in catecholamine release and has been blunted experimentally with propranolol."
(Ali et al, Malignant Hyperthermia, in Best Practice & Research Clinical Anaesthesiology Vol. 17, No. 4, pp. 519–533, 2003) |
D
|
|
|
17. The carotid sinus derives its nerve supply from the
A. vagus nerve B. glossopharyngeal nerve C. ansa cervicalis (hypoglossi) D. middle cervical ganglion E. stellate ganglion |
B
Wikipedia: The carotid sinus baroreceptors are innervated by the sinus nerve of Hering, which is a branch of IX (glossopharyngeal nerve). The glossopharyngeal nerve synapses in the nucleus tractus solitarius (NTS) located in the medulla of the brainstem. The NTS indirectly modulates the activity of sympathetic and parasympathetic (vagal) neurons in the medulla and pons through the hypothalamus. These neurons then regulate the autonomic control of the heart and blood vessels. The aortic arch baroreceptors are innervated by the aortic nerve (Nerve of Cyon), which combines with CN X (vagus nerve) and travels to the NTS. carotid sinus : baroreceptor at the origin of the ICA; rich nerve supply from IX (Glossopharyngeal), stimulation à fall in BP carotid body : chemoreceptor : small, oval, reddish brown structure deep to bifurcation of CCA, also innervated by IX (Glossopharyngeal) |
|
|
24. Sensation from the lobule of the external ear is mediated mostly by
A. the auriculo-temporal nerve B. the great auricular nerve C. the lesser occipital nerve D. the greater occipital nerve E. none of the above |
B
From Anatomy for Anaesthetists: "The great auricular nerve (C2, 3) is the largest cutaneous branch of the cervical plexus. It hooks around the mid-point of the posterior border of sternocleidomastoid, then passes across it in the direction of the angle of the mandible. On this muscle it breaks up into three terminal branches. 1. Auricular - supplying the lower two-thirds of the medial aspect of the external ear and the lateral surface of the lobule. 2. Mastoid - to the skin over the mastoid process. 3. Facial - to the skin over the masseter and the parotid gland." |
|
|
26. When pulmonary oedema is due to raised capillary hydrostatic pressure, the most reliable radiological evidence of this aetiology is derived from
A. heart size B. mediastinal width C. upper lobe vascular markings D. the presence of basal effusions E. oedema migration with postural change |
C
Heart size relates to CCF. Can be other sources of raised hydrostatic pressure eg. pulm fibrosis. Mediastinal width relates to mediastinal pathology, not directly related to raised hydrostatic pressure. Basal effusions are only seen late - when >200-250mL. There is no description of change of edema with postural change in texts. |
|
|
27. In a patient with aortic stenosis,
A. aortic regurgitation is rarely seen B. loss of sinus rhythm is poorly tolerated C. presentation is usually with a cerebrovascular accident D. the characteristic compensation of the left ventricle is dilatation E. the most common aetiology is rheumatic calcification |
B
|
|
|
28. The muscles of the larynx which separate the vocal cords are the
A. thyro-arytenoids B. lateral crico-arytenoids C. oblique arytenoids D. posterior crico-arytenoids E. thyro-arytenoids |
D
From Anatomy for Anaesthetists: "The posterior cricoarytenoid muscle arises from the posterior surface of the lamina of the cricoid and is inserted into the posterior aspect of the muscular process of the arytenoid. It abducts the cord by external rotation of the arytenoid and thus opens the glottis; it is the only muscle to do so." |
|
|
29. The innervation of the human larynx is such that
A. the internal laryngeal branch of the superior laryngeal branch of the vagus supplies the lingual surface of the epiglottis B. in the cadaveric position the cords are fully abducted C. the recurrent laryngeal nerve supplies all the intrinsic muscles of the larynx D. the glossopharyngeal nerves are sensory to the laryngeal mucous membrane above the level of the vocal cords E. cord paralysis can be produced by a distended endotracheal cuff in the larynx compressing a branch of the recurrent laryngeal nerve against the thyroid cartilage |
E
Anaesth Intensive Care. 2004 Jun;32(3):417-8.Links Bilateral adductor vocal cord paresis following endotracheal intubation for general anaesthesia. Recurrent laryngeal nerve palsy is a rare complication of endotracheal intubation. We report a case of bilateral vocal cord palsy following endotracheal intubation for general anaesthesia. The clinical picture was of hoarseness and aspiration suggesting partial paresis, as complete bilateral recurrent laryngeal nerve palsy usually causes acute airway obstruction due to unopposed vocal cord adduction. Compression of the anterior branch of the recurrent laryngeal nerve between the cuff of the endotracheal tube and the posterior part of the thyroid cartilage was the likely mechanism. Ensuring that the cuff of the endotracheal tube is distal to the cricoid cartilage and that the pressure in the cuff is kept to the minimum required to prevent a gas leak should prevent this complication. |
|
|
35. During anaesthesia using IPPV in the lateral position with the left side uppermost, the fractional blood flow to the left lung is
A. 20% B. 35% C. 45% D. 55% E. 60% |
B
Miller: - Distribution of blood flow is L 45%; R 55% (erect / supine). - Less 10% whichever side is up (eg. L side up means 45-10% = 35%). - No difference between awake or asleep; open or closed chest. |
|
|
39. The proportion of adult patients with a probe-patent foramen ovale is
A. 0-10% B. 10-20% C. 20-35% D. 35-50% E. greater than 50% |
C
Stoelting: " Anatomic closure of the foramen ovale occurs between 3 months and 1 year of age, although 20% to 30% of adults have probe-patent foramen ovales." |
|
|
40. The difference in duration of action of bupivacaine and lignocaine is most marked with
A. infiltration anaesthesia B. carbonated solutions C. peripheral nerve block D. extradural anaesthesia E. solutions containing 1 in 200,000 adrenaline |
C
See Stoelting chapter on local anaesthetics - table clearly depicts longest difference between lignocaine and bupivacaine for peripheral nerve blocks |
|
|
41. The sciatic nerve supplies the following muscles EXCEPT
A. biceps femoris B. semitendinosus C. semimembranosus D. gluteus maximus E. adductor magnus |

D
From Anatomy for anaesthetists: |
|
|
48. Typical physiological changes in pregnancy at term, compared to the non-pregnant state include a twenty percent
A. increase in alveolar ventilation B. increase in tidal volume C. increase in vital capacity D. reduction in arterial pH E. reduction in functional residual capacity |
E
In pregnancy: - VT increases 40% - FRC decreases 20% - RR increases 15% - MV increases 60% - Due to diaphragm cephalad incursion + increased chest diameters - PaCO2 approx 32 (i.e. resp alkalosis), but pH unchanged via renal compensation (i.e. HCO3 approx 22 vs 24 normally) |
|
|
49. The percentage of diabetic patients with autonomic neuropathy is reported to be
A. <5% B. 10 - 20 % C. 20 - 40 % D. 60 - 80% E. >80% |
C
BJA. McAnulty et al. 85 (1): 80. 2000: “Detectable in up to 40% of type 1, and 17% of type 2 diabetics. Only a small proportion of these will be symptomatic (gastroparesis, postural hypotension, gustatory sweating, diabetic diarohea, and bladder paresis)” Oxford Handbook of Anaesthesia (1st ed, p72) says: "present in 50% of diabetics" |
|
|
90. Successful regional anaesthesia for femoral hernia repair requires the following nerves to be blocked EXCEPT the
A. ilioinguinal B. iliohypogastric C. cutaneous branches of intercostal nerves from T11 and T12 D. femoral E. genitofemoral |
D
Field block for an inguinal hernia repair. The nerves concerned include: • Subcostal n • Iliohypogastric n • Ilioinguinal n • Genitofemoral n (may supply skin of the medial part of the groin) Principles of Regional Anaesthesia, Wildsmith et al (I would assume the femoral sheath has a similar supply to the inguinal canal being adjacent to each other.) |
|
|
93. Physiological consequences of obstructive sleep apnoea usually include each of the following EXCEPT
A. stimulation of erythropoiesis B. pulmonary vasoconstriction C. tachycardia followed by bradycardia D. systemic vasoconstriction E. loss of deep sleep |
C
It's bradycardia followed by tachycardia. • A – False. (I.e. a true statement.) • B - False. (I.e. a true statement.) • C – True. (I.e. a false statement.) Bradycardia from hypoxia, then tachycardia with resumption of respiration / wakening. • D - False. (I.e. a true statement.) Hypoxia leads to increased sympathetics, which leads to systemic vasoconstriction. • E - False. (I.e. a true statement.) |
|
|
94. In the Neuroleptic Malignant Syndrome
A. there is a familial incidence B. non-depolarising muscle relaxants decrease the muscle rigidity C. creatinine kinase levels are elevated following an episode D. there is an association with malignant hyperpyrexia E. hyperthermia does not always occur |
B
"Considering all the disadvantages of dantrolene (vide infra), using nondepolarizing neuromuscular blocking agents (eg, pancuronium, other newer agents) is reasonable, along with such sedatives as benzodiazepines, to achieve rapid, predictable, and effective control of rigidity and hyperthermia." Emedicine |
|
|
97. Epidural sensory blockade to T2 in healthy adults is associated with each of the following EXCEPT
A. bradycardia B. decreased circulating catecholamines C. dyspnoea D. vasodilatation E. raised PaCO2 |
E
Though C could also be correct The cardiac sympathetic fibers arise from T1 to T4 In addition to the cardiac effects, a high level of sympathetic blockade causes: • Increased central venous pressure without an increase in stroke volume • Compensatory vasoconstriction in the head, neck, and upper limbs • Splanchnic nerve blockade with reduction in medullary secretion of catecholamines • Blockade of vasoconstrictive effect on the capacitance vessels of the lower limbs Lung volumes (tidal volume, vital capacity), resting minute ventilation, and dead space are basically unchanged even with a high thoracic epidural anesthesia. Even with abdominal or intercostal muscle paralysis by a high thoracic block, major alteration in pulmonary function is not seen. |
|
|
98. When providing general anaesthesia to a patient with a history of asthma
A. thiopentone should not be used as it may cause bronchospasm B. intravenous and topical tracheal lignocaine are equally effective in preventing bronchial hyperreactivity C. ketamine provides little benefit in a patient with active wheezing D. induction with propofol is effective in reducing the incidence of wheezing following intubation E. isoflurane is as effective a bronchodilator as halothane when given in MAC equivalent doses |
D
|
|
|
99. Common complications of spinal cord injury include each of the following EXCEPT
A. deep vein thrombosis B. diarrhoea C. heterotopic calcification D. pressure sores E. urinary tract infection |
B
o A. Correct – DVT prophylaxis used acutely "The risk of deep vein thrombosi formationis greatky increased in the early stages. Untreated, 80-85% of patients will develop a deep vein thrombosis." o B. Incorrect \True "Acute gastroparesis and ileus is common immediately after spinal cord injury and caution needs to be applied with the use of oral fluids in the early stage." o C. Correct "Para-articular heterotopic ossification occurs in 20% of cord-injured patients. This is characterised by bone deposition around large joints and is of unknown cause." o D. Correct "Decubitus ulcers occur in up to 60% of patients with cervical lesions as a result of immobility, lack of sensation over pressure areas, altered regulation of skin blood flow, muscle atrophy and psychological factors." o E. Correct "Urinary tract infection is common as a result of high residual volumes and the use of urethral catheters." Reference: P. R. Hambly & B. Martin. Anaesthesia for chronic spinal cord lesions. Anaesthesia 2002 Vol 53(3) p.273-289 |
|
|
101. Of the options below, the best anaesthetic method for ophthalmic examination under anaesthesia in a co-operative mentally retarded adult (without aspiration risk) is intravenous induction and
A. intermittent positive pressure ventilation via endotracheal tube B. intermittent positive pressure ventilation via laryngeal mask airway C. spontaneous ventilation with inhalational agents via facemask D. spontaneous ventilation with inhalational agents via laryngeal mask airway E. ketamine and spontaneous ventilation via cut-down Hudson mask |
B
B to control CO2 and reduce IOP C and D both seem reasonable though I guess From CEACCP: "Spontaneous ventilation via a facemask will frequently suffice for simple eye examinations, although it is often more convenient to utilize a laryngeal mask airway to allow the ophthalmologist unrestricted access to the eyes. Spontaneous ventilation using a laryngeal mask airway is also satisfactory for the shorter surgical procedures where a sterile operating field is not required (e.g. laser surgery), and in most of the extra-ocular cases in older children. For intraocular procedures, the surgeon will require a still, ‘quiet’ eye and this is most satisfactorily achieved using paralysis and controlled ventilation. A secure airway is essential because of the inaccessibility of the airway when the face is covered with sterile drapes. A preformed RAE tracheal tube is generally used but this can pose a problem in neonates as the fixed length of the endotracheal portion of these tubes is frequently too long, potentially resulting in endobronchial intubation. While it is possible to pack out these tubes at the mouth to prevent this, it is more convenient to use a reinforced, flexible tracheal tube in infants below 6 months; this results in a secure airway that does not conflict with the surgical field” |
|
|
103. Pneumonia in children
A. if bacterial is commonly associated with a pleural effusion B. is often caused by Mycoplasma Pneumoniae in infants C. is rarely caused by Chlamydia Trachomatis in neonates D. is rarely fatal in developed countries E. often presents as lethargy without fever or cough |
D
• A - ? False. From Pediatrics in Review. 2002;23:417-426. Pleural Effusions in the Pediatric Population: "Pleural effusions (liquid in the pleural space), which occur less frequently in children than in adults, can be caused by a variety of infectious and noninfectious diseases. Most of the information about pleural effusions is derived from adult studies. Causes of pleural effusions in children differ significantly from those in adults. Among adults, the most frequent cause is congestive heart failure (transudate), and bacterial pneumonia and malignancy are the most frequent causes of exudate. Pleural effusions in children most commonly are infectious (50% to 70% parapneumonic effusion); congestive heart failure is a less frequent cause (5% to 15%), and malignancy is a rare cause. Parapneumonic effusion is defined as fluid in the pleural space in the presence of pneumonia, lung abscess, or bronchiectasis. Nontuberculous bacterial pneumonia constitutes the most frequent origin of pleural effusion in children. Establishing a specific causative agent depends on the patient’s age, underlying disease, standard of laboratory culture method, and initiation of antibiotic therapy. Staphylococcus aureus is the single most common pathogen causing empyema (29% to 35% of cases), especially among infants younger than 2 years of age. Streptococcus pneumoniae is the cause in up to 25% of cases of empyema." but from Emedicine: "In a prospective multicenter study of 154 hospitalized children with acute community-acquired pneumonia in whom a comprehensive search for etiology was sought, a pathogen was identified in 79% of children. Bacteria accounted for 60%, of which 73% were due to Streptococcus pneumoniae; Mycoplasma pneumoniae and Chlamydia pneumoniae were detected in 14% and 9%, respectively. Viruses were documented in 45% of children. Notably, 23% of the children had concurrent acute viral and bacterial disease. In the study, preschool-aged children had as many episodes of atypical bacterial lower respiratory infections as older children. Multivariable analyses revealed that high temperature (38.4°C) within 72 hours after admission and the presence of pleural effusion were significantly associated with bacterial pneumonia." • B - False. In > 6 y/o. • C - False. 10-20% from colonised mothers. • D - True in the developed world. Pediatrics in Review. 2002;23:132-140. Pneumonia: "Worldwide, more than 2 million children die of pneumonia annually. However, mortality is extremely rare in the United States and other parts of the developed world." From Emedicine: "According to the WHOs Global Burden of Disease 2000 Project, lower respiratory infections were the second leading cause of death in children younger than 5 years (about 2.1 million [19.6%]). Most children are treated as outpatients and fully recover. However, in young infants and immunocompromised individuals, mortality is much higher." • E - False. |
|
|
104. Following a retrobulbar block of the eye which of the following features would suggest brainstem spread of the local anaesthetic?
A. an atonic pupil B. blindness in the blocked eye C. blindness in the contralateral eye D. difficulty in swallowing E. diplopia |
D
Clin Anaes p. 978: Brainstem anaes: violent shivering, CL amaurosis, eventual LOC, apnoea, hemiplegia/paraplegia, quadriplegia, hyper-reflexia. BLock of CNs 8-12 - deafness, vertigo, vagolysis, dysphagia, aphasia, loss of neck m power. Blindness is not from brainstem spread, but rather a sign of spread back to optic chiasm |
|
|
105. Adults with chronic renal insufficiency can maintain a normal
plasma potassium concentration via tubular secretion until glomerular filtration rate falls below A. 100 ml.hour-1 B. 80 ml. hour-1 C. 50 ml. hour-1 D. 20 ml. hour-1 E. 8 ml.hour-1 |
E
Correct if ml/min 'Normokalemia can be maintained in patients who consume normal quantities of potassium until GFR decreases to less than 10 mL/min;' |
|
|
107. In patients with advanced liver disease who receive muscle relaxants
A. decreased plasma clearance of vecuronium and rocuronium leading to prolonged blockade is a consistent feature B. duration of action of mivacurium is NOT affected C. initial doses should be reduced as volume of distribution is decreased D. plasma clearance of atracurium and cisatracurium is increased E. when the desired level of block is achieved with the initial dose, subsequent recovery is comparable to patients without liver disease |
D
Based on Stoelting: Anesthesia & Coexisting Disease 4th Ed pg 314-5 Sux & mivacurium are acceptable, although severe liver disease may decrease plasma cholinesterase activity and prolong action (B is out) Inc VD that accompanies cirrhosis may result in the need for larger initial doses of NDMR to produce the required plasma conc, but the resulting NMB may be prolonged if drugs depend on hepatic clearance mechansims (C & E are out) Hepatic dysfunction does not alter the elimination half-time of atracurium and the same is presumed to be true for cisatracurium (D is out) BUT clearance of atrac and cisarac may be increased because of larger Vd |
|
|
108. Increased bleeding risk is associated with all of the following EXCEPT
A. aspirin B. hypothermia C. lupus anticoagulant D. renal failure E. von Willebrand's disease |
C
lupus antiphospholipid → hypercoaguable, therefore an increased clotting risk, not an increased bleeding risk |
|
|
109. Each of the following statements regarding DVIR pacing is true EXCEPT
A. atrial sensing inhibits atrial pacing B. pacing will usually provide AV (atrioventricular) synchrony C. the rate of pacing can be altered by patient activity D. ventricular sensing inhibits atrial pacing E. ventricular sensing inhibits ventricular pacing |
A
DVIR pacemaker • First letter = Paced • Second letter = Sensed • Third letter = Response • Fourth letter = Rate response/programmability |
|
|
110. Following acute subarachnoid haemorrhage, the use of anti¬fibrinolytic agents is associated with decreased
A. incidence of hydrocephalus B. incidence of rebleeding C. incidence of pulmonary embolus D. mortality from all causes E. mortality from ischaemic neurological events |
B
The Lancet Volume 369, Issue 9558, 27 January 2007-2, Pages 306-318 Seminar-Subarachnoid haemorrhage ‘Antifibrinolytic drugs prevent rebleeding after aneurysmal rupture, but because they increase the risk of cerebral ischaemia, they have no useful effect on overall outcome’ |
|
|
111. The patient plate of some diathermy units has two separate areas and two wires to allow for
A. a back-up if one area fails B. bipolar cautery C. capacitive coupling to the patient D. coagulation and cutting currents E. return electrode monitoring |
E
REM™ contact quality monitoring was developed to protect patients from burns due to inadequate contact of the return electrode. Pad site burns are caused by decreased contact area at the return electrode site. REM™-equipped generators actively monitor the amount of impedance at the patient/pad interface because there is a direct relationship between this impedance and the contact area. The system is designed to deactivate the generator before an injury can occur, if it detects a dangerously high level of impedance at the patient/pad interface. In order to work properly, REM™-equipped generators must use a patient return electrode that is compatible, as depicted in the photo at right. Such an electrode can be identified by its “split” appearance – that is, it has two separate areas – and a special plug with a center pin |
|
|
112. Each of the following findings is consistent with brain death EXCEPT
A. absence of diabetes insipidus i.e. continued vasopressin secretion B. Babinski's reflex C. focal EEG (electroencephalogram) activity D. limb movement in response to touch E. nystagmus on injection of cold water into the ear canal |
E
• A - False. (I.e. consistent with brain death). Absence of diabetes insipidus is consistent with a diagnosis of brain death. • B - False. (I.e. consistent with brain death). Presence of Babinski reflex is compatible with a diagnosis of brain death. • C - False. (I.e. consistent with brain death). EEG not part of the criteria in Australia. Has been used in the US. • D - False. (I.e. consistent with brain death). See IC24b - 2 and 4. • E - True. (I.e. INconsistent with brain death). An intact vestibulo-ocular reflex excludes brain death. ANZICS Statement on Death and Organ Donation Brain death is determined by: clinical testing if preconditions are met; or imaging that demonstrates the absence of intracranial blood flow. The overall function of the whole brain is assessed. However, no clinical or imaging tests can establish that every brain cell has died. PRECONDITIONS As well as the evidence of sufficient intracranial pathology, as outlined in Section 2.1, all the following preconditions must be met if brain death is to be determined by clinical examination: • normothermia (temperature > 35 C); • normotension (as a guide, systolic blood pressure > 90 mmHg, mean arterial pressure (MAP) > 60 mmHg in an adult); • exclusion of effects of sedative drugs (self-administered or otherwise) the time taken for plasma concentrations of sedative drugs to fall below levels with clinically significant effects depends on the dose and pharmacokinetics of drugs used, and on hepatic and renal function. If there is any doubt about the persisting effects of opioids or benzodiazepines, an appropriate drug antagonist should be administered; • absence of severe electrolyte, metabolic or endocrine disturbances these include: marked derangements in plasma concentrations of glucose, sodium, phosphate or magnesium; liver and renal dysfunction; and severe endocrine dysfunction; • intact neuromuscular function if neuromuscular-blocking drugs have been administered, a peripheral nerve stimulator or other recognised method (e.g. electromyography) should always be used to confirm that neuromuscular conduction is normal; • ability to adequately examine the brain-stem reflexes it must be possible to examine at least one ear and one eye; and • ability to perform apnoea testing this may be precluded by severe hypoxic respiratory failure or a high cervical spinal cord injury. The following need to be established to determine brain death by clinical testing: • absence of responsiveness; and • absence of brain-stem reflexes; and • presence of apnoea. The following are incompatible with the presence of brain death: • decerebrate or decorticate posturing; • true extensor or flexor motor responses to painful stimuli; and • seizures. |
|
|
113. The incidence of an intra-cranial aneurysm is increased by each of the following EXCEPT
A. Ehlers Danlos disease B. hypertension C. neurofibromatosis D. positive family history of intra-cranial aneurysms E. type 2 diabetes mellitus |
E
Emedicine: The development of cerebral aneurysms remains a controversial topic. A multifactorial etiology is most likely, reflecting the interaction of environmental factors, such as atherosclerosis or hypertension, and a congenital predisposition associated with various vascular abnormalities. Abnormalities of the internal elastic lamina may be congenital or degenerative. Multiple conditions have been associated with cerebral aneurysms; they include the following: • Autosomal dominant inherited polycystic kidney disease • Fibromuscular dysplasia • Arteriovenous malformations • Osler-Weber-Rendu syndrome • Coarctation of the aorta • Other vascular anomalies • Moyamoya syndrome • Marfan syndrome • Ehlers-Danlos syndrome, type IV • Other collagen type III disorders • Pseudoxanthoma elasticum • Alpha1-antitrypsin deficiency • Systemic lupus erythematosus • Sickle cell anemia • Bacterial endocarditis • Fungal infections • Neurofibromatosis type 1 • Tuberous sclerosis |
|
|
114. Early features of pulmonary hypertension include each of the following EXCEPT
A. a narrowly split second heart sound (S2) B. an early diastolic murmur C. decreased oxygen saturation D. dyspnoea on exertion E. hyperlucent lung periphery on chest Xray |
B
Screening, Early Detection, and Diagnosis of Pulmonary Arterial Hypertension: ACCP Evidence-Based Clinical Practice Guidelines Chest 2004;126;14S-34S Patients with PAH generally present with a spectrum of symptoms attributable to impaired oxygen transport and reduced cardiac output. Although PAH may be asymptomatic, particularly in its early stages, exertional dyspnea is the most frequent presenting symptom, and was present in 60% of patients in the National Institutes of Health (NIH) prospective cohort study of patients with PPH.8 Dyspnea is eventually present in virtually all patients as the disease progresses. Fatigue, weakness, or complaints of general exertion intolerance are also common complaints… …Signs of PH on physical examination are subtle and often overlooked. Although no rigorous analysis of the sensitivity and specificity of findings on physical examination has been performed, experience suggests that the likelihood of PAH is increased when certain findings are present. For example, an accentuated pulmonary component of the second heart sound audible at the apex is noted in >90% of patients with IPAH,8 reflecting increased force of pulmonary valve closure due to elevated pulmonary artery pressure. Other signs of increased pulmonary artery pressure include the following: (1) an early systolic ejection click due to sudden interruption of pulmonary valve opening, (2) a midsystolic ejection murmur caused by turbulent transvalvular pulmonary flow, (3) a palpable left parasternal lift produced by the impulse of the hypertrophied high-pressure right ventricle, (4) a right ventricular S4 gallop (audible in 38%),8 and (5) a prominent jugular “a” wave suggesting high right ventricular filling pressure. Physical signs of more advanced disease include the diastolic murmur of pulmonary regurgitation and the holosystolic murmur of TR, which is audible at the lower left sternal border and augmented with inspiration.8 TR can also be detected by an elevated jugular venous pressure with accentuated V waves, hepatojugular reflux and a pulsatile liver. A right ventricular S gallop (audible in 23%),8 marked distension of the jugular veins, pulsatile hepatomegaly, peripheral edema (32%),8 and ascites are indic- ative of right ventricular failure. Low BP, diminished pulse pressure, and cool extremities are ominous signs since they indicate the presence of a markedly reduced cardiac output and peripheral vasoconstriction… …General radiographic signs that can be taken as suggestive of PH are enlarged main and hilar pulmonary arterial shadows, with concomitant attenuation of peripheral pulmonary vascular markings (“pruning”). These features were present in most IPAH patients in the NIH Registry.8 However, the absence of pruning should not be interpreted as excluding IPAH” |
|
|
115. The effect of ketamine on the bispectral (BIS) index is
A. to lower the BIS reading B. to raise the BIS reading C. to initially raise, then lower the BIS reading D. to initially lower, then raise the BIS reading E. unpredictable |
B
We all know ketamine increases BIS, am tempted to pick E though as there is no stipulation on dose or whether patient has received other anaesthetic agents Hans et al. BJA 94 (3): 336. (2005) The hypnotic effect of ketamine is characterized by a dissociative mechanism, and this drug has been shown to increase u activity of the EEG.16 The BIS increase in response to ketamine is paradoxical in so far as the anaesthesia level is deepened by the administration of an additional anaesthetic agent. However, as discussed by Sleigh and Barnard, BIS must be considered to reflect cortical activity rather than the level of consciousness. Ketamine administered in patients anaesthetized with GABAergic agents that depress cortical activity, such as propofol or sevoflurane, induces a change in the EEG pattern towards higher frequencies and desynchronization. This modification is reflected in a BIS increase and has no relationship with anaesthetic depth |
|
|
116. Regarding left "Bronchocath" double lumen tubes
A. the bronchial cuff is inverted and the bronchial tip is non¬bevelled B. the length from the Y adapter to the tracheal opening varies with the size (35F to 41F) C. the outside diameter of the bronchial lumen in a 39F size is significantly larger than in a 37F size D. there is a black ring below the tracheal opening to aid fibre¬optic positioning E. the recommended volume for the bronchial cuff in a 41F tube is greater than 2.5 ml |

D
• A - False. "In 1994, the left Bronchocath tube was redesigned: the bronchial curve was made tighter, an inverted cuff was placed closer to the tip of the bronchial lumen, and the bevel of the bronchial lumen tip was eliminated. The non-beveled tip made inserting the tube through the glottic opening difficult, despite adequate laryngoscopic views. In 2001, Mallinckrodt reintroduced a beveled edge on the tip of the tube."One-Lung Anaesthesia: Making it work. Jerome Klafta • B - False. One-Lung Anaesthesia: Making it work. Jerome Klafta • C - False. Dimensions of Double-Lumen Tracheobronchial Tubes. Russell WJ, et al. Anaesth Intensive Care 2003; 31:50-53: . • D - True. New Landmarks improve the positioning of the left BronchoCath DLT – comparison with the classic technique. CAN J ANESTH 2001/48:8, pp. 790-794: "However, through the left bronchial lumen, and by transparency across the wall of the tube, the position of the tube is adjusted so that the carina is midway between the black radiopaque line and the top of the bronchial cuff (Figures 2D and 3)." • E - False. The resting Volume and Compliance characteristics of the Bronchial Cuff of Left Polyvinyl Chloride Double lumen Endobronchial Tubes. Anesth Analg 1993;77:1222-6. "Because the resting volume of the bronchial cuff of PVC DLTs varies widely between different tube sizes and brands, the users of these tubes should be aware of the specific resting volume of the bronchial cuff of the tube they choose. If the bronchial cuff of a properly placed DLT requires more than the natural resting volume to create a seal it is likely to be the wrong size for that patient." |
|
|
117. The first heart sound on auscultation is
A. characteristically quiet in mitral stenosis B. due equally to mitral and tricuspid valve closure C. louder than usual with a premature beat D. loudest at the left sternal edge E. unchanged in mitral regurgitation |
C
Talley & O’Connor a. false, loud S1 in mitral senosis b. false, higher left sided pressures thus mitral valve contributes more to S1 c. true, the early arrival of ventricular contraction before ventricular filling tapers off means the valve is widely open and will make a louder sound upon closure with the VEB d. false, 5th I/C space, MCL e. false, soft or absent |
|
|
118. The median body mass index (BMI) for a Caucasian boy (in a developed country) is
A. 16 kg.m-2 B. 22 kg.m-2 C. 25 kg.m-2 D. 28 kg.m-2 E. 33 kg.m-2 |
A
|
|
|
119. A 13-year-old boy with Duchenne's muscular dystrophy
A. is at increased risk of malignant hyperthermia B. is likely to have significant scoliosis C. is more likely to be cachectic than obese D. is unlikely to have cardiac involvement E. may develop rhabdomyolysis when non-depolarising muscle relaxants are used |
B
A – False. used to be the thinking in the past, now this MH-like reaction which DMD patients can get when exposed to inhalational agents is termed anaesthesia-induced rhabdomyolysis B – True. “respiratory function is compromised both by the progression of the disease and collapse of the spine, due to muscular weakness, resulting in scoliosis that adds to the pulmonary restrictive defecit” C – False. Pediatric Anesthesia, Volume 18, Issue 2 (p 100-106): “Obesity is common in older boys and they frequently have hypertrophy of the tongue making intubation more difficult.” DMD is pseudohypertrophic disease – therefore patients can appear quite muscular and stout. D – False. Pediatric Anesthesia, Volume 18, Issue 2 (p 100-106): “Dilated cardiomyopathy occurs in over 50% of patients by 15 years of age “ E – False. Applies to depolarising muscle relaxants. |
|
|
120. The most common coagulopathy in trauma patients is
A. clotting factor inhibition and depletion B. disseminated intravascular coagulation C. citrate toxicity D. hypofibrinogenaemia E. thrombocytopaenia |
E
Though my initial thoughts were A Updates in the management of severe coagulopathy in trauma patients Intensive Care Med (2002) 28:S241–S247 "Dilutional thrombocytopenia represents the most common of the coagulation abnormalities occurring in trauma patients, and is particularly common in patients who receive transfusion volumes in excess of 1.5 times their blood volume. After replacement of one blood volume, only about 35–40% of platelets remain in circulation. |
|
|
121. The following are correct statements regarding glycoprotein Ith/IlIa antagonists EXCEPT
A. platelet function persists even at 48 hours after cessation of drug B. their effects may be monitored by use of a platelet turbidometry aggregometer C. they are known to cause severe thrombocytopaenia in some patients D. they are used to treat acute coronary syndromes E. they block fibrinogen binding to platelet glycoprotein Hip/ Ina receptors |
A
• A - False. With regard to abciximab: "ReoPro remains in the circulation for 15 days or more in a platelet bound state, although platelet function recovers over the course of 48 hours." AND "As patients receiving abciximab experience platelet dysfunction for 12–24 h after termination of the infusion, it would seem prudent that surgery should be delayed for at least 12–24 h after abciximab if the patient’s cardiac status permits. Surgery should be delayed for 4–6 h to reduce the risk for increased bleeding in patients who have received eptifibatide or tirofiban." • B - True. "The pharmacological effects of GP IIb/IIIa antagonists can be assessed in a number of different ways. The most widely used method is turbidometric aggregometry..." Scarborough et al., GP IIB/IIIa Antagonists. Circulation 1999;100;437-444. • C - True. "In 0.1–0.5% of patients, severe thrombocytopenia occurs after intravenous administration of glycoprotein IIb/IIIa inhibitors in the nonsurgical setting. Abciximab causes thrombocytopenia in 0.4–1.6% patients, and this can occur after a single dose. In trials with other glycoprotein IIb/IIIa antagonists, the incidence of thrombocytopenia is generally lower than 1%. Thrombocytopenia usually occurs within hours of exposure and resolves on discontinuation of the drug, rarely requiring platelet transfusion unless accompanied by active bleeding." Anesthesiology 2002; 96:1237–49 (P. Kam) • D - True. "The efficacy of the glycoprotein IIb/IIIa antagonists in the treatment of acute coronary syndromes (unstable angina and non–Q wave MI), MI, and percutaneous coronary interventions has been demonstrated in several multicenter trials." Anesthesiology 2002; 96:1237–49 (P. Kam) • E - True. "Eptifibatide (a smaller molecule compared with abciximab) binds to the glycoprotein IIb/IIIa receptor between the IIb and IIIa arms of the extracellular parts of the receptor and prevents binding of fibrinogen." AND "Tirofiban occupies a binding pocket on the glycoprotein IIb/IIIa receptor and competitively inhibits platelet aggregation mediated by fibrinogen and von Willebrand factor." Anesthesiology 2002; 96:1237–49 (P. Kam) |
|
|
122. The most correct statement regarding the Child-Pugh score for liver disease is that
A. a high-risk score is not possible with normal amino-transferase levels B. a high-risk score is possible without encephalopathy C. a prothrombin time greater than 10 seconds above normal confers extra points to the raw score D. it has not been validated for non-shunt and non-transplant laparotomies E. it was originally developed for patients undergoing hepatic transplantation |
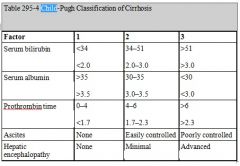
B
• A - False. Can have a high-risk score with normal aminotransferase levels - does not enter into the calculation. • B - True. A high risk score up to 12/15 is possible without encephalopathy. • C - False. Highest score with prothrombin time > 6 seconds (INR > 2.3) • D - False. From CEACCP Volume 9 Number 1 2009, Anaesthesia for hepatic resection surgery: "The Child-Pugh clinical scoring system has been used as a reliable, validated prognostic tool for patients with chronic liver disease undergoing general or porto-caval shunt surgery and has gained widespread use in hepato-biliary surgery." and from Emedicine quote below: "The CTP score was first developed to predict mortality after portocaval shunt surgery, but it has since been used to predict perioperative morbidity and mortality rates for patients undergoing hepatic and nonhepatic intra-abdominal surgeries." • E - False. From quote below: "This scoring system was initially devised to stratify patients into risk groups prior to undergoing portal decompressive surgery" From Harrison's: "A reliable staging system is the modified Child-Pugh classification with a scoring system of 5–15: scores of 5 and 6 being Child-Pugh class A (consistent with "compensated cirrhosis"), scores of 7–9 indicating class B, and 10–15 class C. This scoring system was initially devised to stratify patients into risk groups prior to undergoing portal decompressive surgery. The Child-Pugh score is a reasonably reliable predictor of survival in many liver diseases and predicts the likelihood of major complications of cirrhosis such as bleeding from varices and spontaneous bacterial peritonitis. It was used to assess prognosis in cirrhosis and to provide the standard criteria for listing for liver transplantation (Child-Pugh class B). Recently the Child-Pugh system has been replaced by the model for end-stage liver disease (MELD) score for assessing the need for liver transplantation. The MELD score is a prospectively derived scoring system designed to predict prognosis of patients with liver disease and portal hypertension. It is calculated using three noninvasive variables—the prothrombin time expressed as international normalized ratio (INR), serum bilirubin, and serum creatinine “ |
|
|
123. The incidence of major focal neurological deficits after coronary artery bypass grafting (CABG) is
A. less than 1% B. 3% C. 6% D. 9% E. over 12% |
B
Cardiopulmonary Bypass Management and Neurologic Outcomes: An Evidence-Based Appraisal of Current Practices - Anesth Analg 2006;103:21–37 NEUROLOGIC COMPLICATIONS: MANIFESTATIONS AND MECHANISMS: Brain injury from cardiac surgery is manifest as a spectrum of disorders, including stroke, encephalopathy, and cognitive dysfunction. Stroke is the most obvious clinical manifestation, occurring in 1% to 3% of patients in most series. |
|
|
124. The target serum magnesium level in a patient with pre-eclampsia receiving a magnesium infusion is
A. 1 - 2 mmo1.1-1 B. 2 - 3.5 mmo1.1-1 C. 3 - 6 mmo1.1-1 D. 4 - 6 mmo1.1-1 E. 5 - 8 mmo1.1-1 |
B
|
|
|
125. Amniotic fluid embolism
A. can be associated with a mortality rate of 80% B. has an incidence of 1 in 2000 pregnancies C. is an uncommon cause of peripartum death D. is associated with a small chance of complications in survivors E. only presents during labour or caesarean section |
A
A. True - mortality quoted 20-80%. Oxford Handbook "Up to 80%" mortality B. False - incidence 1:2500 births C. ?False - Uncommon event. One of leading causes (~20%) of direct maternal deaths in Australia, but direct maternal death accounts for only ~1/3 of overall maternal mortality D. False - 50% die in first hour. Hypotension in 100%, foetal distress in 100%, acute hypoxia in >90%, coagulopathy/DIC in 80%, maternal death in 60%, seizures in 50%, >50% residual neurological deficit in 50% of surviving mothers & foetuses. E. False - Occurs due to introduction of foetal Tx into maternal circ. during: • 1st trimester curettage abortion. • 2nd trimester abortion w/ saline, PG or urea. • Amniocentesis • Abdominal Trauma • 3rd trimester spontaneously • Labour • LUSCS Post partum |
|
|
126. In postoperative pain management
A. COX-2 (cyclo-oxygenase-2) specific inhibitors are associated with similar effects on platelet function as other NSAIDs (non-steroidal ant-inflammatory drugs) B. COX-2 specific inhibitors are associated with similar effects on renal function and blood pressure as other NSAIDs C. NSAIDs should never be used in patients on ACE (angiotensin converting enzyme) inhibitors D. tramadol has little effect on post-operative shivering E. tramadol and morphine are associated with a similar degree of dizziness and drowsiness |
B
Quotes from ANZCA pain book: • A - False –Coxibs do not impair platelet function – this leads to reduced periop blood loss compared with NSAIDS. Platelets only produce COX-1, not COX-2. • B - True – Coxibs and non selective NSAIDS have similar effects on renal function. There was no difference in the incidence of CV complications with NSAIDs compared to Coxibs. However, there may bedifferences between different drugs in each class, although evidence is conflicting. • C - False – cautious use not absolutely contraindicated. Not mentioned in APMSE. • D - False – proven to be of benefit for prevention and treatment of post-op shivering. Sasada and Smith says for Tramadol "Tramadol appears to be effective in the treatment of post-operative shivering", • E - False – Tramadol is associated with a low incidence of cardiac depression and significantly less dizziness and drowsiness than morphine |
|
|
127. Patho-physiological features of patients with morbid obesity include
A. a blood volume:body weight ratio which is similar to that of patients with normal body weight B. an increased blood pressure and systemic vascular resistance compared to that of patients with normal body weight C. decreased gastric motility due to increased gastrin secretion D. cardiac pathology resulting from excess body mass and increased metabolic demand E. cardiac pathology resulting mainly from fatty infiltration or fatty change of the heart |
D
• A - False. There is increased blood volume, but not same ratio, maybe as low as 47ml/kg • B – False. Insulin resistance may be factor in enhanced pressor response to NA and Angiotensin II. Increased CO offsets increase in MAP to DECREASE SVR!! Pediatric Cardiology 24 number 6, 2003 p.548-552 • C. Falseish - increased gastric motility is new thinking, and similar resistance between stomach and GOJ, despite higher volume, lower pH. It is commonly believed that the combination of increased IAP, high vol. & low pH of gastric contents, delayed gastric emptying and an increased incidence of hiatus hernia & GOR place the obese pt. at high risk of aspiration. Recently this has been challenged, however, and although obese individuals have a 75% greater gastric vol. the resistance gradient b/w stomach & gastrooesophageal jxn. is similar to that in non-obese patients and gastric emptying is actually faster in the obese (but because of larger gastric vol. the residual vol. is larger.) Despite conflicting evidence it is sensible to take precautions against acid aspiration and all morbidly obese patients should receive acid aspiration prophylaxis, regardless of Sx’s. ‘Obesity in anaesthesia & intensive care’ BJA 2000; 85(1):91-108. Gastric acidity, fluid volume and pressure are increased. Stoelting ‘Anesthesia & Coexisting Disease’ 2nd Ed, Pg. 544 • D - Trueish, probably best answer. However, cardiac pathology linked to many factors (e.g. atherosclerosis, increased afterload, pulmonary hypertension / cor-pulmonale and arrhythmias). On the other hand, metabolic demand seems particularly important since it causes LV hypertrophy which can lead to systolic and diastolic dysfunction. Also increases work of heart. • E. Falseish, does occur, but not main cause |
|
|
128. A patient with pulmonary hypertension secondary to lung disease presents for a laparotomy. Regarding this patient's anaesthetic management
A. an alpha-agonist is the inotrope of choice B. hypothermia is protective against rises in pulmonary artery pressure C. isoflurane will tend to decrease pulmonary artery pressure D. ketamine is an appropriate anaesthetic agent E. right heart failure is not a concern |
A
Isoflurane neither increases not decreases PVR |
|
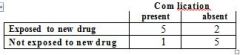
129. Six patients with an uncommon but newly described complication are selected, and 7 matching patients without this complication are selected, to determine their exposure to a new drug. The results are shown in this table.
Com lication present absent Exposed to new drug 5 2 Not exposed to new drug 1 5 The odds ratio of having the complication with exposure, compared with non-exposure, to the new drug is A. unable to be accurately calculated B. 0.08 C. 0.5 D. 2 E. 12.5 |
E
OR = ad/bc = 25/2 = 12.5 |
|
|
130. Following a cadaveric renal transplant under general anaesthesia, your patient's plasma K+ increases to 6.0 mmo1.1-1 in recovery after being 5.0 mmo1.1-1pre and intra-operatively. This patient requires
A. an intravenous infusion of CaC12 (10 mls over 20 minutes B. arterial blood gases to ascertain the acid/base status C. potassium exchange resins rectally D. sodium bicarbonate infusion (50-100 mEq over 5-10 minutes) E. urgent haemodialysis |
B
Discussion on wiki leans towards this answer. K of 6 not very exciting for a renal patient, just checking acid-base status seems reasonable. I’m not that fussed. No specific need for A. C would decrease K, though oral resonium also reasonable. D would also decrease K. E is not required |
|
|
131. Which of the following blood gases is consistent with an episode of malignant hyperthermia?
A. pH 7.13 pCO2 55 mmHg HCO3 18 mmo1.1-1 BE -9.1 mmo1.1-1 B. pH 7.24 pCO2 63 mmHg HCO3- 26 mmo1.1-1 BE 0 mmo1.1-1 C. pH 7.22 pCO2 30 mmHg HCO3- 12 mmo1.1-1 BE -13.8 mmo1.1-1 D. pH 7.46 pCO2 45 mmHg HCO3- 31 mmo1.1-1 BE 7.5 mmo1.11 E. pH 7.32 pCO2 44 mmHg HCO3- 22 mmo1.1-1 BE -3.1 mmo1.1-1 |
A
|
|
|
132. The median nerve
A. can be blocked at the elbow immediately lateral to the brachial artery B. can be blocked at the wrist between palmaris longus and flexor carpi ulnaris C. can be blocked at the wrist medial to flexor carpi ulnaris D. is formed from the lateral, medial, and posterior cords of the brachial plexus E. provides sensation to the radial half of the palm |
E
Almost REPEAT A. False. Lies immediately medial to brachial artery. B. False. Lies between FCR and PL C. False. Lies lateral to FCU D. False. The median nerve (C5–8, T1) carries fibres from all the roots of the brachial plexus; C5, 6 and 7 from the lateral head, which is derived from the lateral cord of the plexus, and C8 and TI from the medial head, derived from the medial cord. Ellis E. True. |
|
|
133. In its pure form, arnica (a herbal medicine), can cause post-operative
A. angina B. bleeding C. prolonged sedation D. oculogyric crises E. vomiting |
B
"Two sesquiterpene lactones of Arnica montana, helenalin and 11, 13-dihydrohelenal have been shown to inhibit collagen-induced platelet aggregation, thromboxane formation, and 5-hydroxytryptamine secretion." (Uptodate) |
|
|
134. A youth of 19 is brought to hospital after a boxing contest because of headache and vomiting. His initial computerized axial tomographic examination (CT scan) of the skull is normal. Two hours later he loses consciousness and is found to have dilatation of one pupil. He shows no response to painful stimuli. His blood pressure is 160/100 mmHg and his pulse rate 55 per minute. In consequence of his deteriorating condition the next step in management should be
A. urgent craniotomy B. repeat CT scan of the skull C. bilateral carotid angiography D. treatment of cerebral oedema E. transfer to an intensive therapy unit |
D
May need craniectomy not craniotomy B, C, E certainly wrong |
|
|
135. A patient needs to have intravenous access established. The best
recommendation for control of intravenous catheter related infection is A daily replacement of the intravenous fluid giving set if used for blood transfusion B. hand washing by the person inserting the catheter C. the application of antiseptic ointment to the cannulation site when dressing and fixing the cannula D. the use of an alcohol rather than aqueous iodine antiseptic skin preparation E. the use of the smallest suitable cannula |
B
http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5110a1.htm “Observe proper hand-hygiene procedures either by washing hands with conventional antiseptic-containing soap and water or with waterless alcohol-based gels or foams. Observe hand hygiene before and after palpating catheter insertion sites, as well as before and after inserting, replacing, accessing, repairing, or dressing an intravascular catheter. Palpation of the insertion site should not be performed after the application of antiseptic, unless aseptic technique is maintained (43,70,196--200). Category IA”-CDC Guidelines |
|
|
136. During surgery for tracheostomy insertion surgical diathermy is being used at the tracheal incision. You are ventilating with 100% oxygen. As the trachea is opened you notice a blue flame shooting up from the incision. Your first action should be to
A. disconnect the breathing circuit from the endotracheal tube B. douse the wound with saline C. insert a tracheostomy tube D. remove the endotracheal tube E. turn off oxygen and ventilate with air |
A
http://www.health.vic.gov.au/vccamm/downloads/fire.pdf 1. Extinguish the fire. 2. In the event of fire, immediately disconnect the patient from the anaesthetic machine, switch off the anaesthetic gas flow, disconnect the gas pipelines and ventilate with room air using a self-inflating bag. 3. Use an airway filter if there is smoke in the theatre. 4. Consider flushing saline down the endotracheal tube to extinguish any intraluminal fire. 5. Consider removing or changing the tube to minimise the inhalation of toxic products of combustion and spread of fire into the tracheo-bronchial tree. However, changing the tube may be more risky than leaving it in if the patient was previously difficult to intubate or the airway has become oedematous. If tube removal deemed necessary use ventilating exchange bougie. |
|
|
137. When considering perioperative hypothermia
A. the brain and major abdominal organs generate more metabolic heat than resting muscle B. the pattern of intra-operative hypothermia has 2 phases C. induction of general anaesthesia leads to a core temperature drop of < 0.5°C within the first hour D. the extent of redistribution hypothermia is primarily related to patient initial body heat content E. conduction contributes most to heat loss during the linear phase of hypothermia |
A
A – true. direct quote from Sessler et al. Anesthesiology 2000 Vol 92: p 578 B – false. 3 phases. C – false. drops 1 – 1.5 degrees Celcius D – false. extent of redistribution depends on temperature gradient between core and periphery E – false. radiation responsible for majority of heat loss |
|
|
138. Features of the transurethral resection of the prostate (TURP) syndrome include all of the following EXCEPT
A. agitation B. angina C. bradycardia D. nausea E. tinnitus |
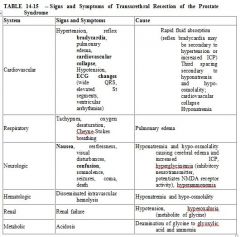
E
Tinnitus is not a feature. Anaesthesia & Co-existing disease, Stoelting 5th edition. p.345 |
|
|
139. In a patient with myasthenia gravis presenting for abdominal hysterectomy
A. anticholinesterase therapy will have an effect on her plasma cholinesterase B. epidural analgesia is contraindicated C. preoperative sedation should be used D. there is an increased sensitivity to suxamethonium E. volatile agents should not be used |
A
A. True – Anticholenesterases neostigmine and pyridostigmine but not edrophonium affect plasma cholinesterase - expect prolonged sux, miva, ester LA. B. False – Regional anaesthesia is a good alternative to post op opiods. C. False – Sedation should be avoided because of risks with bulbar palsy, resp fatigue. D. False – Decreased sensitivity to sux at NMJ due to decreased receptor numbers, need dose 1.5mg/kg, but with inhibition of PCE by regular meds, possibility of Phase 2 block. E. False – Volatiles OK. |
|
|
140. Correct statements regarding desmopressin (DDAVP) include each of the following EXCEPT
A. it improves platelet function in patients with liver disease B. it improves platelet function in patients with renal disease C. it is contraindicated in Type 1 von Willebrand's disease D. it is given in a dose of 0.3 micrograms.kg-1 intravenously E. it is used in the treatment of diabetes insipidus |
C
Product information for desmopressin: • Dose for DI is 1-4mcg/day (10-40mcg/day nasal). 0.3-0.4mcg/kg is for Haemophilia or vWD. • Indications: DI, Haemophilia A, vWD except IIB, platelet disorders • May induce platelet aggregation in vWD IIB • Congenital or acquired platelet disorders including uraemia, drug induced, CPB induced may respond. No evidence for platelet dysfunction of liver disease and use is not supported. |
|
|
141. Which of the following statements regarding pre-operative oral midazolam in children (in appropriate dosage) is INCORRECT?
A. Distress at induction is reduced by approximately one half B. Peak effect is at 20 - 30 minutes C. Pre-operative anxiety is reduced D. Post-operative maladaptive behaviour is reduced E. Significantly delays recovery and discharge |
E
Can J Anaesth. 2006 Dec;53(12):1213-1219 "Recovery times are not significantly delayed" |
|
|
142. Regarding venous air embolism (VAE) during posterior fossa neurosurgery
A. attempts to aspirate air from the caval-atrial junction are of little value B. children are at greater risk than adults C. Doppler ultrasonography is the most specific monitor available D. end-tidal nitrogen monitoring is the most sensitive monitor available E. positive end-expiratory pressure (PEEP) should be used in patients with intra-cardiac shunts |
A
A. True. Air has been successfully aspirated from the right ventricle via a percutaneously introduced needle or a central venous catheter in several experimental models and case reports. In general, however, these maneuvers are of limited benefit because the volume of air recovered is less than 20 mL - Uptodate B. Probably False - Different results from different studies. Sitting Position For Neurosurgery In Children: A Review Of 16 Years’ Experience - BJA 2002 88 (1): 12-17 C. False. TOE is the most sensitive, etN2 is most specific Sensitivity Specificity TOE 0.02ml/kg Not Absolute Precordial Doppler 0.2mg/kg Moderate End Tidal N2 0.1ml/kg Absolute D. False. Most specific. E. False. No evidence that it improves outcome and this may be dangerous as may increase R > L pressures > PAE. BJA 80 (1): 30 -35 |
|
|
143. Post dural puncture headaches (PDPH) in children
A. are less effectively treated by a blood patch (compared to adults) B. are rare in children under 10 years of age C. have an incidence of approximately 5% to 12% following spinal anaesthesia D. have an incidence which is independent of needle gauge E. presents with signs which are not posturally related |
B
A – False – Not enough data yet B – True C – True Paediatric Anaesthesia, Volume 12, Issue 6 (p 473-477) “The incidence of PDPH in children after LP is 2% to 15% and is said not to be age-dependent although it virtually never occurs in those <10 years of age.” Eur J Pediatr (2003) 162: 117–121 There is disagreement in the literature as to whether these figures are age related or not. Some studies have shown that PDPH only occurs in children aged more than 10 years. The incidence in studies (2,3) has varied from 10% (10–12 years) to 50% (13–18 years) following lumbar puncture.” D – false “The risk of PDPH is directly related to the diameter of the needle used.” Eur J Pediatr (2003) 162: E – False “always perform EBP if position dependent headache persists for 1 week” |
|
|
144. In maxillo-facial trauma
A. external soft tissue signs correlate with actual skeletal disruption B. Le Forte fractures rarely occur in combination (e.g. Le Forte 1 and 2) C. Le Forte 1 fractures should NOT be intubated nasally D. Le Forte 2 fractures require base of skull evaluation before nasal intubation E. Le Forte 3 fractures involve a fracture of the cribriform plate |
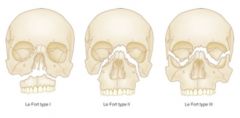
D
• A - wrong: gross oedema makes this difficult • B - wrong: Le Forte fractures are often mixed or in combination • C - wrong: Le Forte 2 & 3 involve base of skull • D - True. • E - False. May involve, but not always. Le Fort classification: I - Transverse fractures of the mid-lower maxilla II - Triangular fracture from top of the nose to the base of the maxilla III - Severe fractures with disruption of facial bones from the skull. Cribriform plate disruption and CSF leak common. In reality, the Le Fort classification is an oversimplification of maxillary fractures. In most instances, maxillary fractures are a combination of the various Le Fort types. Fracture lines often diverge from the described pathways and may result in mixed-type fractures, unilateral fractures, or other atypical fractures. In addition, in very high-energy blows, maxillary fractures may be associated with fractures to the mandible, cranium, or both (ie, panfacial). |
|
|
145. Correct statements regarding serotonin syndrome include each of the following EXCEPT
A. it may be caused by carbamazepine, pethidine or sumatriptan B. it is a clinical triad of cognitive changes, autonomic dysfunction and neuromuscular dysfunction C. the majority or reported cases occur with concommitant use of two or more serotinergic agents D. the mechanism consists of inhibition of serotonin uptake E. the symptoms usually have a slow onset over one week after a change in dose or drug |
E
A – true. all those drugs can cause it. B – true. typical triad described. C – true D – true. one of the mechanisms is inhibition of serotonin reuptake, but there are additional mechanisms as well – such as inhibition of serotonin breakdown by MAO, increased serotonin release or generation E - false. definitely see clinical features quite acutely over minutes to hours. |
|
|
146. Appropriate practice when performing central neuro-axial block should include all of the following EXCEPT
A. application of an alcohol based antiseptic that is allowed to dry B. donning gloves after removal of a watch C. wearing a firm fitting facemask D. thorough hand washing E. use of drugs in sterile packaging |
E
Drugs don’t necessarily need to be in sterile packaging as they can be cleaned with an alcohol swab. Benhamou D, Mercier FJ, Dounas M. Hospital policy for prevention of infection after neuraxial blocks in obstetrics. Int J Obstet Anesth 2002;11:265-269. Even though most regional anesthesia textbooks and articles about infectious complications associated with central neuraxial blocks underline the necessity of surgical asepsis, none offers a clear and precise procedure. This protocol is intended to reduce variability of practices, and is felt to be stringent enough to be effective and liberal enough to be fully implemented. Any person involved with the procedure must wear a cap and a new face mask. The patient also should wear a cap. The anesthesiologist, wearing his usual operating room clothing, must wash his hands with an antiseptic soap solution, dry them on a sterile towel and wear sterile gloves. The patient's back should be disinfected at least twice (alcohol–iodine, alcoholic solution of chlorhexidine or of povidone–iodine). Disposable equipment only must be used. Drugs must be prepared contemporaneously and in a sterile manner (collar of non-sterilized ampoules cleaned with alcohol). The solution is drawn up through the filter (contained in the epidural set) but injected after filter removal. Infusion of sterile mixtures is preferable to top-ups, which require frequent disconnections that may cause hub colonization. Manipulation of the hub of the catheter must be preceded both by antiseptic hand washing and by swabbing with sterilized gauze soaked with 70% alcohol. Catheter removal requires only antiseptic hand washing in most circumstances. Wearing mask and gloves and improving skin disinfection practices are believed to be the more important parts of this protocol |
|
|
147. The physiological change most likely to be associated with infra¬renal cross-clamping of the aorta is
A. decreased coronary blood flow B. decreased renal blood flow C. increased cardiac output D. increased heart rate E. reduction in myocardial wall motion abnormalities |
B
Miller p2073: Regardless of the position of the aortic cross-clamp, RBF is decreased to 50% of normal during surgical preparation of the aorta, presumably because of direct compression or reflex spasm of the renal arteries. After release of the suprarenal cross-clamp, RBF increases above normal (reflex hyperemia), but the GFR remains depressed to a third of control for up to 2 hours |
|
|
148. Features of anorexia nervosa include each of the following EXCEPT
A. dental caries B. increased gastric emptying C. mitral valve prolapse D. sinus bradycardia E. superficial parotitis |
B
MEDSCAPE In anorexia nervosa: CVS • Sinus brady usually • AV block, St depression, T wave inversion, Qt prolongation • Beware of arryhtmias under GA – 16-62% • Higher rate of MVP Resp • Metabolic acidosis - laxative abuse & vomiting • Asp pneumonia • Decreased compliance from starvation Renal • Proteinuria in >50% • Dec GFR • Hyponatraemia, hypokalaemia, hypochloraemia, hypomagnesaemia, and loss of hydrogen ions. • Hypocalcaemia due to decreased dietary intake may also occur Gastrointestinal • Salivary gland hyperplasia, dental caries, periodontis, oesophageal strictures, Mallory-Weiss tears, gastritis, and oesophagitis • Binge-eating patients may develop gastric dilatation and, in acute circumstances, gastric infarction or perforation • Strict dieting appears to prolong gastric emptying times • Abnormal LFT • 'Refeeding syndrome' Endocrine • Amenorrhoea - diagnostic criterion for anorexia nervosa • Menstruation ceases BMI< 15 • May sometimes display features of panhypopituitarism • Decreased T3/T4 Immunological and Haematological • Normal immune till weight < 50% of normal • anaemia is unusual • Anorexic patients also demonstrate raised cholesterol levels and hypercarotenaemia. Neurological • white (revesible) and grey (non-reversible) matter changes in the brain • coma and seizures may occur as a result of hypoglycaemia and electrolyte disturbances, • Mild neuropathies, fatigue, and generalized weakness common • Pain threshold may be raised in anorexics • loss of insulating adipose tissue, hypothermia • body temperatures of commonly < 36.3°C. Musculoskeletal • Generalized myalgia - hyponatraemia, hypokalaemia, and hypophosphataemia • muscle weakness • osteopenia and osteoporosis Investigations • FBE, U&E, CMP, LFT, BSL • Urinalysis – proteinuria • ECG • TTE Anaesthetic • weigh • NG for delayed emptying prior to induction • sodium citrate, ranitidine • RSI • Beware of positioning / pressure care • Avoid hypothermia • Neuromuscular blocking (hypokalaemia / hypocalcemia prolong effect) Hypoalbuminaemia is very common in anorexic patients. This must be considered when calculating drug dosages as a relative increase in the fraction of 'free' drug in the plasma will occur due to decreased protein binding. |
|
|
149. Signs of severe dehydration in an infant include each of the following EXCEPT
A. elevated pulse rate B. marked oliguria C. pale skin colour D. parched mucous membranes E. reduced blood pressure |
C
'Fluid and electrolyte management in children' Mary Cunliffe BJA CEPD Reviews Volume 3 Number 1 2003 - excellent table [1] From BJA review, ref below on assessment of dehydration Appearance: • Mild - Thirsty, restless, alert. • Moderate - Thirsty, restless or lethargic but rousable, pale (BP - Normal/low) • Severe - Drowsy to comatose, limp, cold, sweaty, grey, cyanosed ( BP - Low) |
|
|
150. Transient neurological symptoms (TNS) syndrome is characterised by pain and/or dysaesthesia in the buttocks or lower extremities following spinal anaesthesia. Clinical features of this syndrome include
A. a reduction in symptoms with lower doses of lignocaine B. a significantly decreased risk with 2% lignocaine compared to 5% lignocaine C. increased risk with early ambulation D. increased risk with prone positioning E. similar incidence with lignocaine and bupivacaine |
C
TRANSIENT NEUROLOGIC SYNDROME Transient Radicular Irritation • not associated with any detectable neurologic deficit • pain in the back, buttocks, and thighs mirrors the distribution of nerve damage in cauda equina syndrome sufficiently to support the theory that the nerves are indeed irritated by a noxious intrathecal injection. • Symptoms in 12 to 24 hrs - most often resolve in 3 days, and rarely persist beyond a week. • In addition to the use of intrathecal lidocaine, cofactors that contribute to the occurrence of TNS include the lithotomy position, positioning for knee arthroscopy, and outpatient status • No effect – LA concentration, the presence of glucose, Adr, and technique-related factors such as the size or type of needle do not alter the incidence of TNS. • risk factors for cauda equina syndrome and transient neurologic syndrome similar • Occurred after 2% as well as 5% lidocaine - bupivacaine is relatively blameless (near zero incidence) • Parturients may be at lower risk than other surgical patients Chestnut: Obstetric Anesthesia, 4th ed. Stoelting: Basics of Anesthesia, 5th ed. |
|
|
102. Tracheo-oesophageal Fistula (TOF)
A. is associated with cardiac anomalies in approximately 60% of cases B. is associated with oesophageal atresia in approximately 20% of cases C. is more common in males than females D. is usually left sided E. occurs in approximately 1 in 3500 live births |
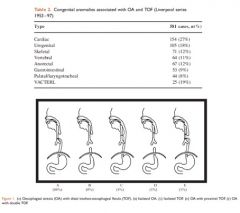
E
• A - False. From Stoelting AACD: "Approximately 20% of neonates with EA have major co-existing cardiovascular anomalies (ventricular septal defect, tetralogy of Fallot, coarctation of the aorta, atrial septal defect), and 30% to 40% are born before term." and from CEACCP- 27%: • B - False. Much higher. From CEACCP: "Approximately 4% of patients with TOF do not have OA." • C - False. 1:1 • D - False. Oesophagus is on the right • E - True. "TEFs are a common congenital anomaly with an incidence of 1 case in 2000-4000 live births" emedicine |

